Published online Nov 21, 2012. doi: 10.3748/wjg.v18.i43.6328
Revised: September 26, 2012
Accepted: September 29, 2012
Published online: November 21, 2012
Lymphangioma is a rare benign condition characterized by proliferation of lymphatic spaces. It is usually found in the head and neck of affected children. Lymphangioma of the small-bowel mesentery is rare, having been reported for less than 1% of all lymphangiomas. Importantly, it can cause fatal complications such as volvulus or involvement of the main branch of the mesenteric arteries, requiring emergency surgery. Moreover, the gross and histopathologic findings may resemble benign multicystic mesothelioma and lymphangiomyoma. Immunohistochemical study for factor VIII-related antigen, D2-40, calretinin and human melanoma black-45 (HMB-45) are essential for diagnosis. Factor VIII-related antigen and D2-40 are positive in lymphangioma but negative in benign multicystic mesothelioma. HMB-45 shows positive study in the smooth-muscle cells around the lymphatic spaces of the lymphangiomyoma. We report a case of small-bowel volvulus induced by mesenteric lymphangioma in a 2-year-and-9-mo-old boy who presented with rapid abdominal distension and vomiting. The abdominal computed tomography scan showed a multiseptated mass at the right lower quadrant with a whirl-like small-bowel dilatation, suggestive of a mesenteric cyst with midgut volvulus. The intraoperative findings revealed a huge, lobulated, yellowish pink, cystic mass measuring 20 cm × 20 cm × 10 cm, that was originated from the small bowel mesentery with small-bowel volvulus and small-bowel dilatation. Cut surface of the mass revealed multicystic spaces containing a milky white fluid. The patient underwent tumor removal with small-bowel resection and end-to-end anastomosis. Microscopic examination revealed that the cystic walls were lined with flat endothelial cells and comprised of smooth muscle in the walls. The flat endothelial cells were positive for factor VIII-related antigen and D2-40 but negative for calretinin. HMB-45 showed negative study in the smooth-muscle cells around the lymphatic spaces. Thus, the diagnosis was lymphangioma of the small bowel mesentery with associated small bowel volvulus.
- Citation: Suthiwartnarueput W, Kiatipunsodsai S, Kwankua A, Chaumrattanakul U. Lymphangioma of the small bowel mesentery: A case report and review of the literature. World J Gastroenterol 2012; 18(43): 6328-6332
- URL: https://www.wjgnet.com/1007-9327/full/v18/i43/6328.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i43.6328
Lymphangioma is a benign condition characterized by proliferation of the thin-walled lymphatic spaces[1]. It is believed to result from congenital lymphatic malformation rather than a true lymphatic neoplasm[2,3]. It is usually found in the head and neck regions during the first few years of life[1]. Lymphangioma of the small-bowel mesentery is rare, representing less than 1% of all lymphangiomas[2]. Volvulus is the most common manifestation of mesenteric lymphangioma[3].
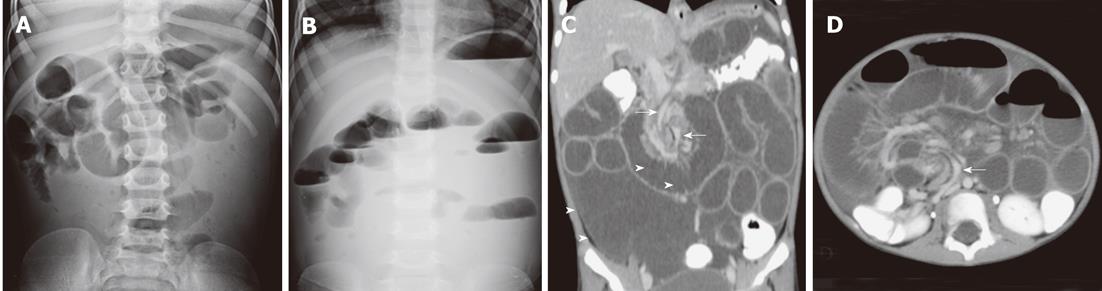
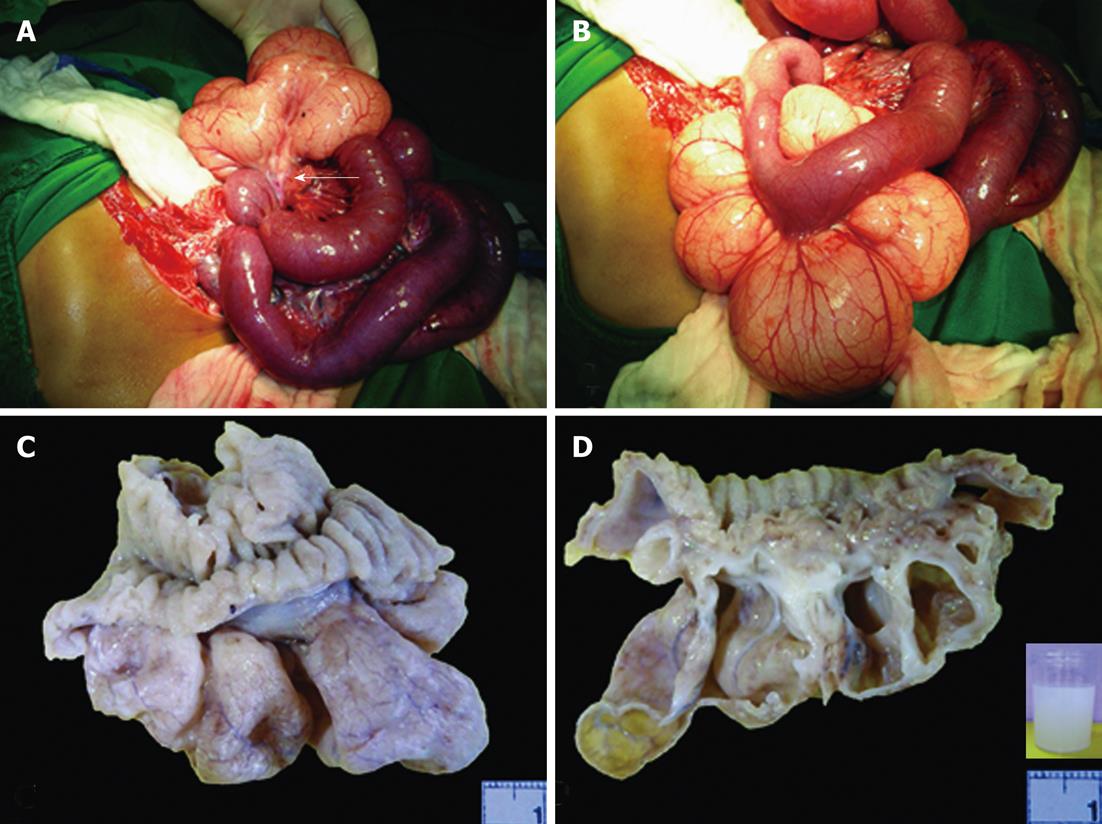
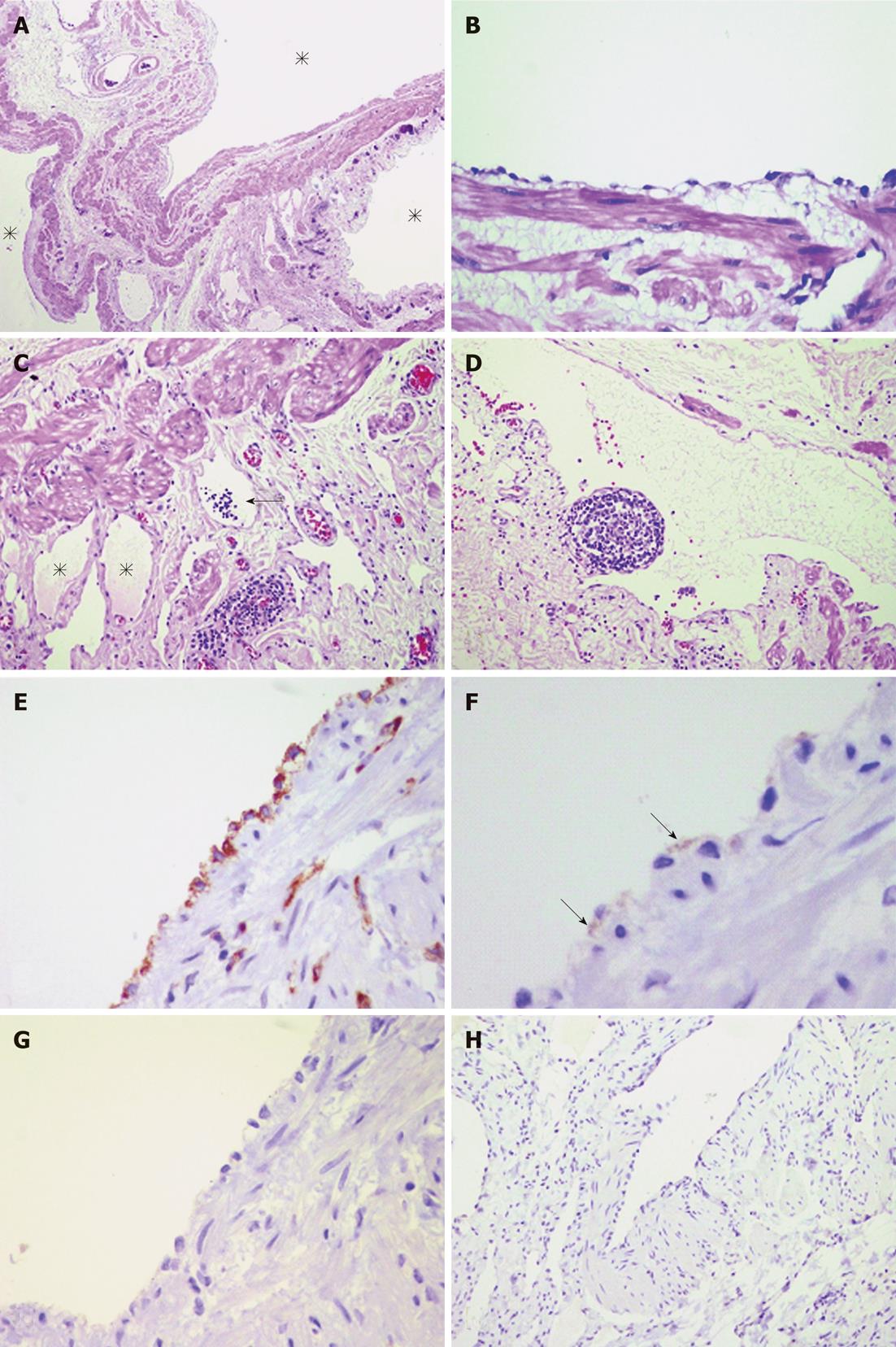
We report a case of a 2-year-and-9-mo-old boy who suffered from unexplained intermittent abdominal pain with vomiting since he was 6 mo old. These symptoms were temporarily relieved by treatment with anti-flatulence and anti-vomiting agents. However, the frequency and severity seemed to gradually increased. Fifteen days prior to admission to the hospital, he developed mucous bloody diarrhea with low-grade fever. He was treated by oral and intramuscular antibacterial agents and oral rehydration. Three days later, the diarrhea had diminished, but the low-grade fever persisted. When he was first brought to the emergency room, his vital signs were not remarkable except the pulse rate, 130 beats/min. Physical examination revealed abdominal distension. Other features were unremarkable. Stool exam was not performed. The initial diagnosis was acute infectious diarrhea. Intravenous fluid was administered, but the patient was not hospitalized. He was treated by oral antibacterial agents and oral rehydration. Five days later, the child was brought to the hospital for the second visit with a 1-d history of intermittent abdominal pain, rapid abdominal distension, and vomiting. However, there was no mucous bloody diarrhea or fever. The vomited content was food material admixed with greenish watery fluid. The patient’s vital signs were unremarkable except for the pulse rate, 110 beats/min. Physical examination revealed abdominal distension with diffuse tenderness and hyperactive bowel sounds but no abdominal rigidity. Rectal digital examination revealed yellow feces. Other features were unremarkable. Plain abdominal radiography revealed dilatation of the small-bowel loops at the upper and mid abdomen with multiple air-fluid levels, suggestive of small-bowel obstruction (Figure 1A and B). Abdominal CT scan revealed a thin-walled, fluid-filled, multiseptated mass, about 7.8 cm × 7 cm × 6.9 cm, at the right lower quadrant with compression of the adjacent bowel and generalized dilatation of the small-bowel loops in a whirl-like pattern, suggestive of a chylous mesenteric cyst associated with midgut volvulus (Figure 1C and D). Laparotomy was performed. During the operation, small-bowel volvulus with small-bowel dilatation and a mesenteric mass were found (Figure 2A and B). The mesenteric mass was lobulated, yellowish pink, cystic, and huge, measuring approximately 20 cm × 20 cm × 10 cm. The mass content was milky white, approximately 100 mL. The mesenteric mass with adjacent small-bowel segment were resected. Small-bowel anastomosis and decompression were performed. After formalin fixation, the mesenteric mass collapsed and shrank to 5.5 cm × 4.5 cm × 2.4 cm (Figure 2C). It was lobulated, cystic, semitranslucent, and pale tan with an adjacent small-bowel segment 5 cm long and 2 cm across. Cut surfaces of the mass revealed multicystic spaces of varying size (Figure 2D). The cystic walls were generally thin, but some walls were relatively thick. There was no fluid in the mass because it had been previously drained. However, there was residual milky white fluid in the specimen container representing the drained lymphatic fluid (inset of Figure 2D). The small-bowel mucosa was grossly unremarkable without invagination into the mass. Microscopic examination revealed that the cystic walls comprised of smooth muscle were lined with flat endothelial cells (Figure 3A and B). The stroma showed various sizes of small lymphatic spaces lined by a flat endothelium and containing small lymphoid cells (Figure 3C). The stroma also contained smooth-muscle bands and scattered lymphoid infiltrates (Figure 3C). Few subendothelial lymphoid follicles were observed, supporting the diagnosis of cystic lymphangioma (Figure 3D). The cell lining of the cystic walls was immunoreactive for factor VIII-related antigen (Figure 3E) and D2-40 (focal) (Figure 3F) but not for calretinin (Figure 3G) and human melanoma black-45 (HMB-45) (Figure 3H).
In conclusion, the diagnosis was cystic lymphangioma as indicated by proliferation of cystically dilated lymphatic spaces, immunoreactivity with factor VIII-related antigen and D2-40, and milky white content. Negative study of calretinin and HMB-45 excluded benign multicystic mesothelioma and lymphangiomyoma, respectively.
Lymphangioma is a mass-forming lesion characterized by numerous thin-walled lymphatic spaces and usually manifests in the first few years of life[1]. The common sites are the head, neck, and axillary regions. Other locations such as the abdominal or mediastinal cavity are rare, accounting for approximately 5% of lymphangiomas[2]. Among these, lymphangioma of the small-bowel mesentery has been described in less than 1% of lymphangiomas[1]. Lymphangioma appears to result from congenital malformation of lymphatic vessels rather than a true lymphatic tumor[2,3]. The former causes sequestration of lymphatic vessels during the embryonic period[1]. However, some data suggest that inflammation, abdominal trauma, abdominal surgery, radiation, or lymphatic obstruction may play a role in the genesis as a tumor[4,5]. Of note, the patient described in this case study had a history of intermittent abdominal pain without an identifiable cause from the time he was 6 mo old. This supports the theory of lymphangioma resulting from congenital malformation of lymphatic vessels rather than a tumor. Lymphangiomas are traditionally classified into three histologic types: capillary (simple), cavernous, and cystic[1]. The capillary (simple) type usually originates in the skin and consists of uniform small thin-walled lymphatic spaces. The cavernous type is composed of various sizes of dilated lymphatic spaces associated with lymphoid stroma and shows a connection with the adjacent normal lymphatic spaces. The cystic type consists of dilated lymphatic spaces of various sizes associated with collagen and smooth-muscle bundles in the stroma but lacks connection to the adjacent normal lymphatic spaces. Cystic lymphangioma findings are similar to cavernous lymphangioma findings in that dilated lymphatic spaces of variable size are seen for both[6].
In this case study, the mass was composed of cystically dilated lymphatic spaces of varying size associated with smooth-muscle cells, characteristic of cystic lymphangioma. An immunohistochemical study for D2-40, a lymphatic endothelial marker, showed focal positivity in the cystic wall endothelium, supporting the diagnosis[7]. Lymphoid follicles and lymphoid infiltrates in the stroma supported the diagnosis[8]. The milky white fluid content supported lymphangioma, in which the white color results from accumulated lymphoid cells. The differential diagnoses were lymphangiomyoma and benign multicystic mesothelioma. The former shows smooth-muscle cell proliferation around the lymphatic spaces with pericytic differentiation, demonstrated by HMB-45 immunoreactivity[8]. Benign multicystic mesothelioma consists of variably sized spaces lined by cuboidal or flattened mesothelial cells, with positive staining for mesothelial marker such as calretinin[9]. In this case study, the smooth-muscle cells around the lymphatic spaces were non-immunoreactive for HMB-45, and the lining cells of the cystic walls were non-immunoreactive for calretinin. Therefore, lymphangiomyoma and benign multicystic mesothelioma were excluded.
Intra-abdominal lymphangioma usually presents as abdominal distension, a palpable abdominal mass, or acute intestinal obstruction[2]. The latter is the most common presentation of mesenteric lymphangioma in the form of small-bowel volvulus[3]. Small-bowel volvulus is the rotation of the small bowel and its mesentery, usually complicated by acute intestinal obstruction. The precipitating factors to volvulus include postoperative adhesion bands, congenital bands, colostomy, ileostomy, fistula, tumors, omental defect, and Meckel’s diverticulum[10]. Mesenteric lymphangioma induces rotation of the small bowel, resulting in small-bowel volvulus with subsequent closed-loop small-bowel obstruction. Partial small-bowel obstruction induced by volvulus was responsible for the patient’s first visit, as manifested by abdominal distension. The patient’s fever and mucous bloody diarrhea might have resulted from secondary bowel inflammation related to volvulus, particularly hemorrhagic infarction, or from unrelated infectious diarrhea. Small-bowel volvulus with closed-loop obstruction resulted in the patient’s second visit and required emergency surgery. One month after the operation, the patient was brought for follow-up and did not manifest postoperative complications.
In conclusion, lymphangioma of the small-bowel mesentery is rare but can cause fatal complications such as volvulus or involvement of the main branch of the mesenteric arteries that requires emergency surgery[1]. The gross and microscopic findings may mimic benign multicystic mesothelioma in case of an overwhelming flattened mesothelium, and these conditions can be distinguished by immunohistochemical study.
| 1. | Chen CW, Hsu SD, Lin CH, Cheng MF, Yu JC. Cystic lymphangioma of the jejunal mesentery in an adult: a case report. World J Gastroenterol. 2005;11:5084-5086. [PubMed] |
| 2. | Jang JH, Lee SL, Ku YM, An CH, Chang ED. Small bowel volvulus induced by mesenteric lymphangioma in an adult: a case report. Korean J Radiol. 2009;10:319-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Campbell WJ, Irwin ST, Biggart JD. Benign lymphangioma of the jejunal mesentery: an unusual cause of small bowel obstruction. Gut. 1991;32:1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Hardin WJ, Hardy JD. Mesenteric cysts. Am J Surg. 1970;119:640-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Daniel S, Lazarevic B, Attia A. Lymphangioma of the mesentery of the jejunum: report of a case and a brief review of the literature. Am J Gastroenterol. 1983;78:726-729. [PubMed] |
| 6. | Rieker RJ, Quentmeier A, Weiss C, Kretzschmar U, Amann K, Mechtersheimer G, Bläker H, Herwart OF. Cystic lymphangioma of the small-bowel mesentery: case report and a review of the literature. Pathol Oncol Res. 2000;6:146-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Fenoglio-Preiser CM, Noffsinger AE, Stemmermann GN, Isaacson PG. Gastrointestinal pathology : an atlas and text. 3rd ed. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins 2008; 1253-1255. |
| 8. | Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss’s soft tissue tumors. 5th ed. Philadelphia, PA: Mosby/Elsevier 2008; 1144-1148. |
| 9. | Rosai J, Ackerman LV. Rosai and Ackerman’s surgical pathology. 9th ed. Vol 2, Edinburgh: Mosby 2004; 2375-2376. |
| 10. | Huang JC, Shin JS, Huang YT, Chao CJ, Ho SC, Wu MJ, Huang TJ, Chang FJ, Ying KS, Chang LP. Small bowel volvulus among adults. J Gastroenterol Hepatol. 2005;20:1906-1912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Peer reviewer: Edward J Ciaccio, PhD, Research Scientist, Department of Medicine, HP 804, Columbia University, 180 Fort Washington Avenue, New York, NY 10032, United States
S- Editor Gou SX L- Editor A E- Editor Xiong L