Published online Oct 21, 2012. doi: 10.3748/wjg.v18.i39.5658
Revised: June 7, 2012
Accepted: June 15, 2012
Published online: October 21, 2012
Endoscopic sphincterotomy (EST) is considered as a possible etiological factor for severe cholangitis. We herein report a case of severe cholangitis after endoscopic sphincterotomy induced by barium examination. An adult male patient presented with epigastric pain was diagnosed as having choledocholithiasis by ultrasonography. EST was performed and the stone was completely cleaned. Barium examination was done 3 d after EST and severe cholangitis appeared 4 h later. The patient was recovered after treated with tienam for 4 d. Barium examination may induce severe cholangitis in patients after EST, although rare, barium examination should be chosen cautiously. Cautions should be also used when EST is performed in patients younger than 50 years to avoid the damage to the sphincter of Oddi.
- Citation: Zhang ZH, Wu YG, Qin CK, Su ZX, Xu J, Xian GZ, Wu SD. Severe acute cholangitis after endoscopic sphincterotomy induced by barium examination: A case report. World J Gastroenterol 2012; 18(39): 5658-5660
- URL: https://www.wjgnet.com/1007-9327/full/v18/i39/5658.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i39.5658
Endoscopic retrograde cholangiopancreatography (ERCP) is an important diagnostic technique for biliary and pancreatic diseases. Endoscopic sphincterotomy has become a well established modality for common bile duct (CBD) stones[1,2]. However, endoscopic sphincterotomy is considered as a possible etiological factor for recurrent ascending cholangitis[3,4]. Here we report a case of severe cholangitis after endoscopic sphincterotomy induced by barium examination, and the patient was recovered after treatment with tienam.
A 40-year-old man presented with dull aching epigastric pain for 2 wk. He had a history of CBD stones for 2 years. The patient was averagely built and nourished. No jaundice was present. Biochemical parameters were all within normal limits. Total white blood cell (WBC) count and hemoglobin measurement were normal. Liver function tests showed that serum bilirubin was 13.5 μmol/L, alkaline phosphatase 55 U/L, aspartate aminotransferase (AST) 40 U/L and alanine aminotransferase (ALT) 35 U/L. Ultrasonography revealed CBD stones in the ampulla of vater and a dilated CBD of 12 mm in diameter. ERCP displayed a dilated CBD. Endoscopic sphincterotomy (EST) was performed in the Second Affiliated Hospital of China Medical University and stones were removed from the biliary tract. The general condition of the patient was good except for slight dull epigastric pain.
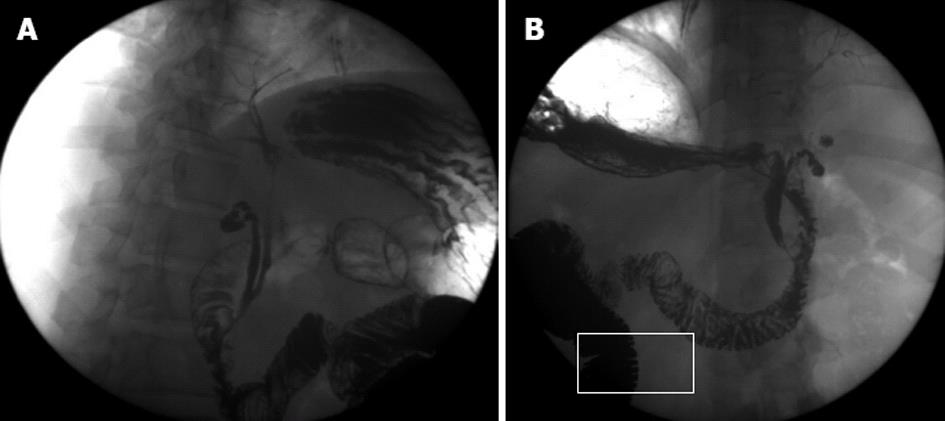
To rule out the disease of stomach, barium examination was made 3 d after EST. In the process of barium examination, barium could be seen refluxed into the biliary tree (Figure 1). Four hours later, the patient had a high fever and chills,and the body temperature was climaxed to 39.8 °C. On investigation, total WBC count was increased to 22.45 × 109/L, and hemoglobin was normal. Liver function tests showed serum bilirubin 33.5 μmol/L, alkaline phosphatase 155 U/L, AST 143 U/L and ALT 235 U/L, urine amylase 85 U/L and blood amylase 110 U/L. Ultrasonography showed a dilated CBD and no specific manifestation of the pancreas. Severe cholangitis after endoscopic sphincterotomy induced by barium examination was then diagnosed. The patient was recovered after treated with tienam for 4 d. He is still alive 5 years after the treatment, but suffered from 1-3 recurrent episodes of reflux cholangitis each year.
Endoscopic papillotomy with stone extraction continues to be a therapeutic choice and the reference standard in the treatment of symptomatic choledocholithiasis, especially for the solitary bile duct stones up to 12 mm in diameter. The overall success rate with EST was 95.7% in the present report. The most frequent complication encountered was bleeding, followed by acute pancreatitis, acute cholangitis, and perforation[5,6]. It has been found recently that the incidence of acute biliary pancreatitis may be lowered by pancreatic duct stenting[7].
After endoscopic sphincterotomy, the biliary sphincter is rendered permanently insufficient. The loss of this physiologic barrier between duodenum and biliary tract results in duodenocholedochol reflux and bacterial colonization of the biliary tract. Our previous study showed that about 35.9% of the patients with a T-tube after cholecystectomy and choledochotomy had duodenal-biliary reflux. Most of them had hypomotility of the sphincter of Oddi[8]. After EST, biliary reflux of duodenal chyme occurs in most patients, aerobilia is seen in about half, and bacterobilia in all the patients[9,10]. Most patients with bacterobillia did not inevitably develop symptomatic recurrent cholangitis, but 20% patients had upper abdominal pain during the follow-up of about 36 mo[11]. Another study showed that 65% patients after EST had duodenobiliary refux, detected by barium studies, although no clinical symptoms were observed [12]. The presence of bacteria in the biliary system, which is sterile under physiologic conditions, might lead to complications after EST. Misra et al[13] studied the incidence of duodenobiliary reflux and acute cholangitis after placement of self-expanding metal stent across the main duodenal papilla, and found that severe reflux of barium was evident in all the patients. However, none of them developed acute cholangitis because of reflux.
To avoid the damage to the biliary sphincter, endoscopic papillary balloon dilation (EPBD) was introduced as a less traumatic alternative to EST in the management of biliary tract stones[14]. However, a high incidence rate of procedure-induced pancreatitis was reported[15]. But, more recently, May et al[16] and Mathuna et al[17] found that the complication rates of pancreatitis by EPBD were similar to those by EST. Toda et al[18] studied the early results of EST and EPBD and found no difference in the early complications between EST and EPBD. The incidence rates of cholangitis by EST and EPBD were 4.0% and 4.2%, respectively. Yasuda et al[19] showed that preservation of papillary function after EPBD was not complete, but remained somewhat reduced. Preservation was more successful with EPBD than with EST. The incidence of pneumobilia was significantly higher in post-EST than in post-EPBD patients. Yasuda et al[20] also found that during long-term follow-up, patients who underwent endoscopic sphincterotomy (ES) had significantly more biliary complications than those who underwent EPBD. The biliary sphincter dysfunction after ES results in additional late complications.
Reflux of duodenal contents into the biliary tract after EST was the consequence of reduction or abolition of sphincter activity, as documented by manometry even 15 years following the sphincterotomy[21]. One study found that sphincterotomy was associated with a 5-fold higher incidence of recurrent brown CBD stones compared with choledocholithotomy[22]. One study reported the potentials of endoscopic papillary large balloon dilatation (EPLBD) with minor EST for the complete removal of CBD stones and found that the recurrence of CBD stones was especially low in cases of periampullary diverticulum treated with EPLBD by minor EST[23].
In our patient after EST, severe cholangitis occurred 4 h after gastrointestinal barium X-ray examination was done. In the process of barium examination, barium refluxed to the CBD, gallbladder and intrabiliary bile duct. Barium examination may induce severe cholangitis in patients after EST. Although the incidence is low, we should avoid early barium examination in patients after EST. The patient was younger than 50 years, if choledochotomy was performed and the sphincter of Oddi was preserved, reflux cholangitis might not occur.
In conclusion, EST, as a standard treatment of choledocholithiasis, destroyed the integrity of sphincter of Oddi which may induce reflux cholangitis. As a motivation factor, barium examination may induce severe cholangitis in patients after EST, although rare, it should be performed cautiously. Cautions should also be used when EST was performed in patients younger than 50 years to avoid the damage to the sphincter of Oddi.
| 1. | Demling L. Papillotomy--indications and technique. Endoscopy. 1983;15 Suppl 1:162-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Vaira D, D'Anna L, Ainley C, Dowsett J, Williams S, Baillie J, Cairns S, Croker J, Salmon P, Cotton P. Endoscopic sphincterotomy in 1000 consecutive patients. Lancet. 1989;2:431-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 179] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Goldman LD, Steer ML, Silen W. Recurrent cholangitis after biliary surgery. Am J Surg. 1983;145:450-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Geenen DJ, Geenen JE, Jafri FM, Hogan WJ, Catalano MF, Johnson GK, Schmalz MJ. The role of surveillance endoscopic retrograde cholangiopancreatography in preventing episodic cholangitis in patients with recurrent common bile duct stones. Endoscopy. 1998;30:18-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Wojtun S, Gil J, Gietka W, Gil M. Endoscopic sphincterotomy for choledocholithiasis: a prospective single-center study on the short-term and long-term treatment results in 483 patients. Endoscopy. 1997;29:258-265. [PubMed] |
| 6. | Gomutbutra T. Risk factors and techniques affecting surgical outcome of therapeutic endoscopic retrograde cholangiopancreatography difficulties. J Med Assoc Thai. 2005;88:1103-1109. [PubMed] |
| 7. | Dubravcsik Z, Hritz I, Fejes R, Balogh G, Virányi Z, Hausinger P, Székely A, Szepes A, Madácsy L. Early ERCP and biliary sphincterotomy with or without small-caliber pancreatic stent insertion in patients with acute biliary pancreatitis: better overall outcome with adequate pancreatic drainage. Scand J Gastroenterol. 2012;47:729-736. [PubMed] |
| 8. | Zhang ZH, Wu SD, Wang B, Su Y, Jin JZ, Kong J, Wang HL. Sphincter of Oddi hypomotility and its relationship with duodenal-biliary reflux, plasma motilin and serum gastrin. World J Gastroenterol. 2008;14:4077-4081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Seifert E. Long-term follow-up after endoscopic sphincterotomy (EST). Endoscopy. 1988;20 Suppl 1:232-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 1.5] [Reference Citation Analysis (2)] |
| 10. | Gregg JA, De Girolami P, Carr-Locke DL. Effects of sphincteroplasty and endoscopic sphincterotomy on the bacteriologic characteristics of the common bile duct. Am J Surg. 1985;149:668-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 101] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Greenfield C, Cleland P, Dick R, Masters S, Summerfield JA, Sherlock S. Biliary sequelae of endoscopic sphincterotomy. Postgrad Med J. 1985;61:213-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Escourrou J, Cordova JA, Lazorthes F, Frexinos J, Ribet A. Early and late complications after endoscopic sphincterotomy for biliary lithiasis with and without the gall bladder 'in situ'. Gut. 1984;25:598-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 170] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Misra SP, Dwivedi M. Reflux of duodenal contents and cholangitis in patients undergoing self-expanding metal stent placement. Gastrointest Endosc. 2009;70:317-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 88] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 14. | Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilation (EPD) for the treatment of common bile duct stones and papillary stenosis. Endoscopy. 1983;15 Suppl 1:197-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 146] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Kozarek RA. Balloon dilation of the sphincter of Oddi. Endoscopy. 1988;20 Suppl 1:207-210. [PubMed] |
| 16. | May GR, Cotton PB, Edmunds SE, Chong W. Removal of stones from the bile duct at ERCP without sphincterotomy. Gastrointest Endosc. 1993;39:749-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 67] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Mathuna PM, White P, Clarke E, Merriman R, Lennon JR, Crowe J. Endoscopic balloon sphincteroplasty (papillary dilation) for bile duct stones: efficacy, safety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 145] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Toda N, Saito K, Wada R, Kawabe T, Shiratori Y, Mitsushima T, Omata M. Endoscopic sphincterotomy and papillary balloon dilation for bile duct stones. Hepatogastroenterology. 2005;52:700-704. [PubMed] |
| 19. | Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001;49:686-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 158] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 20. | Yasuda I, Fujita N, Maguchi H, Hasebe O, Igarashi Y, Murakami A, Mukai H, Fujii T, Yamao K, Maeshiro K. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (2)] |
| 21. | Bergman JJ, van Berkel AM, Groen AK, Schoeman MN, Offerhaus J, Tytgat GN, Huibregtse K. Biliary manometry, bacterial characteristics, bile composition, and histologic changes fifteen to seventeen years after endoscopic sphincterotomy. Gastrointest Endosc. 1997;45:400-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 83] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Cetta F. Do surgical and endoscopic sphincterotomy prevent or facilitate recurrent common duct stone formation? Arch Surg. 1993;128:329-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Ha DW, Song GA, Kim DU, Kim GH, Heo J, Lee HW, Cho EJ, Jeon HK. Recurrent common bile duct stone and endoscopic treatment after endoscopic papillary large balloon dilatation with minor endoscopic sphincterotomy. Korean J Gastroenterol. 2011;57:352-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Peer reviewers: Dr. Seyfettin Koklu, Department of Gastroenterology, Ankara Education and Research Hospital, 06310 Ankara, Turkey; Atsushi Irisawa, Professor, Department of Gastroenterology, Fukushima Medical University Aizu Medical Center, 10-75 Shiromae, Aizuwakamatsu 960-8555, Japan; Ji Kon Ryu, Professor, Department of Internal Medicine, Seoul National University College of Medicine, 28 Yongon-dong, Chongno-gu, Seuol 110-744, South Korea
S- Editor Gou SX L- Editor A E- Editor Li JY