Published online Nov 21, 2013. doi: 10.3748/wjg.v19.i43.7772
Revised: September 24, 2013
Accepted: September 29, 2013
Published online: November 21, 2013
Processing time: 84 Days and 13.7 Hours
AIM: To investigate the pathogenesis of biliary casts after liver transplantation relative to their morphology and biochemical markers.
METHODS: The microstructure of biliary casts was assessed using scanning electron microscopy and Hematoxylin and eosin staining assessed their histology. The expression levels of CD3, CD5, CD34, CD68 and CD79a in these biliary casts were evaluated immunohistochemically.
RESULTS: Biliary casts differed widely in their microstructure, with some containing blood vessels positive for CD34 and collagen fibers with positive Masson staining. Large numbers of neutrophils and other inflammatory cells were present, but only on the edge of the biliary casts; although the boundaries were clear without crossover. None of the biliary casts contained T-lymphocytes, B-lymphocytes, macrophages and other inflammatory cells.
CONCLUSION: The microcostructure of biliary casts differed. Bacteria and acute rejection are not clearly related to their formation.
Core tip: This experimental study employed scanning electron microscopy, Hematoxylin and eosin staining and immunohistochemistry to investigate biliary casts following liver transplantation. The results indicated that blood vessels and collagen fibers are present in biliary casts; however, bacteria and acute rejection are not clearly related to their formation, as evidenced by blood vessels positive for CD34 and collagen fibers with positive Masson staining, and no T-lymphocytes, B-lymphocytes, macrophages and other inflammatory cells. Thus, although bile duct injury after liver transplantation is significantly associated with biliary cast formation, their role in acute rejection is unclear.
- Citation: Yang YL, Zhang C, Lin MJ, Shi LJ, Zhang HW, Li JY, Yu Q. Biliary casts after liver transplantation: Morphology and biochemical analysis. World J Gastroenterol 2013; 19(43): 7772-7777
- URL: https://www.wjgnet.com/1007-9327/full/v19/i43/7772.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i43.7772
Despite advances in the management of patients who have undergone cadaveric liver transplantation, 6%-34% patients experience biliary complications[1]. Biliary cast syndrome (BCS), first described in 1975[2], occurs less frequently than biliary sludge and stones, with an incidence of 2.5% after orthotopic liver transplantation[3]. Multiple intrahepatic biliary strictures, ductal dilatation, intrahepatic abscesses, and biliary anastomotic leakage characterize BCS. The clinical symptoms of BCS usually include high fever, jaundice and cholestatic liver enzyme elevation, similar to the symptoms observed in some patients with intrahepatic bile duct stones. Surgical management is the treatment of choice, and endoscopic techniques have been successful and safe in the removal of biliary casts[4-6]. Morphologically, biliary casts are a similar shape to bile ducts, appearing as a hardened, dark material in the biliary ductal system. Biliary casts can prevent bile drainage, resulting in biliary obstruction and inducing biliary tract infection. Biliary casts can ultimately cause substantial injury to the liver, with some transplant recipients requiring retransplantation. Although the associations between biliary casts and clinical treatment have been assessed recently, less is known about the associations between biliary casts and biochemical markers. We therefore investigated the pathogenesis of biliary casts after liver transplantation relative to their morphology and biochemical markers.
We evaluated 15 patients with a history of orthotopic liver transplantation, who were treated in our department for jaundice, recurrent cholangitis and high fever. There were 10 males and 5 females, with a mean age of 52.1 years (range, 34-78 years). Of these patients, five underwent deceased donor liver transplantation for hepatitis B-induced cirrhosis and primary liver cancer, one for primary hepatocellular carcinoma and nine for cirrhosis during the decompensated period. Choledochoscopy and duodenoscopy have been used frequently to assess patients with biliary complications after liver transplantation[7,8]. Patients with T-tube fistulae can be evaluated by insertion of a cholangioscope directly into the common hepatic duct, whereas patients without T-tube fistulae are evaluated preferably by percutaneous transhepatic cholangioscopy or endoscopic retrograde cholangiopancreatography[9]. The distal aspect of the cast was secured using a basket, allowing each cast to be successfully removed as a single piece. All the casts were stored in liquid nitrogen.
Following their isolation, biliary casts that were kept at room temperature were rinsed in sterile normal saline solution, fixed with 10% neutral formalin for 12 h at 4 °C, rinsed in 0.1 mol/L phosphate buffer (pH 7.0) and dehydrated through a graded series of ethanol (10 min each at 10%, 30%, 50%, 70% and 90%, and 15 min each three times at 100%). After critical point drying at 30 °C with CO2 for 6 h, the samples were mounted, coated with 1-μm gold particles and evaluated using a Hitachi S 4800 field emission scanning electron microscope at 2 kV.
Biliary casts stored in liquid nitrogen were rinsed in sterile normal saline solution, fixed with 10% neutral formalin for 12 h at 4 °C, embedded in paraffin, cross-sectioned into 10 mm slices and placed onto glass slides. Some of these histological sections were stained with hematoxylin and eosin (HE) and Masson trichrome, according to standard procedures. The remaining histological sections were deparaffinized, rehydrated, incubated in 3% hydrogen peroxide/absolute methanol for 5 min to block endogenous peroxidase activity and rinsed in distilled water. Nonspecific binding of antibodies was blocked by incubation with 5% normal goat serum for 10 min at room temperature. After washing, the sections were incubated with primary rabbit antibodies against human CD3, CD5, CD34, CD68 and CD79a, overnight at 4 °C. The sections were subsequently incubated with biotinylated secondary antibody for 30 min at 37 °C, with streptavidin biotin complex reagent for 30 min at 37 °C, and with DAB Plus reagent for 10 min, with the sections repeatedly washed with PBS, pH 7.4, between incubations. The sections were counterstained with hematoxylin, mounted and examined by optical microscopy. All antibodies and reagents for immunohistochemistry were purchased from the Beijing Zhongshan Golden Bridge Biotechnology Company, Beijing, China.
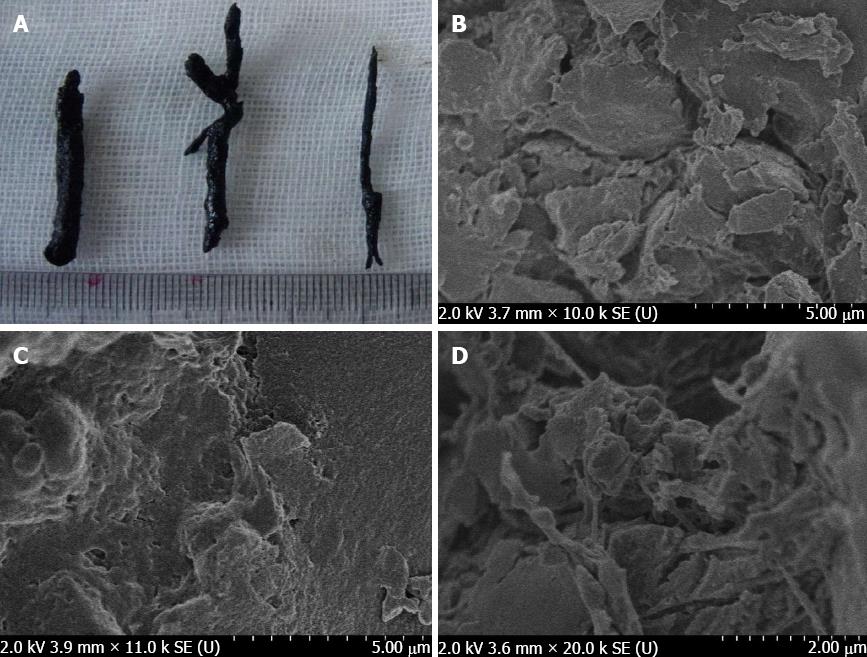
Morphologically, biliary casts have a cordlike, columnar, dendritic shape within the biliary ductal system (Figure 1A). Scanning electron microscopy, however, showed that biliary casts were present in a variety of forms: irregular sheets composed of imbricated accumulations (Figure 1B); honeycombs with porous structures and adherent crystalline substances (Figure 1C); and filamentous structures (Figure 1D).
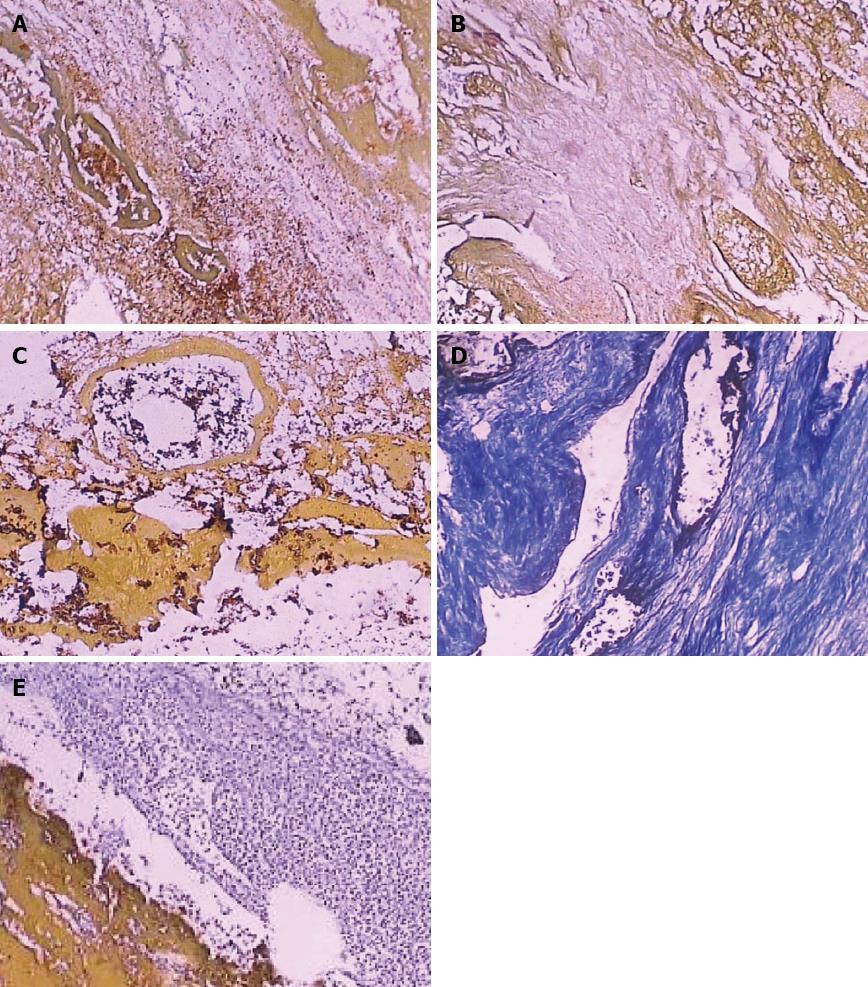
HE staining revealed large numbers of lacunae containing bilirubin, tubiform (Figure 2A) and filamentous structures (Figure 2B). To determine the composition of the tubiform and filamentous structures, we incubated these sections with antibodies to cell markers and with Masson stain. We found that the tubiform structures were positive for CD34 (Figure 2C), whereas the filamentous structures were positive for Masson stain (Figure 2D). These findings indicated that the tubiform structures were blood vessels and the filamentous structures were collagen fibers.
HE staining showed large numbers of neutrophils and other inflammatory cells on the edge of the biliary casts; however, the boundaries were clear without crossover, and no inflammatory cells were present within the biliary casts (Figure 2E). Scanning electron microscopy showed no evidence of bacteria or bacterial debris on the surface of the biliary casts.
Acute rejection generally occurs 1 to 3 wk after liver transplantation. To determine the relationship between immune rejection reactions and biliary cast formation, we incubated the biliary cast samples with antibodies to CD3, CD5, CD68, and CD79a. None of the biliary casts was positive for any of these markers, indicating that these biliary casts did not contain T-lymphocytes, B-lymphocytes and macrophages.
Physically and morphologically, biliary casts appear as dark, hardened material in the shape of bile ducts within the biliary ductal system, but differ from bile duct stones. Scanning electron microscopy showed that biliary casts appear in a variety of forms, including irregular sheets composed of imbricated accumulations; honeycombs with a porous structure and adherent crystalline substances; and filamentous structures. Although bile duct stones and biliary casts have a similar microstructure[10], their mechanism of formation differs significantly. Biliary casts that form after liver transplantation are not caused by a single pathogenic factor, but may be associated with late functional rehabilitation, biliary strictures and obstruction, acute rejection, recurrent cholangitis, cold and warm ischemia times, hepatic ischemia and reperfusion injury[3,11-13].
Bilirubin has been reported to be the primary component of biliary casts (approximately 10%-50%), followed by bile acid synthesis products and cholesterol, with protein comprising only 5%-10%[14]. In comparison, we observed large amounts of bilirubin, as well as blood vessels and collagen fibers, consistent with our earlier findings. Choledochoscopy showed a large number of flocs in bile duct cellulose 5 mo after transplantation, with histopathological examination showing that these flocs were composed of cellulose, bile duct epithelial cells and necrotic inflammatory cells. These elements then become structureless, with biliary casts observed in the bile ducts 9 mo after transplantation[15]. The presence of blood vessels and collagen fibers in the biliary casts was related to injury to the bile duct mucosa. The extent of bile duct injury during orthotopic liver transplantation differs, with cold preservation/reperfusion injury being the most important initiator of bile duct tree injuries and vessel plexus damage. Bile duct injury may, therefore, be associated with microcirculatory disturbances surrounding the bile ducts[16]; however, the specific mechanisms underlying bile duct injury require further investigation.
Acute rejection after liver transplantation generally occurs 1 to 3 wk postoperatively. Typical clinical symptoms include unexplained fever, loss of appetite, poor spirit, liver pain, progressively deepening jaundice, and elevated bilirubin and transaminase. The diagnosis mainly depends on liver puncture biopsy and pathology. Biliary casts and acute rejection after transplantation have a similar time of onset and similar clinical symptoms. However, biliary casts generally form at least 1 mo after transplantation[17]. Liver recipients with high serum concentrations of soluble major histocompatibility complex class I related chain A (sMICA) tend to develop BCS more easily than recipients with normal post-transplant sMICA concentrations[18]. We hypothesized that the formation of biliary casts was related to acute rejection and that T lymphocytes, B lymphocytes and macrophages would be present in biliary casts. However, we found that these cells were absent from biliary casts arising after liver transplantation, similar to the findings in patients who underwent non-liver transplantation[19,20]. Therefore, our findings suggest that acute rejection after liver transplantation was not significantly associated with biliary cast formation.
Electron microscopic examination of cholesterol calculi showed the presence of bacteria in the core and periphery of cholesterol stones, suggesting that bacteria may be involved in initiating the formation of cholesterol stones[21,22]. Patients with biliary casts usually have recurrent episodes of cholangitis. Escherichia coli, which has glucuronidase activity and can grow in cultures of biliary casts, can degrade conjugated bile acids and conjugated bilirubin, yielding free bile acids and free bilirubin, respectively. Free bile acids and free bilirubin are relatively insoluble and are not present in the bile of patients. Damage to the bile duct mucosa can result in their precipitation into biliary casts, suggesting that a number of factors, including infection, supersaturation with cholesterol and mucosal damage, may be involved in bile cast formation after liver transplantation[2]. To assess the relationship between bacteria and biliary casts, we evaluated biliary casts using scanning electron microscopy. However, neither bacteria nor bacterial debris was observed in the interior or surface of biliary casts. Large numbers of neutrophils were observed on the periphery of biliary casts, but the boundaries were clear and there were no neutrophils or similar cells within the mold. The multiplication of bacteria in an environment of poor bile drainage and cholestasis caused by biliary casts may therefore induce recurrent fever, obstructive jaundice and other complications. Biliary tract infections may be secondary pathological changes following biliary cast formation, rather than being the direct cause of mold formation. Therefore, when treating patients who experience complications after liver transplantation, anti-infectious agents may only alleviate the symptoms. The removal of the biliary casts may therefore be primary.
Biliary casts are infrequent complications after liver transplantation, resulting in various clinical symptoms. Although the associations between biliary casts and clinical treatment have been assessed recently, less is known about the associations between biliary casts and biochemical markers.
The current pathogenesis study of biliary casts after liver transplantation mostly concentrated on clinical aspects. Biliary casts were not caused by a single pathogenic factor, but may be associated with late functional rehabilitation, biliary strictures and obstruction, acute rejection, recurrent cholangitis, cold and warm ischemia times, hepatic ischemia and reperfusion injury.
The results indicated that blood vessels and collagen fibers are present in biliary casts; however, bacteria and acute rejection are not clearly related to their formation, as evidenced by blood vessels positive for CD34 and collagen fibers with positive Masson staining, and the absence of T-lymphocytes, B-lymphocytes, macrophages and other inflammatory cells.
These findings indicate that bile duct injury is clearly associated with biliary cast formation after liver transplantation; however, bacteria and acute rejection were not significantly related to their formation.
Biliary cast syndrome, first described in 1975, occurs less frequently than biliary sludge and stones, with an incidence of 2.5% after orthotopic liver transplantation. Orthotopic liver transplantation refers to a procedure in which a failed liver is removed from the patient’s body and a healthy donor liver is transplanted into the same location. Biliary casts are infrequent complications after liver transplantation, resulting in various clinical symptoms.
The authors analyzed the pathogenesis of biliary casts after liver transplantation relative to their morphology and biochemical markers. These findings indicate that bile duct injury was clearly associated with biliary cast formation after liver transplantation, but that bacteria and acute rejection are not clearly related to their process of bile duct injury. Therefore, it is an interesting study. The analytical approaches are described in detail, and the results are impressive.
| 1. | Bak SH, Choi HS, Yang SY, Jun DW, Han SH, Lee HL, Lee OY, Yoon BC, Hahm JS, Lee MH. [Obstructive jaundice due to biliary cast syndrome followed by orthotopic liver transplantation]. Korean J Gastroenterol. 2006;48:119-123. [PubMed] |
| 2. | Waldram R, Williams R, Calne RY. Bile composition and bile cast formation after transplantation of the liver in man. Transplantation. 1975;19:382-387. [PubMed] |
| 3. | Gor NV, Levy RM, Ahn J, Kogan D, Dodson SF, Cohen SM. Biliary cast syndrome following liver transplantation: Predictive factors and clinical outcomes. Liver Transpl. 2008;14:1466-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Navaneethan U, Venkatesh PG, Al Mohajer M, Gelrud A. Successful diagnosis and management of biliary cast syndrome in a liver transplant patient using single operator cholangioscopy. JOP. 2011;12:461-463. [PubMed] |
| 5. | Saleem A, Baron TH. Successful endoscopic treatment of biliary cast syndrome in an orthotopic liver transplant patient with a Roux-en-Y anastomosis via balloon enteroscopy. Liver Transpl. 2010;16:527-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Srinivasaiah N, Reddy MS, Balupuri S, Talbot D, Jaques B, Manas D. Biliary cast syndrome: literature review and a single centre experience in liver transplant recipients. Hepatobiliary Pancreat Dis Int. 2008;7:300-303. [PubMed] |
| 7. | Barritt AS, Miller CB, Hayashi PH, Dellon ES. Effect of ERCP utilization and biliary complications on post-liver-transplantation mortality and graft survival. Dig Dis Sci. 2010;55:3602-3609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Yang Yl, Fu QL, Tan WX, Liu XB, Feng QS, Zhang BS. Diagnosis and treatment of 6 patients with biliary complications following orthotopic liver transplantation by choledochofiberscopy. Zhonghua Qiguan Yizhi Zazhi. 2005;26:561-563. [DOI] [Full Text] |
| 9. | Yu Q, Yang YL, Lin MJ, Zhang HW, Shi LJ, Li JY, Zhang C. The therapeutic value of percutaneous transhepatic cholangioscopy for biliary cast after liver transplantation. Zhonghua Xiaohua Neijing Zazhi. 2011;28:146-149. [DOI] [Full Text] |
| 10. | Yu Q, Yang YL, Lin MJ, Zhang HW, Shi LJ. A Comparative Study of liver transplantation biliary cast and morphology of bile duct stones. Zhonghua Waike Zazhi. 2011;49:650-651. [DOI] [Full Text] |
| 11. | Starzl TE, Putnam CW, Hansbrough JF, Porter KA, Reid HA. Biliary complications after liver transplantation: with special reference to the biliary cast syndrome and techniques of secondary duct repair. Surgery. 1977;81:212-221. [PubMed] |
| 12. | Sawyer RG, Punch JD. Incidence and management of biliary complications after 291 liver transplants following the introduction of transcystic stenting. Transplantation. 1998;66:1201-1207. [PubMed] |
| 13. | Sheng R, Ramirez CB, Zajko AB, Campbell WL. Biliary stones and sludge in liver transplant patients: a 13-year experience. Radiology. 1996;198:243-247. [PubMed] |
| 14. | Shah JN, Haigh WG, Lee SP, Lucey MR, Brensinger CM, Kochman ML, Long WB, Olthoff K, Shaked A, Ginsberg GG. Biliary casts after orthotopic liver transplantation: clinical factors, treatment, biochemical analysis. Am J Gastroenterol. 2003;98:1861-1867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Yang YL, Fu WL, Liu XB, Tan WX, Zhang BS, Feng QS. Diagnosis and treatment of biliary stone by choledochofibroscope after orthotopic liver transplantation. Zhonghua Gandan Waike Zazhi. 2005;11:528-529. [DOI] [Full Text] |
| 16. | Tan WX, Yang YL, Wang XG, Fu WL. Pathological changes of bile duct injury after orthotopic liver transplantation. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2008;12:10583-10587. |
| 17. | Yang YL, Liu ZW, Lin MJ, Zhang HW, Shi LJ. Analysis of liver function test and screening of early warning indicators for biliary cast group after orthotopic liver transplantation. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2011;15:5707-5712. [DOI] [Full Text] |
| 18. | Zou Y, Yang X, Jiang X, Wang H, Hao Q, Liu Y, Yu P. High levels of soluble Major Histocompatibility Complex class I related chain A (MICA) are associated with biliary cast syndrome after liver transplantation. Transpl Immunol. 2009;21:210-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Zimmer V, Raedle J, Treiber G, Lammert F. Biliary cast syndrome in sclerosing cholangitis. Dig Liver Dis. 2011;43:e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Gleeson FC, Czaja AJ, Baron TH. Successful endoscopic management of biliary cast syndrome in nonliver transplant patients. J Clin Gastroenterol. 2008;42:752-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Yang YL, Tan WX, Liu XB, Li XT. Observation of Bacteria in Cholesterol Stones by Electronic Microscope. Zhongguo Puwai Jichu yu Linchuang Zazhi. 2004;5:447-449. [DOI] [Full Text] |
| 22. | Wu SD, Yu H, Su Y, Zhang ZH, Fan Y, Sun SL, Kong J, Tian Y, Tian Z, Wei Y. Study on etiology of primary bile duct pigment stones. Zhonghua Gandan Waike Zazhi. 2007;13:717-720. [DOI] [Full Text] |
P- Reviewers: Nundy S, Sugawara Y, Tolba RH S- Editor: Song XX L- Editor: Stewart G E- Editor: Liu XM