Published online Jan 7, 2013. doi: 10.3748/wjg.v19.i1.122
Revised: October 15, 2012
Accepted: October 30, 2012
Published online: January 7, 2013
Acute appendicitis, which requires immediate surgical intervention, is an important diagnosis in patients with acute abdomen. However, developmental abnormalities may interfere with the preoperative diagnosis and surgical treatment in some cases. Agenesis and atresia of the cecal vermiform appendix is an extremely rare clinical diagnosis. In addition, preoperative diagnosis may be difficult in some cases. Thus, diagnosis of the congenital absence of the vermiform appendix requires a thorough exploration of the retrocecal and ileocecal regions. A 59-year-old male was admitted from the emergency services with right lower abdominal pain. A celiotomy was performed with the suspicion of acute appendicitis. However, an atresia of the vermiform appendix was observed. The patient’s appendix was thus removed. Pathological examination confirmed suppurative appendicitis. This case underlines the importance of the clinical entity for surgeons who may deal with a similar case.
- Citation: Yaylak F, Algin MC, Gungor Y, Korkmaz M. Atresia of the appendix vermiformis: A rare case of developmental abnormality. World J Gastroenterol 2013; 19(1): 122-124
- URL: https://www.wjgnet.com/1007-9327/full/v19/i1/122.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i1.122
Acute appendicitis is an important diagnosis in patients with acute abdomen, and requires immediate surgical intervention. However, developmental abnormalities of appendix vermiformis may interfere with the preoperative diagnosis and surgical treatment in some cases. Although rare, duplication and agenesis of appendix vermiformis have been reported previously[1-3]. Clinical diagnosis of developmental abnormalities merits a thorough exploration of the abdominal cavity when clinical and surgical findings are atypical[2,4,5]. A definite diagnosis is essential, not only to control the ongoing inflammation due to an overlooked appendix, but also to exclude a cancer misdiagnosis. Here we present an atresia of the vermiform appendix in a patient with acute abdomen.
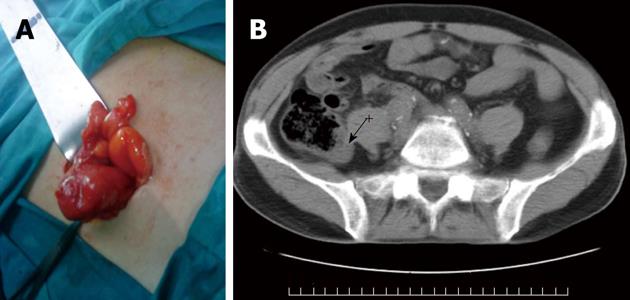
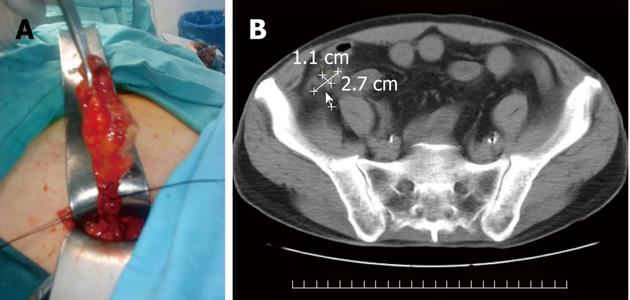
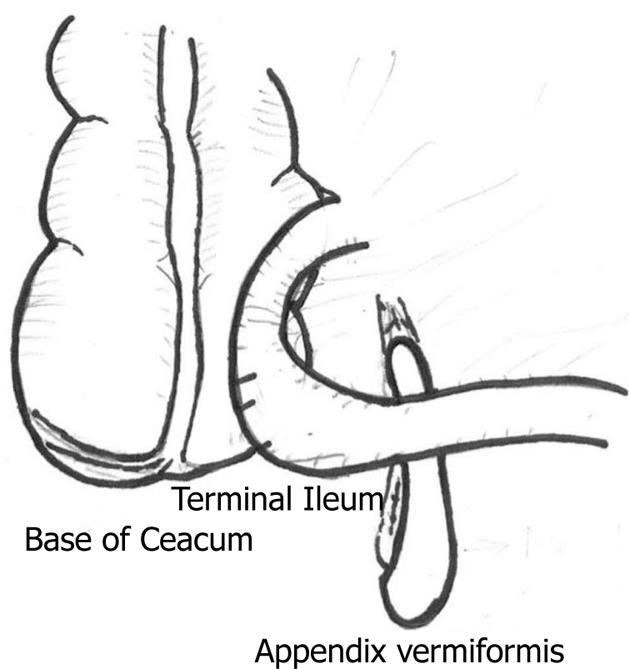
A 59-year-old male was admitted with acute abdomen. His past medical and surgical history was significant for coronary heart disease and a coronary by-pass surgery with two vessels replacement in 2005. His medication included oral anticoagulants and acetaminophen as needed for pain. He denied tobacco, alcohol, or intravenous drug use. He was afebrile and in mild distress at the time of presentation. His abdominal examination was significant for tenderness at McBurney’s point with voluntary guarding. Laboratory results revealed an elevated white blood cell count of 12.6 × 103/μL and a C-reactive protein level of 5.9 mg/L. Preoperative evaluation of the abdomen with computed tomography (CT) without contrast revealed mildly dilated loops of the small bowel, and questionable appendicitis with periappendiceal inflammation. The patient was thus scheduled for emergent diagnostic celiotomy. The preoperative diagnosis was suspicious for acute perforated appendicitis, and the intention was an appendectomy. Celiotomy was performed through a McBurney’s incision. Purulent material in the pericecal and pelvic cavity was observed, and the surgical cavity was cleared with aspiration and irrigation. The cecum and retrocecal region were macroscopically normal in appearance without an appendix vermiformis (Figure 1A). A mass, with a free tip, was observed approximately 10 cm proximal of the ileocecal valve (Figure 2A). The tip of the mass was inflamed and the lumen was ending blindly without a connection to the cecum. The mass was removed after preparation of its mesoappendix-like pedicle (Figure 3). The vascular supply of the mass was the ileocecal artery. Meckel’s diverticulum was excluded. After removal of the mass, the peritoneal and pelvic cavities were irrigated with saline, and a drain was placed in the pelvic cavity. Surgical incision was closed primarily. The drain was removed on the fifth postoperative day, and the surgical sutures were removed on the tenth day. Intravenous metronidazole (500 mg twice a day) was begun preoperatively and continued for five days. Analgesics were supplied as the patient needed. Pathological examination confirmed suppurative appendicitis. The initial surgical course was uneventful, but on the third day the patient was recognized to have a decrease in his speech ability and a loss of strength in his left leg. The end diagnosis was a transient ischemic attack from which the patient recovered after medical treatment with piracetam for five days and anticoagulation.
Developmental abnormalities of the appendix vermiformis, such as alterations in localization, duplication, or agenesis, may complicate the clinical and surgical presentation of patients with acute abdomen[2,3]. Thus, meticulous preoperative evaluation and surgical exploration of the abdominal cavity is essential in patients with atypical presentations[6-8]. Preoperative abdominal CT scanning may be helpful in some patients. In our case, an atresia of the appendix vermiformis was observed during surgical exploration. Preoperative abdominal CT images were reviewed with an experienced radiologist after surgery. Abdominal CT findings were found to be conclusive, with a focal increase in the thickness of the posteromedial wall of the cecum (Figure 1B). A tubular mass was noticed inferior to the cecum. There was no connection between this mass and the cecum (Figure 2B). In addition, the surrounding mesenteric fatty tissues were found to be dirty due to inflammation. Thus, this case also underlines the fact that a careful evaluation of abdominal CT images is the important part of the preoperative diagnosis. An experienced radiologist should be available to improve the preoperative diagnostic workup in the management of acute abdomen.
Previous reports with appendiceal developmental abnormalities have suggested an association with cancer[5]. In our experience, preoperative clinical presentation was suspicious for perforated appendicitis. However, a perforation was excluded with the presence of a healthy cecum and the observation of the inflamed mass in the ileocecal region. Cancer was excluded with histopathological examination of the resected mass. Routine histopathological examination should not be ignored in patients with appendicitis in order to exclude possible malign disorders[9].
In conclusion, this case is one of the first reports to demonstrate atresia of the appendix vermiformis. In such difficult cases, a surgeon should remember that a thorough exploration of the abdominal cavity is an essential part of the management of the patients with acute appendicitis. Preoperative diagnosis may be improved with the use of abdominal CT. Possible misdiagnoses may lead to inappropriate and inadequate treatment in patients with acute abdomen.
| 1. | Yucel AF, Pergel A, Kocakusak A, Aydin I, Bagci P, Sahin DA. Multiple caeco-appendiceal fistulas and diverticulosis: a newly defined congenital anomaly of the appendix-report of the first case. J Gastrointest Surg. 2011;15:2111-2113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Sobhian B, Mostegel M, Kunc C, Karner J. [Appendix vermiformis duplex--a rare surprise]. Wien Klin Wochenschr. 2005;117:492-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Woywodt A, Verhaart S, Kiss A. Atresia of the appendix. J Pediatr Surg. 1998;33:1423-1425. [PubMed] |
| 4. | Hsu KF, Yu JC, Chan DC, Liu YC. Atypical acute appendicitis and its complications: a rare location of the appendix in the periduodenum. Acta Gastroenterol Belg. 2011;74:105. [PubMed] |
| 5. | Freeman HJ. Duplicated appendix complicated by appendiceal cancer. World J Gastroenterol. 2011;17:135-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Chamisa I, Nikolov S, Bam TQ. Duplex appendicitis. S Afr Med J. 2007;97:843. [PubMed] |
| 7. | Samee A, Alibhai M, Ameer N, Sparks M, Morgan A, Halliday M. Appendicitis in a duplex appendix mimicking intussusception. BMJ Case Rep. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Collins DC. 71,000 Human appendix specimens. a final report, summarizing forty years’ study. Am J Proctol. 1963;14:265-281. [PubMed] |
| 9. | Chan W, Fu KH. Value of routine histopathological examination of appendices in Hong Kong. J Clin Pathol. 1987;40:429-433. [PubMed] |
P- Reviewers Amin AI, Leitman M S- Editor Gou SX L- Editor Rutherford A E- Editor Xiong L