Published online Mar 7, 2013. doi: 10.3748/wjg.v19.i9.1466
Revised: December 19, 2012
Accepted: January 11, 2013
Published online: March 7, 2013
Processing time: 130 Days and 6.9 Hours
AIM: To determine the mortality associated with functional bowel disorders (FBDs) and their possible relationship with organic bowel disease.
METHODS: Patients who satisfied the Rome III criteria for FBD (retrospective diagnosis) were followed up by telephone interview and/or outpatient review at 5 years after their first attendance. The patients were divided into the following groups: irritable bowel syndrome, functional abdominal bloating, functional constipation, functional diarrhea and unspecified FBD. The survival of the FBD patients overall and of those with each FBD were compared with data obtained from the Guangzhou population in 2005. The incidences of colonic cancer overall and for each FBD were compared with data from the Chinese population obtained from 56 cancer registries in 19 provinces of the country in 2008.
RESULTS: Two hundred and sixty-three patients were followed-up. Five patients died, which was not significantly different from the expected survival rate. No differences in mortality among the FBDs were found. There were nine cases of organic bowel disease: three colonic cancers and six colonic polyps. The incidence of colonic cancer in FBD patients was higher than that in the general Chinese population (0.23% vs 0.03%, P < 0.05). There were significant differences in the incidence of colonic cancer among the FBDs (0/134, 0/24, 2/29, 1/66, 0/10, respectively, P < 0.05); functional constipation was the most common. The incidence of colonic polyps was similar among the FBDs. The baseline age of patients who died was greater than that of those who survived (66.60 ± 6.84 years vs 45.14 ± 10.34 years, P < 0.05). The baseline age of patients who had colonic cancer or polyps during follow-up was greater than that of those without colonic cancer or polyps (60.33 ± 1.53 years vs 45.38 ± 10.62 years; 54.50 ± 6.47 years vs 45.34 ± 10.68 years, P < 0.05).
CONCLUSION: FBDs do not increase the risk of death. The incidence of colonic cancer in patients with FBDs may be increased, especially in those with functional constipation and in the elderly.
- Citation: Tang YR, Wang P, Yin R, Ge JX, Wang GP, Lin L. Five-year follow-up of 263 cases of functional bowel disorder. World J Gastroenterol 2013; 19(9): 1466-1471
- URL: https://www.wjgnet.com/1007-9327/full/v19/i9/1466.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i9.1466
Functional gastrointestinal disorders (FGIDs) are common in populations of various ethnicities and can seriously affect patients’ quality of life[1,2]. Functional bowel disorders (FBDs) are the most common FGIDs and include irritable bowel syndrome (IBS), functional abdominal bloating, functional constipation, functional diarrhea and unspecified functional bowel disorder[3,4]. FBDs are common in the Chinese population. Epidemiological investigations have found the prevalence of IBS to be 5.7% and 10.5% in Guangzhou and Beijing, respectively[5,6], IBS patients account for 11.3% of gastroenterology department outpatients[7], and the prevalence of functional constipation is about 3.0% in Guangzhou residents[8]. The extent and outcomes of FBD in the Chinese population are a cause of widespread concern.
FBDs are defined by symptom-based diagnostic criteria that combine chronic or recurrent symptoms attributable to the gastrointestinal (GI) tract in the absence of other, pathologically based disorders according to the Rome III criteria[3]. In recent years, technological advances and new research have revealed pathophysiologic changes in FBDs, including bowel motility disorder, visceral hypersensitivity, changes in the intestinal flora and psychologic abnormalities[9-13]. It has been thought that these do not affect patient survival, and a recent study reported that functional dyspepsia was not associated with increased mortality in the community, though the data for any effect of IBS on survival were less clear[14]. Research from Europe and the United States suggest that FBDs are closely related to certain organic bowel diseases; for example, functional constipation and colorectal cancer, or IBS and inflammatory bowel disease (IBD)[15-18]. However, such views are controversial.
No study has shown whether FBDs increase the risk of death or whether there is a link between FBDs and organic bowel disease in the Chinese population. In the present study, we followed up 263 outpatients with FBDs for 5 years to determine their survival and incidence of organic bowel disease.
As shown in Figure 1, data were collected from outpatients who attended the Department of Gastroenterology at Nanjing Jiangbei People’s Hospital between January, 2005 and December, 2006 and reported mainly bowel symptoms, such as abdominal pain or discomfort, bloating, swelling or abnormal bowel movements. Patients retrospectively diagnosed with FBD according to the Rome III criteria[3] and who agreed to follow-up were included in the study. All patients underwent routine blood, urine and stool hemoccult tests, stool form examination and endoscopy of the GI tract. Patients younger than 18 years or with a structural bowel disease or a history of abdominal surgery were excluded. Pregnant patients were not included. All patients included in the study were followed up in June, 2012.
Two hundred and sixty-three patients with FBDs were followed up for more than 5 years and their survival and incidence of organic bowel disease recorded.
Patient groups: Based on the Rome III diagnostic criteria, the patients were divided into the following groups: IBS, functional abdominal bloating, functional constipation, functional diarrhea and unspecified FBD[3].
Baseline data obtained: Baseline data for each subject were obtained from outpatient medical records, including age, gender, place of residence, and the duration and nature of symptoms.
Follow-up methods and content: All patients were followed up by telephone to ascertain: (1) survival (in the case of patients who had died, details of the cause and date of death were obtained); and (2) the presence of organic bowel disease and date of diagnosis. All surviving patients were asked to undergo review routine blood, urine and stool hemoccult tests, stool form examination, and endoscopy or radiographic examination of the GI tract.
All data were analyzed using SPSS version 19.0. Statistical significance was set at P < 0.05. Categorical data were analyzed using the χ2 test. All measurement data were reported as the mean ± SD and analyzed using the t test (between two groups) or one-way analysis of variance (among more than two groups). Kaplan-Meier estimates of overall survival observed vs expected for the whole cohort. Expected survival was based on the whole cohort using survival characteristics of the Guangzhou population from 2005[19]. The incidence of colonic cancer in FBD patients was compared with data from the Chinese population obtained from 56 cancer registries in 19 provinces of the country in 2008[20], using Fisher’s exact test. Survival and the incidence of colonic cancer and polyps in different age, gender and residence groups and in each FBD group were compared using Fisher’s exact test.
As shown in Figure 1, 312 patients were included in the study and 263 FBD patients were followed up; a dropout rate of 15.71%. At baseline, these patients were aged 20-74 years (45.55 ± 10.68 years) and comprised 128 (48.66%) males and 135 (51.33%) females. The duration of FBD ranged from 6 mo to 20 years, with a median duration of 1 year.
Clinical data for each FBD group are shown in Table 1. IBS was the most common FBD in these patients, followed by functional diarrhea, functional constipation, functional abdominal bloating and unspecified FBD. There were no differences in age, gender, place of residence (urban or rural) or duration of FBD between groups (all P > 0.05).
| FBD | n (%) | Age (yr)(mean ± SD) | Gender (F/M) | Residence (urban/rural) | Duration of FBD |
| IBS | 134 (47.1) | 45.44 ± 10.32 | 63/71 | 68/66 | 6 mo-20 yr |
| Functional abdominal bloating | 24 (9.1) | 43.17 ± 11.86 | 10/14 | 13/11 | 6 mo-17 yr |
| Functional constipation | 29 (11.0) | 46.59 ± 13.22 | 10/19 | 12/17 | 6 mo-20 yr |
| Functional diarrhea | 66 (25.1) | 46.56 ± 9.34 | 41/25 | 34/32 | 6 mo-20 yr |
| Unspecified FBD | 10 (3.8) | 41.90 ± 13.40 | 4/6 | 4/6 | 6 mo-10 yr |
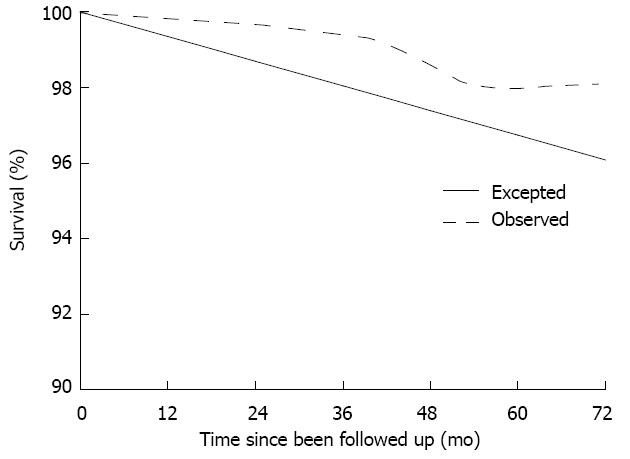
Survival: Five (1.90%) deaths had been reported in the cohort by the time of the last follow-up interview in June, 2012. Table 2 provides details of the deaths. The average age of the patients who died was greater at baseline than that of those who survived (66.60 ± 6.84 years vs 45.14 ± 10.34 years, t = 4.617, P < 0.01). There were no differences in mortality between genders or with place of residence (both P > 0.05). No differences of mortality in the various FBDs were found (P > 0.05). Expected survival was based on the whole cohort using survival characteristics of the Guangzhou population from 2005[19]. Overall observed vs expected survival for the whole set of respondents is illustrated in Figure 2; the data suggest there was no significant difference between observed and expected (P > 0.05).
| Details | n/N (%) |
| Age (yr), mean ± SD | |
| Baseline | 66.60 ± 6.84a |
| Death | 70.40 ± 5.86 |
| Gender | |
| Female | 2/135 (1.48) |
| Male | 3/128 (2.34) |
| Residence | |
| Urban | 3/133 (2.26) |
| Rural | 2/130 (1.54) |
| Cause of death | |
| Cardiovascular | 2 |
| Gastric cancer | 1 |
| Colonic cancer | 2 |
| Diagnosis at baseline | |
| IBS | 1/134 (0.75) |
| Functional abdominal bloating | 1/24 (4.17) |
| Functional constipation | 2/29 (6.90) |
| Functional diarrhea | 1/66 (1.52) |
| Unspecified FBD | 0/10 (0) |
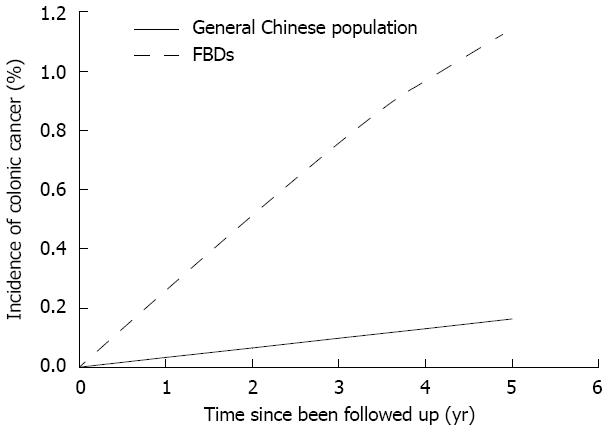
Detection of organic bowel disease: Organic bowel disease was detected in nine cases (3.42%): colonic cancer in three (1.14%) and colonic polyps in six (2.28%). Table 3 gives the details of the organic bowel diseases observed. The average age of patients with colonic cancer or colonic polyps was greater at baseline than that of the other patients (60.33 ± 1.53 years vs 45.38 ± 10.62 years, t = 13.582, P < 0.01; 54.50 ± 6.47 years vs 45.34 ± 10.68 years, t = 2.089, P < 0.05). There were no differences in the incidence of colonic cancer or polyps between genders or with place of residence (all P > 0.05). There were significant differences in the incidence of colonic cancer between the various FBDs (P < 0.05, Fisher’s exact test); the incidence was highest in the functional constipation group, being significantly higher than in the IBS group (P < 0.05, Fisher’s exact test), though not significantly different from the incidence in the other FBD groups (P > 0.05). The incidence of colonic polyps was similar between the various FBDs (P > 0.05). Compared with data from the general Chinese population obtained from 56 cancer registries in 19 provinces of the country, the incidence of colonic cancer was significantly increased in patients with FBDs (P < 0.01, Fisher’s exact test; Figure 3).
| Details | n/N (%) |
| Colonic cancer | |
| Age (yr), mean ± SD | |
| Baseline | 60.33 ± 1.53b |
| Cancer observed | 63.67 ± 2.08 |
| Gender | |
| Female | 1/135 (0.74) |
| Male | 2/128 (1.56) |
| Residence | |
| Urban | 2/133 (1.50) |
| Rural | 1/130 (0.77) |
| Diagnosis at baseline | |
| IBS | 0/134 (0) |
| Functional abdominal bloating | 0/24 (0) |
| Functional constipation | 2/29 (6.70)e |
| Functional diarrhea | 1/66 (1.52) |
| Unspecified FBD | 0/10 (0) |
| Colonic polyps | |
| Age (yr), mean ± SD | |
| Baseline | 54.50 ± 6.47c |
| Polyps observed | 57.83 ± 6.52 |
| Gender | |
| Female | 2/135 (1.48) |
| Male | 4/128 (3.13) |
| Residence | |
| Urban | 2/133 (1.50) |
| Rural | 4/130 (3.08) |
| Diagnosis at baseline | |
| IBS | 5/134 (3.62) |
| Functional abdominal bloating | 0/24 (0) |
| Functional constipation | 0/29 0() |
| Functional diarrhea | 1/66 (1.52) |
| Unspecified FBD | 0/10 (0) |
FBDs have long been considered a group of functional diseases in patients without any pathologically based disorder[3] that do not affect survival and are not associated with organic disease. Recent research from Europe and the United States, however, suggests that FBDs are closely related to certain organic bowel diseases - for example, functional constipation and colorectal cancer, or IBS and IBD[15-18] - and do have an effect on survival. No study has investigated the association between FBDs and organic bowel disease, or whether FBDs increase the risk of death, in the Chinese population. In the present study, we followed up 263 outpatients with FBDs for 5 years, revealing new information.
The mortality of the FBD patients was 1.90% over the 5-year follow-up period, equivalent to an average annual mortality of approximately 0.38%. A death spectrum and potential life lost investigation found a crude death rate of 652.3/100 000 (approximately 0.65%) in the Guangzhou population in 2005[19]. Compared with this population, our FBD patients showed no trend towards increased mortality. We can conclude that FBD does not increase the risk of death in Chinese patients. We found no differences in mortality among the various FBDs.
Data from 56 cancer registries in 19 provinces of China from 2008 shows the incidence of colorectal cancer to be 31.39/100 000 (approximately 0.03%) in the Chinese population[20]. In this study, three cases (1.14%) of colonic cancer were detected, equivalent to an average annual mortality of approximately 0.23%. The incidence of colonic cancer in patients with FBDs was thus significantly increased.
Significant differences in the incidence of colonic cancer were found between the FBDs; that of functional constipation was up to 6.70%, equivalent to an average annual incidence of approximately 1.34%. This was significantly higher than in the other FBDs, and also higher than in the general Chinese population (approximately 0.03%). A study based on the Japanese population suggests that the number of bowel movements is closely related to the incidence of colorectal cancer[21]. However, European and American studies have shown that constipation itself does not induce colorectal cancer, but use of cathartics (especially anthraquinones or phenolphthalein) may increase the incidence of both colorectal adenomas and colorectal cancer[22,23].
During the 5 years of follow-up in the present study, six cases (2.28%) of colonic polyps were observed. Several studies have reported the detection rate of colonic polyps in outpatients under colonoscopy, but no data are available regarding the annual incidence of colonic polyps in the Chinese population. Thus, we are unable to assess the risk of colon polyps in FBDs.
There were no differences in mortality or in the incidence of colonic polyps or cancer between genders or with place of residence. The average age at baseline of the patients who died during follow-up or who were found to have colonic cancer and polyps was greater than the average age at baseline of the patients who survived or did not have colonic cancer or polyps. We therefore suggest that the possibility of organic bowel disease should be considered in FBD patients over the age of 50 years, and that repeated review by colonoscopy is necessary after the diagnosis of FBD is established.
In conclusion, FBDs did not in general increase the risk of death assessed over 5 years in a Chinese population. Compared with the general population, the incidence of colonic cancer may be increased in FBD patients, especially those with functional constipation. These conclusions are based on the follow-up investigation of a small sample of FBD patients. A larger sample needs to be observed, control data should be collected from the general population over the same period, and a rigorous prospective study must be designed to verify our results.
Functional gastrointestinal disorders (FGIDs) are common in populations of various ethnicities and can severely affect patients’ quality of life. Functional bowel disorders (FBDs) are the most common FGIDs and are common in the Chinese population. The extent and outcomes of FBD in the Chinese population are a cause of widespread concern.
In recent years, research from Europe and the United States suggests that FBDs are closely related to certain organic bowel diseases; for example, functional constipation and colorectal cancer, or irritable bowel syndrome and inflammatory bowel disease. Whether FBDs increase the risk of death is controversial.
No study has shown whether FBDs increase the risk of death or whether there is a link between FBDs and organic bowel disease in the Chinese population. In the present study, authors followed up 263 outpatients with FBDs over 5 years to determine their survival and the incidence of organic bowel disease.
The study results suggest FBDs did not increase the risk of death over 5 years, though the incidence of colonic cancer in patients with FBDs may be increased, especially in those with functional constipation. The authors therefore suggest that the possibility of organic bowel disease should be considered in FBDs, especially in functional constipation, and repeated review by colonoscopy is necessary after the diagnosis of FBD is established.
FBDs are defined by symptom-based diagnostic criteria that combine chronic or recurrent symptoms attributable to the gastrointestinal tract in the absence of other, pathologically based disorders according to the Rome III criteria. FBDs are the most common functional gastrointestinal disorders and include irritable bowel syndrome, functional abdominal bloating, functional constipation, functional diarrhea and unspecified functional bowel disorder.
This is an interesting and well written manuscript examining the morbidity and mortality of FBDs in China. This has not really been examined before and is important to the extent that certain patients with FBDs may benefit from improved cancer surveillance. This manuscript describes a small, preliminary epidemiologic study of mortality and the development of organic bowel disease in Chinese patients diagnosed with functional bowel disorders over 5 years.
| 1. | Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119:654-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 541] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 2. | Simrén M, Svedlund J, Posserud I, Björnsson ES, Abrahamsson H. Health-related quality of life in patients attending a gastroenterology outpatient clinic: functional disorders versus organic diseases. Clin Gastroenterol Hepatol. 2006;4:187-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 85] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 3. | Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1467] [Cited by in RCA: 1493] [Article Influence: 74.7] [Reference Citation Analysis (1)] |
| 4. | Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3413] [Cited by in RCA: 3410] [Article Influence: 170.5] [Reference Citation Analysis (4)] |
| 5. | Xiong LS, Chen MH, Chen HX, Xu AG, Wang WA, Hu PJ. A population-based epidemiologic study of irritable bowel syndrome in Guangdong province. Zhonghua Yixue Zazhi. 2004;84:278-281. [PubMed] |
| 6. | Pan G, Lu S, Ke M, Han S, Guo H, Fang X. An epidemiologic study of irritable bowel syndrome in Beijing - a stratified randomized study by clustering sampling. Zhonghua Liuxingbingxue Zazhi. 2000;21:26-29. [PubMed] |
| 7. | Tang YR, Yang WW, Wang YL, Lin L. Sex differences in the symptoms and psychological factors that influence quality of life in patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2012;24:702-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Wei X, Chen M, Wang J. The epidemiology of irritable bowel syndrome and functional constipation of Guangzhou residents. Zhonghua Neike Zazhi. 2001;40:517-520. [PubMed] |
| 9. | Chen CL, Liu TT, Yi CH, Orr WC. Evidence for altered anorectal function in irritable bowel syndrome patients with sleep disturbance. Digestion. 2011;84:247-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Martínez C, Lobo B, Pigrau M, Ramos L, González-Castro AM, Alonso C, Guilarte M, Guilá M, de Torres I, Azpiroz F. Diarrhoea-predominant irritable bowel syndrome: an organic disorder with structural abnormalities in the jejunal epithelial barrier. Gut. 2012;May 25; Epub ahead of print. [PubMed] |
| 11. | Simrén M, Barbara G, Flint HJ, Spiegel BM, Spiller RC, Vanner S, Verdu EF, Whorwell PJ, Zoetendal EG. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. 2013;62:159-176. [PubMed] |
| 12. | Yu XZ, Liu HF, Sun ZX. Investigation of the effect of military stress on the prevalence of functional bowel disorders. World J Gastroenterol. 2012;18:3004-3007. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 13. | Hartono JL, Mahadeva S, Goh KL. Anxiety and depression in various functional gastrointestinal disorders: do differences exist? J Dig Dis. 2012;13:252-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Ford AC, Forman D, Bailey AG, Axon AT, Moayyedi P. Effect of dyspepsia on survival: a longitudinal 10-year follow-up study. Am J Gastroenterol. 2012;107:912-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Porter CK, Cash BD, Pimentel M, Akinseye A, Riddle MS. Risk of inflammatory bowel disease following a diagnosis of irritable bowel syndrome. BMC Gastroenterol. 2012;12:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Aguas M, Garrigues V, Bastida G, Nos P, Ortiz V, Fernandez A, Ponce J. Prevalence of irritable bowel syndrome (IBS) in first-degree relatives of patients with inflammatory bowel disease (IBD). J Crohns Colitis. 2011;5:227-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Chan AO, Hui WM, Leung G, Tong T, Hung IF, Chan P, Hsu A, But D, Wong BC, Lam SK. Patients with functional constipation do not have increased prevalence of colorectal cancer precursors. Gut. 2007;56:451-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (2)] |
| 18. | Chang JY, Locke GR, McNally MA, Halder SL, Schleck CD, Zinsmeister AR, Talley NJ. Impact of functional gastrointestinal disorders on survival in the community. Am J Gastroenterol. 2010;105:822-832. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 173] [Cited by in RCA: 175] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 19. | Tan XH, Zhang Y. Analysis of causes of death and potential years of life lost in 7 districts of Guangzhou. Nanfang Yike Daxue Xuebao. 2011;31:1075-1077. [PubMed] |
| 20. | Dai M, Ren JS, Li N, Li Q, Yang L, Chen YH. Estimation and prediction on cancer related incidence and mortality in China, 2008. Zhonghua Liuxingbingxue Zazhi. 2012;33:57-61. [PubMed] |
| 21. | Tashiro N, Budhathoki S, Ohnaka K, Toyomura K, Kono S, Ueki T, Tanaka M, Kakeji Y, Maehara Y, Okamura T. Constipation and colorectal cancer risk: the Fukuoka Colorectal Cancer Study. Asian Pac J Cancer Prev. 2011;12:2025-2030. [PubMed] |
| 22. | Simons CC, Schouten LJ, Weijenberg MP, Goldbohm RA, van den Brandt PA. Bowel movement and constipation frequencies and the risk of colorectal cancer among men in the Netherlands Cohort Study on Diet and Cancer. Am J Epidemiol. 2010;172:1404-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Dukas L, Platz EA, Colditz GA, Willet WC, Giovannucci EL. Bowel movement, use of laxatives and risk of colorectal adenomatous polyps among women (United States). Cancer Causes Control. 2000;11:907-914. [PubMed] |
P- Reviewers Johnston JM, Keefer L S- Editor Huang XZ L- Editor Logan S E- Editor Li JY