Published online Apr 21, 2012. doi: 10.3748/wjg.v18.i15.1800
Revised: November 22, 2011
Accepted: December 31, 2011
Published online: April 21, 2012
AIM: To investigate perception of natural orifice transluminal endoscopic surgery (NOTES) as a potential technique for appendectomy.
METHODS: One hundred patients undergoing endoscopy and 100 physicians were given a questionnaire describing in detail the techniques of NOTES and laparoscopic appendectomy. They were asked about the reasons for their preference, choice of orifice, and extent of complication risk they were willing to accept.
RESULTS: Fifty patients (50%) and only 21 physicians (21%) preferred NOTES (P < 0.001). Patients had previously heard of NOTES less frequently (7% vs 73%, P < 0.001) and had undergone endoscopy more frequently (88% vs 36%, P < 0.001) than physicians. Absence of hernia was the most common reason for NOTES preference in physicians (80% vs 44%, P = 0.003), whereas reduced pain was the most common reason in patients (66% vs 52%). Physicians were more likely to refuse NOTES as a novel and unsure technique (P < 0.001) and having an increased risk of infection (P < 0.001). The preferred access site in both groups was colon followed by stomach, with vagina being rarely preferred. In multivariable modeling, those with high-school education [odds ratio (OR): 2.68, 95% confidence interval (CI): 1.23-5.83] and prior colonoscopy (OR: 2.10, 95% CI: 1.05-4.19) were more likely to prefer NOTES over laparoscopic appendectomy. There was a steep decline in NOTES preference with increased rate of procedural complications. Male patients were more likely to consent to their wives vaginal NOTES appendectomy than male physicians (P = 0.02).
CONCLUSION: The preference of NOTES for appendectomy was greater in patients than physicians and was related to reduced pain and absence of hernia rather than lack of scarring.
- Citation: Hucl T, Saglova A, Benes M, Kocik M, Oliverius M, Valenta Z, Spicak J. Patient and physician perception of natural orifice transluminal endoscopic appendectomy. World J Gastroenterol 2012; 18(15): 1800-1805
- URL: https://www.wjgnet.com/1007-9327/full/v18/i15/1800.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i15.1800
Minimally invasive surgery has been challenging traditional open surgery. Laparoscopic surgery is less traumatic than open surgery, and is generally associated with fewer local and systemic complications, less postoperative pain, faster recovery and better cosmesis[1]. Natural orifice transluminal endoscopic surgery (NOTES) is a novel technique that takes advantages of natural orifices. It may be even less invasive than traditional laparoscopic surgery because it avoids abdominal incisions[2]. To date, a variety of surgical procedures using natural orifices have been performed in animals and humans[3,4].
The advantages of NOTES have not yet been fully confirmed in randomized trials[4], but are expected to include lack of scarring, a less profound systemic response, faster recovery, less pain and absence of hernia. Due to limited maneuverability and lack of efficient and safe closure of NOTES access sites, hybrid procedures involving additional laparoscopic instruments or vaginal access with hand-sutured closures have been used in most human procedures[5-7]. The overall complication rates reported in the first human studies have not exceeded those of laparoscopic surgery, but these findings remain to be proven in controlled trials[7]. Ultimately, the acceptance of NOTES procedures by both patients and physicians will be crucial in determining whether this new approach will become a part of our routine clinical practice.
Results of the few studies that have addressed the perception of NOTES have been variable. A very high patient preference of almost 80% for NOTES over laparoscopic cholecystectomy has been reported[8]. In contrast, the perception of NOTES among surgeons in another survey was receptive overall, but more cautious[9]. The aim of our study was to evaluate the perception of NOTES appendectomy among patients and physicians. Furthermore, we aimed to determine reasons for their preference, the preferred access site, and the extent of acceptable complication risk.
A group of consecutive patients scheduled to undergo procedures in the endoscopy unit were given a questionnaire by a staff member and asked to complete it anonymously. Physicians in various departments of our hospital (cardiology, cardiac surgery, gastroenterology, general surgery, diabetology, nephrology and radiology) also participated in the study and were given the same questionnaire. One hundred questionnaires were completed by each group and were evaluated. Participation in the study was voluntary. Only subjects with an intact appendix were included. Prior to beginning the study, the questionnaire was evaluated for consistency and clarity in a group of 20 medical students.
The first page of the questionnaire described acute appendicitis and its management in detail. The technique of laparoscopic appendectomy with its benefits and risks was explained. Then, the concept of NOTES was described; stating clearly that it is still an experimental technique with its benefits and risk being only estimated. It was stated that the technique was not available in our hospital and that the response of the patients would in no way influence their further medical management.
This information was followed by a list of 12 questions. Age, sex, educational status, prior awareness of NOTES and prior experience with endoscopy or laparoscopy were queried first. Then, preference between NOTES and laparoscopic appendectomy was determined. Those who preferred laparoscopy were asked for reasons for their preference with options being safety and efficiency of the technique, willingness to tolerate scars and pain, and because NOTES is new, concerns about the technique and risk of infection. The options offered to those preferring NOTES were less pain, absence of scars and hernia, and a new unique technique. Patients who chose NOTES were asked to score their preference for access site (1, 2 or 3, mouth/stomach, anus/colon, vagina in women). Men were also asked if they would object to a vaginal NOTES procedure for their wives. Those who preferred NOTES were asked about their tolerance for procedure-related complications (less, equal to, 1.5 times or two times greater than that of laparoscopic appendectomy), given a complication rate of laparoscopic appendectomy of around 8%.
We hypothesized a 56% preference of NOTES based on evidence available at the time of study design[10]. We expected physicians’ preference to be 75% of that of patients. Thus, assuming a power of 0.8 and α of 0.05, 99 patients and physicians needed to be included to show a statistically significant difference.
Data were analyzed for all participants overall and for both groups separately. The between-group differences were compared using a two-sample t test for continuous variables and Fisher’s exact test for categorical variables. Odds ratio (OR) and 95% confidence interval (CI) were calculated. A two-tailed P < 0.05 was required for statistical significance. To assess the effect of individual factors, multiple logistic regression was used. Analyses were performed using R software for statistical computing[11].
Questionnaires were obtained from a 100 patients and 100 physicians, and evaluated. Characteristics of the study subjects are summarized in Table 1. Fifty-six patients (56%) and 53 physicians (53%) were male. The mean age of patients was higher than that of physicians (52 years vs 41 years, respectively, P < 0.001). Previously, 88 patients (88%) had an endoscopy; 67 (67%) had upper gastrointestinal endoscopy and 60 (60%) had colonoscopy. Only 36 physicians (36%) had a previous endoscopy (P < 0.0001); 28 (28%) had upper gastrointestinal endoscopy (P < 0.0001) and 14 (14%) had colonoscopy (P < 0.0001). There was no statistically significant difference in prior laparoscopy experience (20 patients vs nine physicians, P > 0.05).
| Patients | Physicians | |
| Age (yr) | 52 (mean) | 41 (mean) |
| Men | 56 (56) | 53 (53) |
| Education | ||
| Graduate | 28 (28) | 100 (100) |
| High school | 58 (58) | 0 (0) |
| Elementary school | 14 (14) | 0 (0) |
| Heard of NOTES | 7 (7)a | 73 (73) |
| Prior endoscopy | 88 (88)a | 36 (36) |
| Prior laparoscopy | 20 (20) | 9 (9) |
| NOTES preference | 50 (50)a | 21 (21) |
| Laparoscopy preference | 50 (50)a | 79 (79) |
| Reasons for preference | ||
| Pain | 33 (66) | 11 (52) |
| Cosmesis | 15 (30) | 11 (52) |
| Absence of hernia | 22 (44)a | 17 (80) |
| Access site preference | ||
| Colon | 25 (50) | 12 (57) |
| Stomach | 19 (38) | 8 (38) |
| Vagina | 6 (12) | 1 (5) |
| Approval of wife’s NOTES | 42/49 (86)a | 29/46 (63) |
Fifty patients (50%) and only 21 physicians (21%) preferred NOTES over laparoscopic appendectomy (P < 0.01). For the patients, the OR for NOTES preference was 1 (95% CI: 0.676-1.480), and none of the queried characteristics influenced the preference for NOTES. For physicians, the OR for NOTES preference was low (OR: 0.152, 95% CI: 0.069-0.337). However, the OR for NOTES preference was significantly higher in female vs male physicians (OR: 2.875, 95% CI: 1.044-7.919).
The most common reasons for NOTES preference in patients was absence of pain [33 (66%)], followed by absence of hernia [22 (44%)] and cosmetic issues [15 (30%)]. The most common reasons in physicians were absence of hernia [17 (80%)] followed by cosmetic issues and absence of pain [11 (52%) each]. Absence of hernia was given as a reason for NOTES preference by significantly more physicians than patients (80% vs 44%, P < 0.001).
In both groups, the most frequently chosen reasons for preference of laparoscopy were proven safety [33 (66%) vs 65 (82%)] followed by absence of cosmetic concerns [31 (62%) vs 43 (54%)] and proven efficiency [20 (40%) vs 43 (54%)]. Physicians were more likely to chose laparoscopy for the reason that NOTES was a novel, unproven technique [33 (42%) vs 6 (12%), P < 0.0001] and had a greater risk of infection [25 (32%)) vs 2 (4%), P = 0.0001].
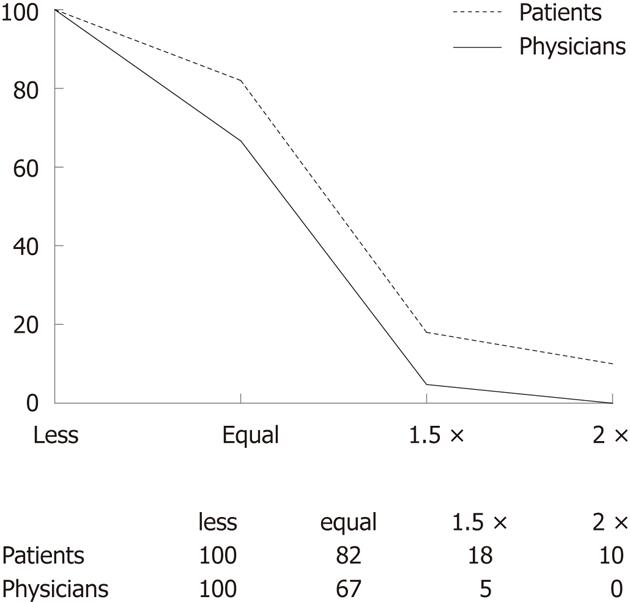
The preferred NOTES access site was the colon in both groups [25 (50%) vs 12 (57%)], followed by the stomach [19 (38%) vs 8 (38%)] with the vagina being rarely preferred [6 (27%) vs 1 (7%)]. Forty-two of 49 male patients (86%) but only 29 of 46 male physicians (63%) did not object to vaginal NOTES for their wives (P = 0.02). There was a steep decline in NOTES preference with an increased rate of procedural complications in both study groups (Figure 1). When the NOTES complication rate was lower than or equal to that of laparoscopic appendectomy (≤ 8%), it was acceptable for a vast majority of those preferring NOTES. Once the complication rate increased to twofold that of laparoscopy, the NOTES preference rate dropped to 10%.
When the study subjects were analyzed based on the overall NOTES preference vs laparoscopy, those with a university education [NOTES vs laparoscopy, 34 (27%) vs 94 (73%), P = 0.002], those who had heard of NOTES [20 (25%) vs 60 (75%), P = 0.02] and those who had not had prior colonoscopy [35 (28%) vs 91 (72%), P = 0.004] were more likely to prefer laparoscopic over NOTES appendectomy. In multivariable modeling, lower education status (high school) (OR: 2.678, 95% CI: 1.230-5.826) and prior colonoscopy (OR: 2.098, 95% CI: 1.050-4.192) were significantly associated with NOTES preference (Table 2).
NOTES is an experimental surgical approach in which an endoscope is passed through a natural opening (e.g., mouth, anus or vagina) and then through an internal incision in the stomach, colon or vagina. So far, NOTES has been limited primarily to animal procedures. Although a variety of procedures are technically possible in animals and the first laparoscopically assisted procedures have been performed in humans, the efficiency and safety of NOTES as well as its expected benefits, such as less trauma, remain to be shown[12]. Wide adoption of NOTES will depend largely on public acceptance.
Public acceptance and demand have previously been shown to play a major role in adoption of a surgical technique. In the 1980s when a totally new technique of gallbladder surgery, laparoscopic cholecystectomy, was introduced, medical professionals expressed little interest in the new approach. The early reports did not even show much benefit of the new concept except for cosmesis[13]. However, public demand influenced in part by industry marketing spurred adoption of this minimally invasive technique despite unproven benefits and increased risks. In spite of the early difference in patient and physician perception of laparoscopy, the technique has gained significant importance in abdominal surgery with laparoscopy cholecystectomy now representing a gold standard procedure. In parallel to this interesting phenomenon, we aimed to determine the perception of NOTES among patients and physicians.
Our study results show a discrepancy between patient and physician perception of this new technique. Half the patients questioned would prefer to undergo NOTES appendectomy despite the fact that the vast majority had never heard of the technique before. In contrast, most physicians refused the novel technique in favor of laparoscopic appendectomy. A few differences between the groups may have contributed to this result. First, the medical profession is known for its general skepticism of a new technique with an unproven rate of complications; thus the sensitivity to potential NOTES-associated risks was expected from the physicians[14]. Second, the mean age of the patients was older than that of the physicians; however, older age has previously been associated with decreased NOTES preference. Third, a majority of patients had previously undergone an endoscopy, and a previous positive experience with endoscopy may have contributed to their preference for NOTES, being partly an endoscopic technique.
Patients’ preference for NOTES in our study was lower than previously reported. Almost 80% of patients preferred NOTES over laparoscopy in a study performed by Varadarajulu et al[8] in 2008. The preference decreased to 56% in a study reported in 2009 by Swanstrom et al[10]. The observed decline may result from differences in the study design, chosen procedure or questioned populations. It may also reflect an actual trend of NOTES moving out of the public focus.
Physicians’ negative perception of NOTES is not completely new. In a recent study by Volckmann et al[9], surgeons were asked whether they would choose personally to undergo NOTES cholecystectomy. Only 26% of them opted for NOTES over laparoscopy, with most of the surgeons citing that NOTES was too new and was more risky. In another study by Thele et al[15], only 29% of gynecologists would recommend NOTES to their patients even if NOTES presented the same surgical risks as the laparoscopic approach. Interestingly however, female physicians in our study were almost three times more likely to choose NOTES than male physicians. The reason for this finding is unclear.
In patients, decreased postoperative pain was the major determinant for favoring NOTES. In physicians, the major determinant was absence of hernia. Surprisingly, cosmesis was considered important by only a third of patients and half of physicians. However, such a finding is consistent with a survey comparing NOTES and laparoscopy by Strickland et al[16], in which only 44% of women were concerned with scarring after laparoscopy. Even though we did not ask our subjects specifically for reasons for refusing NOTES, those who favored laparoscopic appendectomy most frequently reported proven safety of laparoscopy as their reason. The second most common reason was absence of cosmesis concerns, further supporting the above stated finding of cosmesis being a relatively infrequent reason for choosing NOTES. Thus, the most striking benefit of scarless surgery may not be the most important one for potential patients.
In our study, patients with high-school education and those with prior colonoscopy experience were significantly more likely to choose NOTES over laparoscopic appendectomy. However, this finding resulting from a multivariate analysis of the pooled data needs to be interpreted with caution. Our two groups of subjects differed a priori in their educational status, with all physicians having a university education. Furthermore, the frequency of prior colonoscopy was much lower in the physicians group. Thus, university education and low rate of prior colonoscopy experience were inherent attributes of the physicians group having a low preference for NOTES. Multivariate analysis of the patient group itself did not reveal any characteristics suggestive of NOTES preference.
Interestingly, in both groups, the preferred route of access was the colon, with the vagina preferred by only a minority of women. This finding was surprising given the very unpleasant bowel preparation required for transcolonic NOTES as opposed to transgastric and transvaginal NOTES, and is in contrast with some previously reported results[8]. It may be speculated that for some patients, removal of diseased organs may be better tolerated when performed via the anus as compared to the mouth. Another reason might be the high rate of prior colonoscopy experience in our subjects. The reserved attitude of women to transvaginal access is in contrast with previously published data[17], and deserves attention because most of the current procedures are offered via the transvaginal route due to uncertainty of transgastric or transcolonic closure.
The preference for NOTES decreased dramatically, even in those who preferred it, once the indicated rate of complications increased. This phenomenon was observed in both patients and physicians and has been reported previously by others[8]. However, in our study population, the NOTES preference was significantly lower than that reported by Swanstrom et al[10] In their study group, almost 20% of patients would have still elected NOTES even if the complication risk was 10 times greater than that of laparoscopy. Only less than 5% of our patients tolerated only twice the risk of laparoscopic appendectomy.
Interestingly, physicians were less willing than patients to consent to their wives vaginal NOTES procedure. This finding may be explained in part by the negative perception of NOTES itself by physicians as well as their better awareness of the possible complications associated with transvaginal procedures such as dyspareunia, infection and infertility.
Several limitations of our study should be noted. Only patients undergoing an endoscopic procedure were questioned. Such a study population may not accurately represent the general public. Next, our patients were asked about their perception of NOTES appendectomy. Acceptance of NOTES may be disease related and may thus be different for another procedure. Furthermore, our patients did not suffer from complaints of acute appendicitis and their decision was being made only based on description of the disease. They may also have been biased in favor of NOTES due to attending an endoscopy clinic as opposed to a surgical clinic. Finally, only a theoretical description of the benefits and risks was provided, which may change as more data are available.
In conclusion, the survey results show that there is considerable public interest in a new and experimental technique of transluminal surgery. In contrast, physicians would be reluctant to undergo NOTES. Decreased pain and absence of hernia were the most frequently reported reasons for choosing NOTES in patients and physicians, with cosmesis being of minor importance. Physicians were much more concerned than patients about the risk of infection. The study indicates that NOTES should be seriously considered as a potential technique with considerable public demand. However, it also highlights the importance of further development of the technique and outcomes data reporting to enlighten physicians about NOTES.
Natural orifice transluminal endoscopic surgery (NOTES) is a novel surgical technique that takes advantages of natural orifices. It may be even less invasive than traditional laparoscopic surgery because it avoids abdominal incisions.
Wide adoption of NOTES will depend largely on public acceptance. Results of the few studies that have addressed perception of NOTES have been variable.
The study shows that there is a considerable public interest for NOTES, even though it has declined over time. Physicians remain reluctant to undergo transluminal surgery.
The study indicates that NOTES should be seriously considered as a potential technique, with considerable public demand. However, further development is needed to convince physicians about the potential benefits of NOTES.
NOTES is a minimally invasive surgical technique that eliminates abdominal incision. Flexible endoscopes are used to create a transvisceral opening via natural orifice access to enter the peritoneal cavity.
This is a survey evaluating the acceptance of NOTES among patients and physicians. The authors found considerable acceptance, which at some points contrasts with previous studies, and is important to report.
| 1. | Zacks SL, Sandler RS, Rutledge R, Brown RS. A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol. 2002;97:334-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 125] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1037] [Cited by in RCA: 912] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 3. | Hucl T, Benes M, Kocik M, Krak M, Maluskova J, Kieslichova E, Oliverius M, Spicak J. A novel double-endoloop technique for natural orifice transluminal endoscopic surgery gastric access site closure. Gastrointest Endosc. 2010;71:806-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Meining A, Feussner H, Swain P, Yang GZ, Lehmann K, Zorron R, Meisner S, Ponsky J, Martiny H, Reddy N. Natural-orifice transluminal endoscopic surgery (NOTES) in Europe: summary of the working group reports of the Euro-NOTES meeting 2010. Endoscopy. 2011;43:140-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Zorron R, Maggioni LC, Pombo L, Oliveira AL, Carvalho GL, Filgueiras M. NOTES transvaginal cholecystectomy: preliminary clinical application. Surg Endosc. 2008;22:542-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 169] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 6. | Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg. 2007;142:823-826; discussion 823-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 615] [Cited by in RCA: 531] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 7. | Zornig C, Siemssen L, Emmermann A, Alm M, von Waldenfels HA, Felixmüller C, Mofid H. NOTES cholecystectomy: matched-pair analysis comparing the transvaginal hybrid and conventional laparoscopic techniques in a series of 216 patients. Surg Endosc. 2011;25:1822-1826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Varadarajulu S, Tamhane A, Drelichman ER. Patient perception of natural orifice transluminal endoscopic surgery as a technique for cholecystectomy. Gastrointest Endosc. 2008;67:854-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 92] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Volckmann ET, Hungness ES, Soper NJ, Swanstrom LL. Surgeon perceptions of Natural Orifice Translumenal Endoscopic Surgery (NOTES). J Gastrointest Surg. 2009;13:1401-1410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Swanstrom LL, Volckmann E, Hungness E, Soper NJ. Patient attitudes and expectations regarding natural orifice translumenal endoscopic surgery. Surg Endosc. 2009;23:1519-1525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | R Foundation For Statistical Computing R Development Core Team. R: A language and environment for statistical computing. Vol. 1. Vienna, Austria: R Foundation for Statistical Computing 2008; 2673. |
| 12. | Santos BF, Hungness ES. Natural orifice translumenal endoscopic surgery: progress in humans since white paper. World J Gastroenterol. 2011;17:1655-1665. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Squirrell DM, Majeed AW, Troy G, Peacock JE, Nicholl JP, Johnson AG. A randomized, prospective, blinded comparison of postoperative pain, metabolic response, and perceived health after laparoscopic and small incision cholecystectomy. Surgery. 1998;123:485-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 61] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Eckardt AJ, Pinnow G, Pohl H, Wiedenmann B, Rösch T. Antireflux 'barriers': problems with patient recruitment for a new endoscopic antireflux procedure. Eur J Gastroenterol Hepatol. 2009;21:1110-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Thele F, Zygmunt M, Glitsch A, Heidecke CD, Schreiber A. How do gynecologists feel about transvaginal NOTES surgery? Endoscopy. 2008;40:576-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Strickland AD, Norwood MG, Behnia-Willison F, Olakkengil SA, Hewett PJ. Transvaginal natural orifice translumenal endoscopic surgery (NOTES): a survey of women's views on a new technique. Surg Endosc. 2010;24:2424-2431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Peterson CY, Ramamoorthy S, Andrews B, Horgan S, Talamini M, Chock A. Women's positive perception of transvaginal NOTES surgery. Surg Endosc. 2009;23:1770-1774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
Peer reviewer: Dr. Stefan von Delius, Klinikum rechts der Isar, II. Medizinische Klinik, Ismaninger Str. 22, 81675 Munich, Germany
S- Editor Gou SX L- Editor Kerr C E- Editor Xiong L