Published online Sep 21, 2013. doi: 10.3748/wjg.v19.i35.5929
Revised: April 24, 2013
Accepted: May 22, 2013
Published online: September 21, 2013
Processing time: 242 Days and 5.1 Hours
Minimal invasive techniques have allowed for major surgical advances. We report our initial experience of performing total laparoscopic left hepatectomy (segments II-IV) with the Lotus (laparoscopic operation by torsional ultrasound) Ultrasonic Scalpel. The perioperative and postoperative courses of the young female patient were uneventful and she is in a good general condition without complaints 18 mo after surgery. To the best of our knowledge, this is the first total laparoscopic hemihepatectomy to be performed in Greece, as well as the first laparoscopic liver resection using Lotus shears.
Core tip: This report describes the first total laparoscopic hemihepatectomy performed in Greece, as well as the first laparoscopic liver resection using Lotus shears. The effectiveness of the Lotus Ultrasonic Scalpel highlights the importance of surgical innovation in making minimally invasive procedures available to all surgical specialties.
- Citation: Sotiropoulos GC, Stamopoulos P, Charalampoudis P, Molmenti EP, Voutsarakis A, Kouraklis G. Totally laparoscopic left hepatectomy using the Torsional Ultrasonic Scalpel. World J Gastroenterol 2013; 19(35): 5929-5932
- URL: https://www.wjgnet.com/1007-9327/full/v19/i35/5929.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i35.5929
The development of minimally invasive hepatic resection techniques in the early 1990s established new surgical standards[1,2] and introduced highly innovative instruments such as ultrasonic dissectors, saline coagulation, and radiofrequency ablation[3-6]. We report our initial experience of performing a laparoscopic left hepatectomy with the ground-breaking Lotus (laparoscopic operation by torsional ultrasound) Ultrasonic Scalpel (S.R.A. Developments, Ashburton, Devon, United Kingdom).
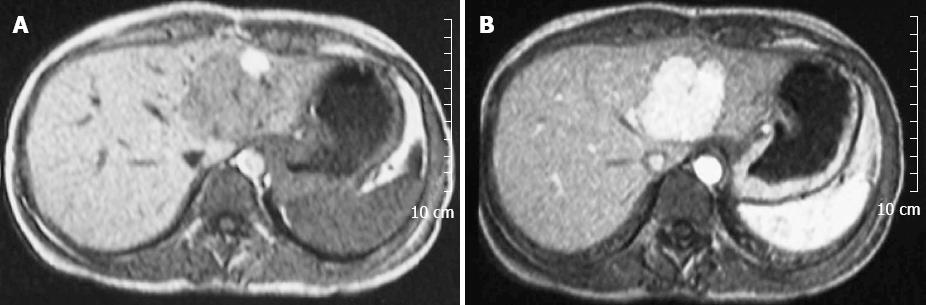
A 35-year-old asymptomatic woman with an unremarkable past medical history was referred to our department for surgical management of a liver lesion. The tumor had been diagnosed during work-up of elevated γ-glutamyltransferase (GT) (135 U/mL, normal laboratory range 7-36 U/mL) detected at premarital testing. Complete blood count, biochemical profile, liver function tests (except for γGT), and tumor markers were within the normal range. There was no history of oral contraceptive use. Abdominal ultrasound showed a 5-cm isoechoic liver mass in the left hepatic lobe. Gadolinium-enhanced magnetic resonance imaging (MRI) demonstrated a 5.2-cm lesion in segments III/IV, with compression of the middle and left hepatic veins (Figure 1). A laparoscopic left hemihepatectomy was scheduled with a presumed diagnosis of liver adenoma.
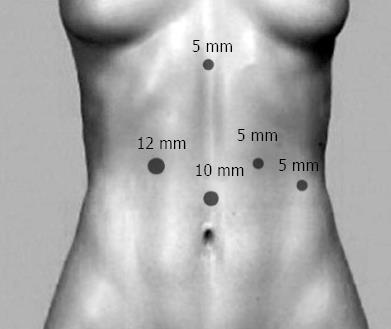
With the patient in the supine position and under general anesthesia[7], five trocar ports were placed as follows: an observation port (10 mm) 4 cm above the umbilicus; a main manipulation port (12 mm) in the midclavicular line below the right costal margin; a 5-mm port below the xiphoid process; and two 5-mm ports (for the assistant surgeon) in the left midclavicular and left anterior axillary lines, respectively (Figure 2). The operating surgeon stood between the patient’s legs.
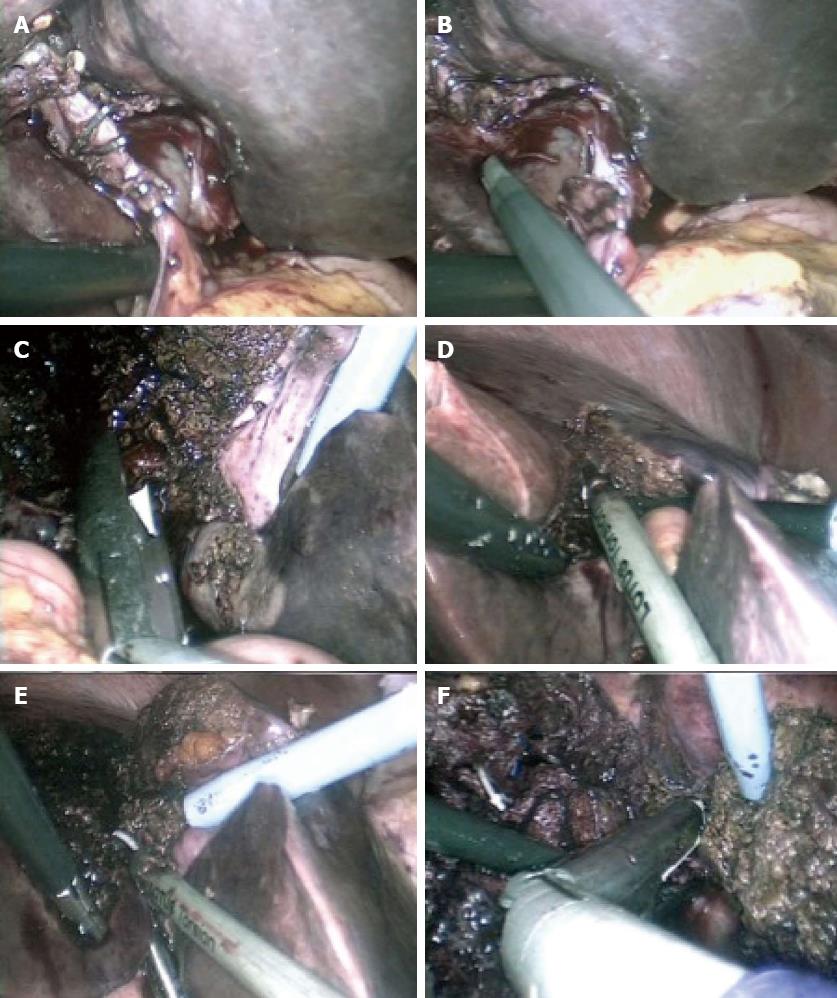
After the falciform and left triangular ligaments were transected, a replaced left hepatic artery branch was identified, clipped, and transected (Figure 3A and B). The left branch of the portal vein was bluntly dissected (Figure 3C) and ligated with an Endopath ETS Articulating Linear Cutter (Ethicon Endo-Surgery, Blue Ash, OH, United States). The liver parenchyma was divided using the Lotus Ultrasonic Scalpel (Figure 3D and E). Non-absorbable clips were used to control the middle hepatic vein, large vessels, intrahepatic bile ducts, and the left hepatic duct. Once this had been achieved, the left hepatic vein was exposed, dissected, and divided with an Endopath ETS Articulating Linear Cutter (Ethicon Endo-Surgery) (Figure 3F). The resected specimen (segments II-IV) was removed via a 6-cm supraumbilical incision (Figure 4).
Total operating time was approximately 4 h. Estimated blood loss was < 400 mL. The patient had an uneventful hospital course and was discharged on postoperative day 6. Pathological evaluation of the specimen revealed focal nodular hyperplasia. The patient married 6 mo later and is currently in good health 18 mo after the procedure.
Ultrasound-activated scalpels are safe and effective devices[8]. The Lotus Ultrasonic Scalpel introduced the concept of torsional rather than longitudinal ultrasound emissions to achieve transection and hemostasis. Its mechanism of action includes a vibratory grooved blade that generates compression forces directly into the target tissue, and a central blade that cuts as the Teflon jaw is closed. The components of the acoustic systems vibrate harmonically at 36.0 kHz. Laparoscopic torsional ultrasound shears have significant advantages over conventional cutting bipolar forceps when used to divide and coagulate pedicles in gynecological surgery. The Lotus shears are associated with shorter bisection times, less thermal damage, and more effective control of intraparenchymal blood vessels and bile ducts (a major limitation of previous devices).
To the best of our knowledge, this is the first total laparoscopic hemihepatectomy performed in Greece, as well as the first laparoscopic liver resection using Lotus shears. The effectiveness of the Lotus device further emphasizes the importance of surgical innovation in laparoscopic liver surgery.
| 1. | Cescon M, Vetrone G, Grazi GL, Ramacciato G, Ercolani G, Ravaioli M, Del Gaudio M, Pinna AD. Trends in perioperative outcome after hepatic resection: analysis of 1500 consecutive unselected cases over 20 years. Ann Surg. 2009;249:995-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 196] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 2. | Lin NC, Nitta H, Wakabayashi G. Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. Ann Surg. 2013;257:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 137] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 3. | S Hammond J, Muirhead W, Zaitoun AM, Cameron IC, Lobo DN. Comparison of liver parenchymal ablation and tissue necrosis in a cadaveric bovine model using the Harmonic Scalpel, the LigaSure, the Cavitron Ultrasonic Surgical Aspirator and the Aquamantys devices. HPB (Oxford). 2012;14:828-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Hirokawa F, Hayashi M, Miyamoto Y, Iwamoto M, Tsunematsu I, Asakuma M, Shimizu T, Komeda K, Inoue Y, Tanigawa N. A novel method using the VIO soft-coagulation system for liver resection. Surgery. 2011;149:438-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Geller DA, Tsung A, Maheshwari V, Rutstein LA, Fung JJ, Marsh JW. Hepatic resection in 170 patients using saline-cooled radiofrequency coagulation. HPB (Oxford). 2005;7:208-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Pai M, Frampton AE, Mikhail S, Resende V, Kornasiewicz O, Spalding DR, Jiao LR, Habib NA. Radiofrequency assisted liver resection: analysis of 604 consecutive cases. Eur J Surg Oncol. 2012;38:274-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Machado MA, Makdissi FF, Surjan RC, Herman P, Teixeira AR, C Machado MC. Laparoscopic resection of left liver segments using the intrahepatic Glissonian approach. Surg Endosc. 2009;23:2615-2619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Troisi RI, Van Huysse J, Berrevoet F, Vandenbossche B, Sainz-Barriga M, Vinci A, Ricciardi S, Bocchetti T, Rogiers X, de Hemptinne B. Evolution of laparoscopic left lateral sectionectomy without the Pringle maneuver: through resection of benign and malignant tumors to living liver donation. Surg Endosc. 2011;25:79-87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
P- Reviewer Shah OJ S- Editor Huang XZ L- Editor Kerr C E- Editor Ma S