Published online Dec 28, 2013. doi: 10.3748/wjg.v19.i48.9485
Revised: November 5, 2013
Accepted: November 12, 2013
Published online: December 28, 2013
Processing time: 148 Days and 15.5 Hours
We report a case of hepatic choriocarcinoma in a man diagnosed at autopsy after a rapid downhill clinical course. The patient was a 49-year-old man who presented with acute right-sided abdominal pain. There were no masses palpable on physical examination. Radiographic findings showed large multi-nodular tumors mainly in the right lobe of the liver. Fludeoxyglucose-positron emission tomography scan showed uptake only in the liver, and no uptake in the testes. We initially planned to perform a liver resection for the presumed diagnosis of intra-hepatic cholangiocarcinoma. However, the tumors grew rapidly and ruptured. Multiple lung metastases rapidly developed resulting in respiratory failure, preventing liver resection or even biopsy. He died 60 d after initial presentation with no pathological diagnosis. Postmortem studies included histopathological and immunohistological examinations which diagnosed a primary choriocarcinoma of the liver. Primary hepatic choriocarcinoma is very rare but should be considered in the differential diagnosis of a liver tumor in a middle aged man. Establishing this diagnosis may enable treatment of the choriocarcinoma. Liver biopsy and evaluation of serum human chorionic gonadotropin are recommended in these patients.
Core tip: Evaluation of serum human chorionic gonadotropin levels in addition to other liver tumor markers should be performed in middle-aged men with undiagnosed hepatic tumors, to rule-out the possibility of primary hepatic choriocarcinoma. Liver biopsy is important to diagnose this rare and highly malignant tumor.
- Citation: Sekine R, Hyodo M, Kojima M, Meguro Y, Suzuki A, Yokoyama T, Lefor AT, Hirota N. Primary hepatic choriocarcinoma in a 49-year-old man: Report of a case. World J Gastroenterol 2013; 19(48): 9485-9489
- URL: https://www.wjgnet.com/1007-9327/full/v19/i48/9485.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i48.9485
Choriocarcinoma is a rare, aggressive, malignant germ-cell neoplasm of trophoblastic cells, which are among the first cells to differentiate from the fertilized egg to enable implantation. Choriocarcinoma is prone to rapid hematogenous metastases, and the first clinical manifestation is often metastatic lesions[1]. The characteristic laboratory finding in patients with choriocarcinoma is an elevated serum human chorionic gonadotropin (hCG) level. Choriocarcinoma is less common in men than women, and comprises only 1% of all germ-cell tumors, most often with the primary lesion in the testes[2]. There are only seven patients previously reported in the English literature with primary choriocarcinoma of the liver[3-5]. These patients have been reported from Asia, including Japan and China. We report here a 49-year-old Japanese male with primary choriocarcinoma of the liver diagnosed at autopsy, who presented initially with acute abdominal symptoms and a rapid downhill clinical course. Establishing the diagnosis early may enable treatment of choriocarcinoma. Consideration of this lesion in a patient with an undiagnosed liver mass is essential, necessitating evaluation of serum hCG level and urgent liver biopsy.
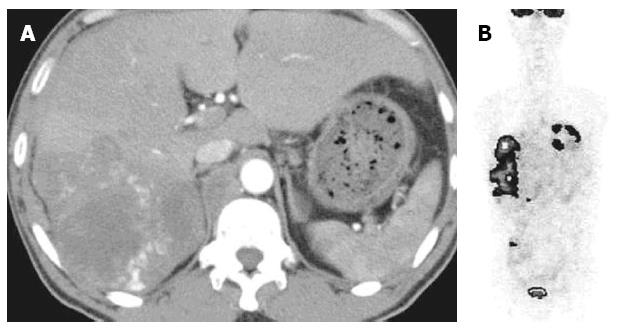
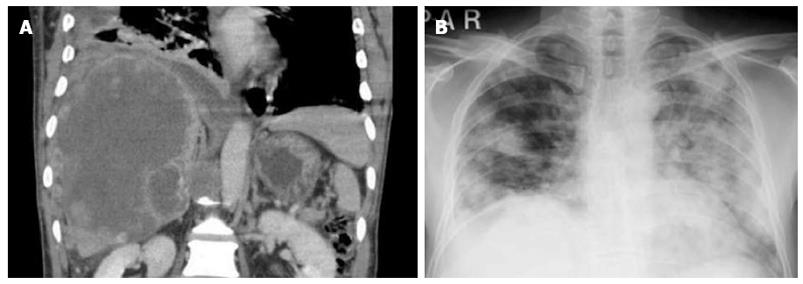
A 49-year-old male presented to the emergency room with acute right-sided abdominal pain and fever. He had a previous history of diabetes mellitus and hepatitis C. Physical examination was positive for abdominal tenderness. Contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI) scans revealed a multi-nodular hepatic tumor more than 10 cm in diameter in the right lobe (Figure 1A). Laboratory data showed white blood count (WBC) and liver function tests within normal limits but an elevated C-reactive protein to 8.75 mg/L. Serum carcinoembrionic antigen (CEA) was elevated to 18.5 ng/mL but α-fetoprotein (AFP) and CA19-9 were within normal limits. We suspected a metastatic liver tumor or intra-hepatic cholangiocarcinoma. Endoscopy found no primary lesion in the gastrointestinal tract and fludeoxyglucose-positron emission tomography (FDG-PET) scan showed abnormal uptake only in the liver (Figure 1B). We planned to perform liver resection with a presumptive diagnosis of intra-hepatic cholangiocarcinoma but avoided performing a liver biopsy due to the risk of dissemination. Before he could undergo liver resection, the tumors grew rapidly and ruptured (Figure 2A). Multiple lung metastases rapidly developed, accompanied by severe respiratory failure (Figure 2B). Due to pulmonary, biopsy or resection of the liver were not possible and the patient died 60 d after initial presentation.
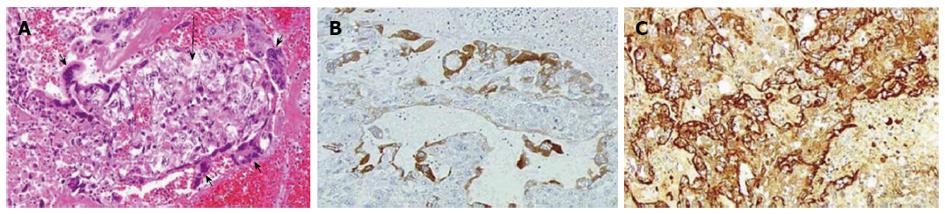
At autopsy, the liver weighed 4080 g with numerous hemorrhagic satellite nodules in the right lobe. There were multiple hemorrhagic lung nodules up to 3 cm in diameter, and microscopic metastases were identified in other viscera, including a para-aortic lymph node, the right adrenal gland, peritoneum, right renal capsule, and spleen. There was no malignant change or scar in the testes. Histological findings of the hepatic tumors showed choriocarcinoma with a biphasic pattern of mononuclear cytotrophoblasts and giant multi-nucleated syncytiotrophoblast cells (Figure 3A).
Immunohistochemistry was positive for an antibody to hCG subunits α (Figure 3B) and β (Figure 3C). Control tissue slides of placental chorionic villi stained with the same antibody showed staining limited to the syncytiotrophoblast layer. The syncytiotrophoblast cells in the liver were strongly positive for hCG, as were those in the other organs involved. Serum hCG was evaluated post-mortem, significantly elevated at 53000 IU/mL.
Choriocarcinoma is an uncommon, aggressive trophoblastic malignant neoplasm that is prone to early hematogenous metastases. It typically presents as a primary tumor of the uterus or genital tract in gestational females. In males the primary lesion is usually in the testes, but represents only 1% of all testicular tumors[2]. Extra-genital choriocarcinomas are less common, and often exist with other carcinomas, tending to occur in mid-line organs[1]. Pure extra-genital non-midline choriocarcinomas are the least common type. Only seven previous male patients with choriocarcinoma of the liver have been reported in the English language literature (Table 1)[3-5]. Hepatic choriocarcinoma has been recognized as a primary malignant tumor of the liver since 1992 when first reported by Fernández Alonso et al[3]. The other patients were reported from Asia (China and Japan), with a majority from China[4,5].
The patient in this report presented with acute abdominal symptoms and a multi-nodular tumor in the right lobe of the liver. Based on radiographic appearance, an elevated serum CEA and the absence of a lesion in the gastrointestinal tract, the leading diagnosis was intra-hepatic cholangiocarcinoma. FDG-PET scan showed no other lesions, including the testes. Based on these findings, a liver resection was planned in this patient. FDG-PET scan has been reported previously in the diagnosis of choriocarcinoma[6,7]. Furthermore, FDG-PET scan is also useful to evaluate the efficacy of treatment of liver lesions such as surgery or chemotherapy[6].
In the differential diagnosis of malignant liver tumors in a patient presenting with an acute abdomen, sarcomatous changes from hepatocellular carcinoma or cholangiocarcinoma must be considered. Both of these tumors can have a rapid clinical course and generally have poor outcomes. Sarcomatous change in primary liver tumors has been reported from Asian countries as well as choriocarcinoma[8-10]. Sarcomatous changes are seen in about 2%-4% of patients with resected hepatocellular carcinoma. Patients with sarcomatous changes have a worse prognosis than that in patients with typical hepatic lesions. More than half of the patients with sarcomatous changes died within a year of resection[8].
The characteristic laboratory finding in choriocarcinoma is an elevated hCG level in the blood or urine. This patient had an elevated serum hCG level in a post-mortem blood sample. In male patients, there are few reasons to evaluate serum hCG levels except in patients with testicular tumors[11-13]. When we evaluate a middle aged patient with an aggressive liver tumor, we recommend checking serum hCG as tumor marker in addition to AFP, CEA and CA19-9.
The strategy for choriocarcinoma of the liver is not established because of its rarity and highly malignant behavior. We believe that urgent liver resection before manifestation of distant metastases and chemotherapy may be the best course for prolongation of survival. In a patient with gastric choriocarcinoma and multiple liver metastases, Waseda et al[14] reported pathological complete response using etoposide and cisplatinum, with a two year disease-free survival after surgical resection. Methotrexate and actinomycin D may also be important agents in the treatment of choriocarcinoma. The use of cyclophosphamide, etoposide and vincristine have also been reported. Cisplatinum and 5-FU were used in other reports. Shi et al[5] reported five patients with hepatic choriocarcinoma. Two of the five patients underwent liver resection with adjuvant chemotherapy, and three of the five patients with distant metastases were treated with chemotherapy after needle biopsy. The two patients who underwent resection survived only six and eight months respectively, despite having received adjuvant chemotherapy. Of the three other patients reported, two were diagnosed with undifferentiated carcinoma and one with metastatic choriocarcinoma by needle biopsy. These patients underwent chemotherapy including 5-FU and platinum, but all died within five months.
Liver biopsy was not performed in the present patient because the diagnosis of intra-hepatic cholangiocarcinoma was suspected, and biopsy could result in an increased risk of tumor dissemination. His condition rapidly deteriorated due to respiratory failure, which precluded the safe conduct of any invasive procedures. The diagnostic accuracy of needle or aspiration biopsy is not adequate, and may lead to an incorrect diagnosis of poorly differentiated carcinoma because of the similarity to cytotrophoblasts. The accuracy of liver biopsy is still controversial in establishing the diagnosis of choriocarcinoma. However, in order to enable rapid treatment of such an aggressive tumor, liver biopsy should be performed without hesitation.
In a middle-aged male patient with an aggressive liver tumor, evaluation of serum hCG levels in addition to other liver tumor markers should be performed. Liver biopsy is important, especially in Chinese and Japanese patients, to detect this rare and highly malignant tumor.
Written informed consent was obtained from the patient’s younger brother for publication of this report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Acute abdominal pain and fever in a 49-year-old man.
Primary hepatic choriocarcinoma.
Sarcomatous changes from hepatocellular carcinoma or cholangiocarcinoma.
Elevated hCG in blood or urine is definitive.
Multi-nodular liver tumor with uptake by FDG-PET.
Liver biopsy with immunohistochemistry is recommended.
Urgent surgical resection and chemotherapy is recommended.
Hepatic choriocarcinoma in a middle-aged male is the least common.
In a middle-aged male with an aggressive liver tumor, evaluation of serum hCG levels and liver biopsy should be performed.
The study reported a case of a patient suffering primary hepatic choriocarcinoma, which is a kind of very rare, especially in men, and malignant trophoblastic cancer. The description of this case is very interesting for the detection and differentiation of this type of aggressive tumour among other primary liver cancers and the conclusions are enlightening for the clinical management of these patients.
| 1. | Fine G, Smith RW, Pachter MR. Primary extragenital choriocarcinoma in the male subject. Case report and review of the literature. Am J Med. 1962;32:776-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 117] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Scholz M, Zehender M, Thalmann GN, Borner M, Thöni H, Studer UE. Extragonadal retroperitoneal germ cell tumor: evidence of origin in the testis. Ann Oncol. 2002;13:121-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 89] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Fernández Alonso J, Sáez C, Pérez P, Montaño A, Japón MA. Primary pure choriocarcinoma of the liver. Pathol Res Pract. 1992;188:375-37; discussion 375-37;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Arai M, Oka K, Nihei T, Hirota K, Kawano H, Kawasaki T, Hakozaki H. Primary hepatic choriocarcinoma--a case report. Hepatogastroenterology. 2001;48:424-426. [PubMed] |
| 5. | Shi H, Cao D, Wei L, Sun L, Guo A. Primary choriocarcinoma of the liver: a clinicopathological study of five cases in males. Virchows Arch. 2010;456:65-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Cimarelli S, Deshayes E, Mognetti T, Biron P, Desuzinges C, Rivoire M, Giammarile F. F-18 FDG PET/CT imaging in a case of primary choriocarcinoma in the retroperitoneum. Clin Nucl Med. 2009;34:449-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Sanchez D, Zudaire JJ, Fernandez JM, Lopez J, Arocena J, Sanz G, Gimenez M, Rosell D, Robles JE, Berian JM. 18F-fluoro-2-deoxyglucose-positron emission tomography in the evaluation of nonseminomatous germ cell tumours at relapse. BJU Int. 2002;89:912-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Maeda T, Adachi E, Kajiyama K, Takenaka K, Sugimachi K, Tsuneyoshi M. Spindle cell hepatocellular carcinoma. A clinicopathologic and immunohistochemical analysis of 15 cases. Cancer. 1996;77:51-57. [PubMed] |
| 9. | Kakizoe S, Kojiro M, Nakashima T. Hepatocellular carcinoma with sarcomatous change. Clinicopathologic and immunohistochemical studies of 14 autopsy cases. Cancer. 1987;59:310-316. [PubMed] |
| 10. | Inagaki Y, Sugimoto K, Shiraki K, Yoshizawa N, Tameda M, Ogura S, Yoneda M, Takei Y, Fuke H, Hashimoto A. Sarcomatous hepatocellular carcinoma with remittent fever. Intern Med. 2012;51:3025-3029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Nakanuma Y, Unoura M, Noto H, Ohta G. Human chorionic gonadotropin in primary liver carcinoma in adults. An immunohistochemical study. Virchows Arch A Pathol Anat Histopathol. 1986;409:365-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Braunstein GD, Vogel CL, Vaitukaitis JL, Ross GT. Ectopic production of human chorionic gonadotropin in Ugandan patients with hepatocellular carcinoma. Cancer. 1973;32:223-226. [PubMed] |
| 13. | Nonomura A, Mizukami Y, Matsubara F, Izumi R, Nakanuma Y, Hayashi M, Watanabe K, Takayanagi N. Human chorionic gonadotropin and alpha-fetoprotein in cholangiocarcinoma in relation to the expression of ras p21: an immunohistochemical study. Liver. 1989;9:205-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Waseda Y, Komai Y, Yano A, Fujii Y, Noguchi N, Kihara K. Pathological complete response and two-year disease-free survival in a primary gastric choriocarcinoma patient with advanced liver metastases treated with germ cell tumor-based chemotherapy: a case report. Jpn J Clin Oncol. 2012;42:1197-1201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
P- Reviewer: Romero MR S- Editor: Wen LL L- Editor: A E- Editor: Zhang DN