Published online Jan 21, 2012. doi: 10.3748/wjg.v18.i3.291
Revised: May 27, 2011
Accepted: June 4, 2011
Published online: January 21, 2012
Endoscopic submucosal dissection is a challenging technique that enables en-bloc resection for large colorectal tumors, as laterally spreading tumors, particularly difficult, if the ileocecal valve and terminal ileum is involved. Herein, we report on one of 4 cases. The procedures, using a bipolar needle knife (B-Knife) to reduce the perforation risk and carbon dioxide instead of conventional air insufflation for patient comfort, achieved curative resections without any complications.
- Citation: Kishimoto G, Saito Y, Takisawa H, Suzuki H, Sakamoto T, Nakajima T, Matsuda T. Endoscopic submucosal dissection for large laterally spreading tumors involving the ileocecal valve and terminal ileum. World J Gastroenterol 2012; 18(3): 291-294
- URL: https://www.wjgnet.com/1007-9327/full/v18/i3/291.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i3.291
Laterally spreading tumors (LSTs)[1] are mainly located in the cecum and rectum and endoscopic mucosal resection (EMR) is the therapeutic choice[2,3] because of their lower incidence of submucosal (sm) invasion. Involvement of the ileocecal valve with possible spreading to the terminal ileum, however, complicates the EMR and resulting in piecemeal resection in which persistent recurrence leads to surgery even for adenomas and intramucosal cancers[4]. In addition, the thin wall of the narrow ileum increases the risk of perforation during EMR[5].
Our experience suggests that the well-established endoscopic submucosal dissection (ESD) also produces good results in colorectal cases as in early gastric cancer treatment[6]. Unlike the stomach, colonic ESD presents high risk of complications[7] and increased patient discomfort. These factors motivated us to develop better techniques to achieve successful ESDs such as using a bipolar needle knife (B-Knife® Zeon Medical Co. Tokyo, Japan)[8] to reduce the risk of perforation and carbon dioxide (CO2) instead of conventional air insufflation for patient comfort[9].
In the present report, we describe our experience and the utility of using ESD on one of 4 complete resections of large LSTs (70 mm in diameter) involving the ileocecal valve and terminal ileum.
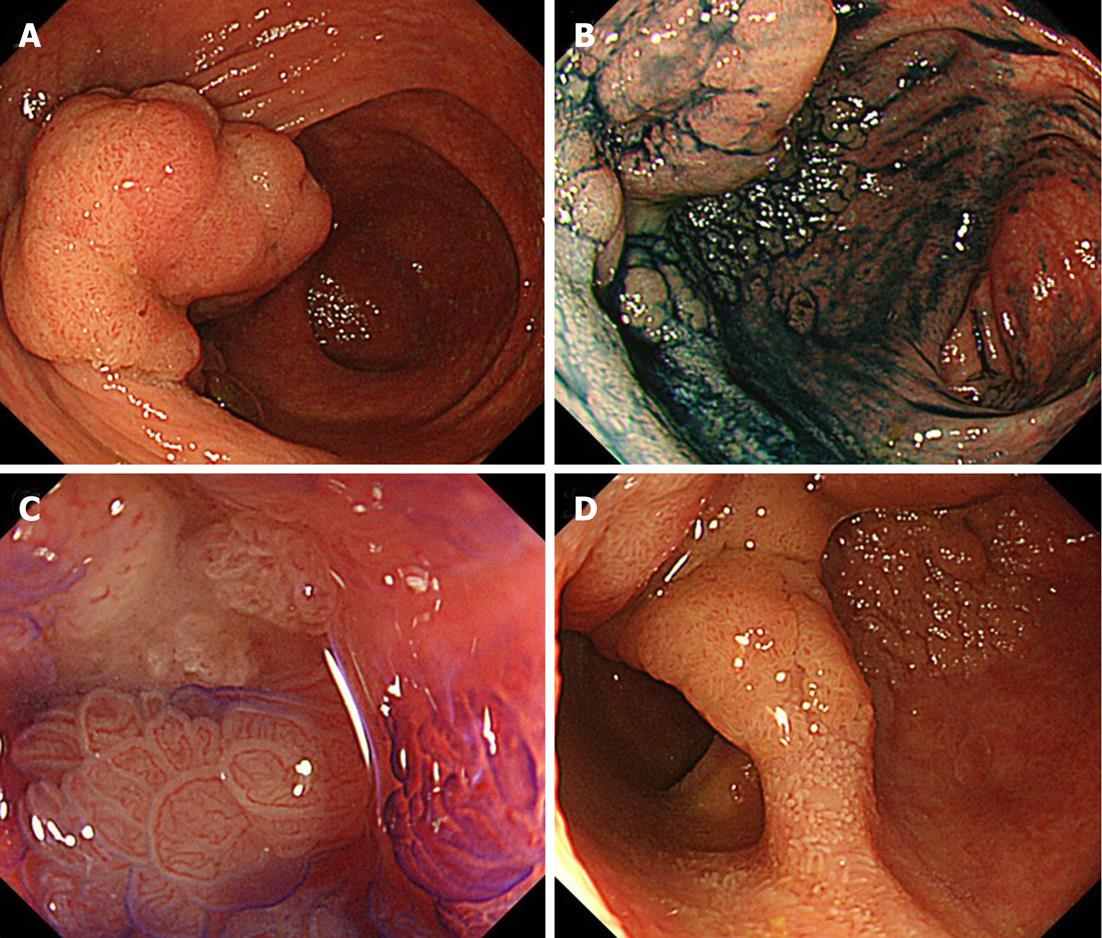
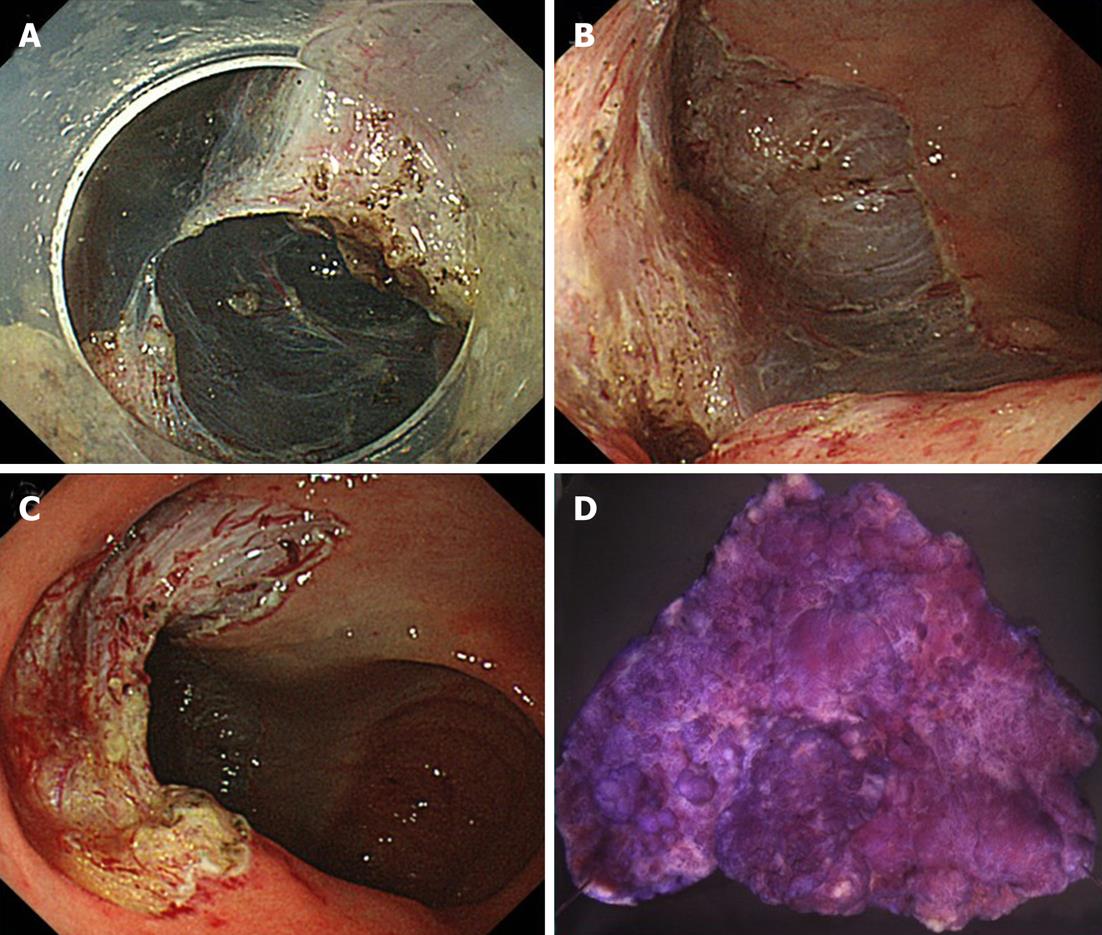
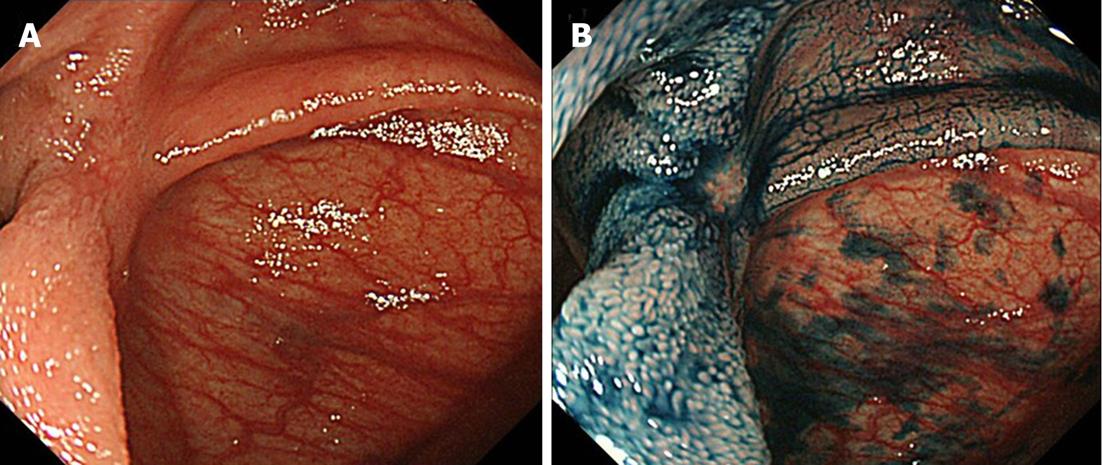
A 76-year-old woman was referred to our hospital for endoscopic treatment of a neoplastic lesion located at the cecum. Conventional colonoscopy revealed a broad base, flat tumor. After 0.4% indigo-carmine dye spraying, the margin of the 70 mm-lesion was clearly delineated (Figure 1A and B). High-magnification colonoscopy (PCF-Q240ZI; Olympus Optical Co. Ltd, Tokyo, Japan) disclosed a non-invasive pit pattern[10-12] indicating an intramucosal cancer despite the lesion’s large size (Figure 1C). Extension onto the terminal ileum until 1.5 cm from the ileocecal valve was also observed (Figure 1D). After diagnosing a Is+IIa, LST granular type (LST-G), we performed ESD using B-Knife and insulation-tip knife (IT-Knife) (Olympus Optical Co., Tokyo, Japan) (Figure 2A). During the procedure, we used CO2 instead of air insufflation to reduce patient’s intraoperative abdominal discomfort. This is a safe and effective technique suitable in lengthy colonic endoscopic procedures with the patient under conscious sedation[13]. Following the injection of glycerol and sodium hyaluronate solution into the sm layer[14,15], a circumferential incision was made using a B-Knife. The thickened sm layer was then dissected (oral to anal) across the ileocecal valve using both the B-Knife and IT-Knife. Finally, hemostasis was carefully checked throughout the ileocecal region (Figure 2B and C). The procedure took 150 min and neither perforation nor delayed bleeding was recognized. Hospitalization lasted four days with no further complications. Histopathology disclosed that the 70 mm resected specimen was an intramucosal cancer with tumor-free margins (Figure 2D). Although some retraction of the ileocecal valve could be observed, follow-up examinations after 6 mo revealed no residual tumor or recurrence (Figure 3A and B).
In the present report, en-bloc resection was successfully achieved by ESD using B-Knife and IT-Knife, despite the difficult location involving the ileocecal valve and terminal ileum and the large size of the lesion. IT-Knife, a developed insulation-tipped monopolar electrosurgical knife for removing large gastric lesions en-bloc, is not widely accepted in the colorectum because of its technical difficulty and the risk of complications, such as perforation and bleeding. On the other hand, a bipolar current minimizes the damage to deeper tissues. Thus, the current flow characteristics of the B-Knife reduce the vertical damage and risk of perforation demonstrating its utility for ileocecal ESDs[9,10].
Another important consideration was patient discomfort with air insufflation in long procedures. The supply of air can easily flow into the ileum causing painful distension even in EMRs for cecal lesions. In an earlier study aimed at reducing abdominal discomfort using CO2 in colorectal ESDs, we demonstrated the advantages and safety of CO2 compared to conventional air[14]. This factor was evident in the present case. Although a large amount of CO2 was supplied to the ileum, only a small amount of midazolam (4 mg in both cases) was required for intra-operative sedation.
Considering the indications for colorectal ESD, we generally recommend ESD for LST-non granular type lesions > 20 mm and planned piecemeal EMR for LST-Gs M < 40 mm[3]. In these four cases, we decided to perform ESD because of the LST-Gs large size, their location at the ileocecal valve and terminal ileum spreading, the probability of sm infiltration, and an increased likelihood of incomplete resections and recurrence.
In our institution, we have performed colorectal ESD using a B-Knife and an IT-Knife in 500 cases. Among of these 500 ESDs, large LST involving the ileocecal valve were only 4 cases, including the presented case. Based on our experience, lesions should be limited at most to 1 or 2 cm into the ileum and not circumferential. If the extension is more than 2 cm or circumferential, ESD would be very difficult and hazardous, so laparoscopy-assisted colectomy should be recommended. The reported case extended 1.5 cm into the ileum, making the most challenging one. Compared with conventional EMR[16], however, the longer procedure time for colorectal ESDs is still a problem. Nevertheless, we are improving our learning curve and using newly developed devices to reduce the length of the procedure and associated complications in order to increase the widespread use of colorectal ESD.
In conclusion, we successfully performed ESD in large LST-G involving the ileocecal valve and terminal ileum using a B-Knife and an IT-Knife with CO2 insufflation.
| 1. | Kashida H, Kudo SE. Early colorectal cancer: concept, diagnosis, and management. Int J Clin Oncol. 2006;11:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Saito Y, Fujii T, Kondo H, Mukai H, Yokota T, Kozu T, Saito D. Endoscopic treatment for laterally spreading tumors in the colon. Endoscopy. 2001;33:682-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 121] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Uraoka T, Saito Y, Matsuda T, Ikehara H, Gotoda T, Saito D, Fujii T. Endoscopic indications for endoscopic mucosal resection of laterally spreading tumours in the colorectum. Gut. 2006;55:1592-1597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 309] [Article Influence: 15.5] [Reference Citation Analysis (1)] |
| 4. | Sano Y, Machida H, Fu KI, Ito H, Fujii T. Endoscopic mucosal resection and submucosal dissection method for large colorectal tumors. Dig Endosc. 2004;16:S93-S96. [RCA] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Saito Y, Matsuda T, Kikuchi T, Ikehara H, Uraoka T. Successful endoscopic closures of colonic perforations requiring abdominal decompression after endoscopic mucosal resection and endoscopic submucosal dissection for early colon cancer. Dig Endosc. 2004;19:S34-S39. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Gotoda T, Kondo H, Ono H, Saito Y, Yamaguchi H, Saito D, Yokota T. A new endoscopic mucosal resection procedure using an insulation-tipped electrosurgical knife for rectal flat lesions: report of two cases. Gastrointest Endosc. 1999;50:560-563. [PubMed] |
| 7. | Park SY, Jeon SW. Acute intestinal obstruction after endoscopic submucosal dissection: report of a case. Dis Colon Rectum. 2008;51:1295-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Sano Y, Fu KI, Saito Y, Doi T, Hanafusa M, Fujii S, Fujimori T, Ohtsu A. A newly developed bipolar-current needle-knife for endoscopic submucosal dissection of large colorectal tumors. Endoscopy. 2006;38 Suppl 2:E95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Fu KI, Sano Y, Saito D. Endoscopic treatment of large superficial colorectal tumors: a case series of 200 endoscopic submucosal dissections (with video). Gastrointest Endosc. 2007;66:966-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 293] [Article Influence: 15.4] [Reference Citation Analysis (11)] |
| 10. | Fujii T, Hasegawa RT, Saitoh Y, Fleischer D, Saito Y, Sano Y, Kato S. Chromoscopy during colonoscopy. Endoscopy. 2001;33:1036-1041. [PubMed] |
| 11. | Matsuda T, Fujii T, Saito Y, Nakajima T, Uraoka T, Kobayashi N, Ikehara H, Ikematsu H, Fu KI, Emura F. Efficacy of the invasive/non-invasive pattern by magnifying chromoendoscopy to estimate the depth of invasion of early colorectal neoplasms. Am J Gastroenterol. 2008;103:2700-2706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 266] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 12. | Fujii T, Kato S, Saito Y, Kozu T, Matsuda N, Ota A, Gotoda T, ONO H, Sano Y. Diagnostic ability of staging in early colorectal cancer - Comparison with magnifying colonoscopy and endoscopic ultrasonography. Stomach Intestine. 2001;36:816-827. |
| 13. | Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Kozu T, Saito D. A pilot study to assess the safety and efficacy of carbon dioxide insufflation during colorectal endoscopic submucosal dissection with the patient under conscious sedation. Gastrointest Endosc. 2007;65:537-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 14. | Yamamoto H, Kawata H, Sunada K, Sasaki A, Nakazawa K, Miyata T, Sekine Y, Yano T, Satoh K, Ido K. Successful en-bloc resection of large superficial tumors in the stomach and colon using sodium hyaluronate and small-caliber-tip transparent hood. Endoscopy. 2003;35:690-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 300] [Article Influence: 13.0] [Reference Citation Analysis (1)] |
| 15. | Uraoka T, Fujii T, Saito Y, Sumiyoshi T, Emura F, Bhandari P, Matsuda T, Fu KI, Saito D. Effectiveness of glycerol as a submucosal injection for EMR. Gastrointest Endosc. 2005;61:736-740. [PubMed] |
| 16. | Tsuchida K, Joh T, Okayama N, Yokoyama Y, Senoo K, Okumura F, Gotoh K, Shiraki S, Okayama Y, Itoh M. Ileal adenoma with high-grade dysplasia involving the ileocecal valve treated by endoscopic mucosal resection: a case report. Gastrointest Endosc. 2002;55:125-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Peer reviewer: Giovanni D De Palma, Professor, Department of Surgery and Advanced Technologies, University of Naples Federico II, School of Medicine, Naples 80131, Italy
S- Editor Tian L L- Editor Cant MR E- Editor Xiong L