Published online Oct 21, 2011. doi: 10.3748/wjg.v17.i39.4429
Revised: August 11, 2011
Accepted: August 18, 2011
Published online: October 21, 2011
AIM: To evaluate the efficacy of Stretta procedure with gastroesophageal reflux disease (GERD) based on symptom control, medication changes and oesophagitis grade.
METHODS: Ninety patients with a history of GERD underwent Stretta procedure from June 2007 to March 2010. All patients with GERD diagnosed by the presence of endoscopically evidenced oesophagitis or abnormal esophageal pH testing. We evaluated GERD-health-related quality of life, satisfaction, medication use and endoscopy at baseline, 6, 12 mo after treatment. Complications of the procedure were analyzed.
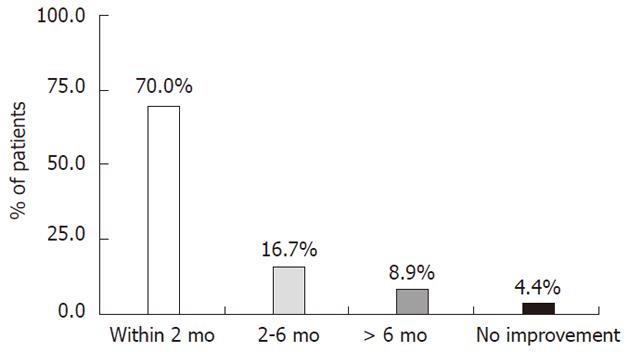
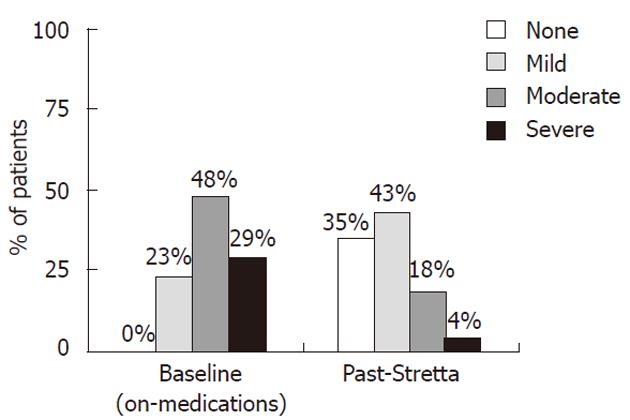
RESULTS: We found that patients experienced significant changes in symptoms of GERD after Stretta procedure. The onset of GERD symptom relief was less than 2 mo (70.0%) or 2 to 6 mo (16.7%). The mean GERD-HRQL score was 25.6 (baseline), 7.3 (6 mo, P < 0.01), and 8.1 (12 mo, P < 0.01).The mean heartburn score was 3.3 (baseline), and 1.2 (12 mo, P < 0.05). The percentage of patients with satisfactory GERD control improved from 31.1% at baseline to 86.7% after treatment, and patient satisfaction improved from 1.4 at baseline to 4.0 at 12 mo (P < 0.01). Medication usage decreased significantly from 100% of patients on proton pump inhibitors therapy at baseline to 76.7% of patients showing elimination of medications or only as needed use of antacids/H2-RA at 12 mo. An improvement in endoscopic grade of oesophagitis was seen in 33 of the 41 patients. All patients had either no erosions or only mild erosive disease (grade A) at 6 mo.
CONCLUSION: The experience with Stretta procedure confirms that it is well tolerated, safe, effective and durable in the treatment of GERD. The Stretta procedure provides the drug-refractory patients with a new minimally invasive method.
- Citation: Liu HF, Zhang JG, Li J, Chen XG, Wang WA. Improvement of clinical parameters in patients with gastroesophageal reflux disease after radiofrequency energy delivery. World J Gastroenterol 2011; 17(39): 4429-4433
- URL: https://www.wjgnet.com/1007-9327/full/v17/i39/4429.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i39.4429
Gastroesophageal reflux disease (GERD) is one of the most common illnesses of the gastrointestinal tract, with a large proportion of the population affected. Patients report adverse effects on their quality life because of symptoms such as heartburn, regurgitation, or dysphagia. GERD is associated with severe health-related quality-of-life impairment, which is comparable to patients afflicted with diabetes mellitus,congestive heart failure or arthritis[1]. Although GERD is known as a chronic disease requiring life-long treatment , many patients have inadequate symptom control with medication, usually proton pump inhibitors (PPIs). About 20% of patients will have breakthrough heartburn and regurgitation causing detrimental effects on the quality of life. GERD treatment using a minimally invasive endoluminal method to deliver low-level radiofrequency energy to the gastroesophageal junction (Stretta procedure) is a new method[2-4]. Several clinical trials showed that the Stretta procedure improves GERD symptoms, quality of life, esophageal acid exposure, and eliminates the need for antisecretory drugs in most patients[5-8].This study reports our experience using the Stretta procedure in patients with persistent GERD symptoms in China.
Fifty-seven men and 33 women (ages 31-72 years, 22.2% hiatal hernia, Table 1) were treated using the Stretta procedure. These patients had a history of GERD symptoms ranging from 1 to 26 years. They were either self-referred or recruited from the outpatient endoscopy unit from June 2007 to March 2010. All patients had significant GERD with persistent symptoms of heartburn and regurgitation in spite of the use of PPI drugs taken everyday. All patients had the diagnosis of GERD confirmed by finding erosive esophagitis at upper endoscopy (Los Angeles grade A or higher) or abnormal acid contact time detected at ambulatory esophageal pH testing. They were excluded if they were under 18 or over 80 years of age, pregnant, achalasia, or if they had a sliding hiatal hernia > 2 cm, collagen vascular disease, or severe uncontrolled medical illness.
| Characteristics | |
| No. of patients (n) | 90 |
| Gender (n) | |
| Male | 57 (63.3%) |
| Female | 33 (36.7%) |
| Age (yr) | |
| mean ± SD | 51 ± 13 |
| Range | 31-72 |
| Years with GERD | |
| mean ± SD | 6.7 ± 6.0 |
| Range | 1-26 |
| 0-2 | 21.1% |
| 3-5 | 38.9% |
| 6-8 | 10.0% |
| 8-11 | 14.4% |
| > 12 | 15.6% |
| Patients with hiatal hernia | |
| None | 77.8% |
| < 2 cm | 22.2% |
| Patients with esophagitis | |
| None | 54.4% |
| A | 13.3% |
| B | 28.9% |
| C | 3.3% |
Radiofrequency energy was delivered using the Stretta system (Curon Medical Inc., Sunnyvale, Calif., United States) in an outpatient endoscopy unit. The Stretta procedure catheter uses a balloon basket assembly to deploy 4 nitinol needle electrodes into the muscular layer of the esophageal wall. Radiofrequency energy delivered by the needle electrodes causes a thermal reaction in the LES with controlled temperature elevation to 85 °C, while continuous mucosal irrigation with chilled water prevents the development of stricture or ulceration. Deploying the needle electrodes at 5 mm levels above and below the squamocolumnar junction (SCJ) produces 56 thermal lesions. After informed consent, the patient is prepared for upper endoscopy with conscious sedation by using midazolam or fentanyl in the usual manner[9]. Diagnostic upper endoscopy is used to carefully inspect the esophagus and the cardia, and to determine the SCJ location. The Stretta catheter is passed over the guidewire, and introduced into the esophagus, where it is positioned 1 cm above the SCJ. After appropriate balloon inflation, the treatment elements are deployed 1 to 2 mm into the lower esophageal sphincter muscle, where energy is delivered in a series of thermal treatments at 4 levels in 2 positions (distal esophagus) and at 2 levels in 3 positions (gastric cardia). Constant monitoring and feedback of temperature and impedance ensures that each treatment element is maintained safely within target tissues. The mucosa was cooled during this procedure to prevent ulceration or stricture. After completion of the procedure and catheter removal, the diagnostic endoscopy procedure is repeated to verify that there have been no complications such as bleeding or perforation and to document the appropriate site of treatment. All pre-Stretta medication is maintained for 6 to 8 wk after the procedure to maintain baseline and allow time for complete healing.
GERD symptom assessment has been described as the most appropriate measure for the definition of treatment success, because it directly pertains to patients and the clinicians who provide their care. Before undergoing the Stretta procedure, patients underwent symptom assessment with the GERD health-related quality-of-life questionnaire (rated 0-50, with scores less than 10 considered normal)[10]. This is a validated questionnaire assessing specific GERD symptoms, followed by questions about heartburn severity on a scale of 0 to 5, with higher scores indicating more severe symptoms, and with questions about patient satisfaction on a scale of 0 to 5, with higher scores indicating better satisfaction/quality of life[11]. This testing was repeated 6 and 12 mo after the Stretta procedure. Assessment of medication usage was performed at baseline and 6 mo with the assistance of patient diaries and detailed questions addressing the use of all GERD medications such as PPIs, histamine-2 blockers, antacids, and prokinetic agents.
The date of the experiment was represented in the form of mean ± SD. Variance analysis and t test for non-match data were performed by a professional SPSS statistical program.
Minor complications occurred after the procedure, including 5 cases of dyspepsia (5.6%), 9 transient chest pain (10%), 2 superficial mucosal injury (2.2%), 3 mucosal bleeding (3.3%), 2 low-grade fever after procedure (2.2%). These complications resolved within 1 wk, without sequelae. No serious complications were noted after the procedure.
The onset of GERD symptom relief was reported as within 2 mo by the majority (70%) of patients, 2 to 6 mo by 16.7%, after 6 mo by 8.9%, and no improvement by 4.4% (Figure 1). At baseline, 77% of patients had moderate or severe symptoms despite PPI therapy. After Stretta, however, this number fell to 22%, indicating that 78% of patients had good control after treatment (Figure 2). The mean GERD-HRQL scores improved from 25.6 ± 9.0 at baseline to 7.3 ± 4.1 at 6 mo, and 8.1 ± 3.9 at 12 mo (P < 0.01). The mean heartburn scores improved from 3.3 ± 1.3 at baseline to 1.0 ± 0.9 at 6 mo, and 1.2 ± 1.1 at 12 mo (P < 0.05) (Table 2).
| Parameters | Baseline | 6 mo | 12mo | P value |
| GERD health-related quality-of-life questionnaire | 25.6 ± 9.0 | 7.3 ± 4.1 | 8.1 ± 3.9 | < 0.01 |
| Heartburn | 3.3 ± 1.3 | 1.0 ± 0.9 | 1.2 ± 1.1 | < 0.01 |
| Satisfaction | 1.4 ± 1.1 | 4.3 ± 1.3 | 4.0 ± 0.9 | < 0.01 |
| Percent without PPI | 0 | 78.9 | 76.7 | < 0.05 |
At baseline, only 31.1% of patients reported that they were satisfied with GERD symptom control on twice-daily PPI, whereas after Stretta treatment, 86.7% reported satisfactory GERD symptom control. This is also reflected in the satisfaction score, which improved from 1.4 ± 1.1 at baseline to 4.3 ± 1.3 at 6 mo, and 4.0 ± 0.9 at 12 mo (P < 0.01) (Table 2).
Medication usage decreased significantly (P < 0.05) (Table 2). At baseline, 100% of patients were receiving twice-daily PPI therapy. After Stretta treatment, 76.7% of patients showed elimination of medications or only as needed use of antacids/H2-RA at 12 mo.
Six months after Stretta treatment, an improvement in endoscopic grade of oesophagitis was seen in 33 of the 41 patients, 80.5% patients had no erosions, and only 19.5% patients had mild erosive disease (grade A).
GERD is a common disease that significantly impairs the quality of life of patients, and it is associated with pathophysiologic alterations such as transient lower esophageal sphincter relaxations and the presence of a hiatal hernia. Although antisecretory medications such as PPIs are considered as the mainstay of GERD treatment, they do not address any of the underlying pathophysiologic derangements. It is not surprising, therefore, that up to 20% of patients do not have adequate symptom control despite these drugs effectively control GERD in most patients by reducing acid reflux. Moreover, long-term use of these medications may provide a significant and lifelong economic expense. These patients may seek antireflux surgery, which has high success rates but may wane over time, with 50% of patients requiring medications to control recurrent reflux symptoms[12]. The invasiveness, high costs, and risks associated with surgery, and the dependence and long-term costs of medical management have caused patients and physicians alike to pursue a minimally invasive, effective, and durable treatment alternative that actually addresses the underlying pathophysiologic problems of GERD[7,13].
The Stretta endoscopic antireflux procedure was introduced in 2000 for the treatment of patients with GERD who had suboptimal symptom control with GERD therapy. The Stretta procedure has been found to have multiple mechanisms of action, including mechanical alteration of the gastroesophageal junction, with increased gastric yield pressure[14]; neural modulation of transient lower esophageal sphincter relaxation[15]; and normalization of delayed gastric emptying[14]. The Stretta procedure uses temperature-controlled delivery of radiofrequency energy to the lower esophageal sphincter to address the underlying pathophysiology. Production and healing of these lesions causes inflammation, subsequent collagen deposition[16,17], and muscular thickening[18], whereas efferent/afferent vagal nerve ablation causes a decrease in total lower esophageal sphincter relaxations and thus a decrease in esophageal acid exposure[19,20].
The Stretta procedure is an endoluminal radiofrequency energy delivery system to the gastroesophageal junction. Several clinical trials showed that the Stretta procedure improved GERD-related symptoms, decreased symptom scores and heartburn scores, increased the satisfaction. Meier et al[21] reported the results of an European multicenter, open-label, prospective study. At 12 mo after treatment, 75% of the patients were more satisfied with their symptom control and had statistically significantly fewer GERD symptoms. GERD-HRQL score decreased from 19.2 to 6.6 (P < 0.0001) and overall physical and mental health also improved significantly. This is also reflected in the satisfaction score, which improved significantly from 2 to 4 (P < 0.0001). Wolfsen et al[22] reported the multicenter Stretta registry study of 558 patients. The percentage of patients with satisfactory GERD control improved from 26.3% at baseline (on drugs) to 77.0% after treatment (P < 0.0001). Median baseline symptom control on drugs was 50%, compared with 90% at follow-up (P < 0.0001). Baseline patient satisfaction on drugs was 23.2%, compared with 86.5% at follow-up (P < 0.0001). Subgroup analysis showed a superior effect on symptom control in these patients beyond 1 year of follow-up, supporting procedure durability. Noar et al[9] reported on a series of 109 consecutive patients treated with the Stretta procedure who have reached 4-year follow-up. Heartburn scores decreased from 3.6 to 1.2 (P < 0.001), GERD-HRQL score decreased from 27.8 to 7.1 (P < 0.001), and patient satisfaction improved from 1.4 to 3.8 (P < 0.001). In our study, we found significant changes in symptoms of GERD. After treatment, onset of GERD symptom relief was less than 2 mo (70.0%) or 2 to 6 mo (16.7%). The GERD-HRQL score decreased from 25.6 to 8.1 (P < 0.01). The mean heartburn score decreased from 3.3 to 1.2 (P < 0.05). The percentage of patients with satisfactory GERD control improved from 31.1% at baseline to 86.7% after treatment, and patient satisfaction improved from 1.4 to 4.0 (P < 0.01).
The need for medication for GERD symptoms improved significantly one year after Stretta treatment compared to baseline. In our study, about 76.7% of the patients studied needed no medication or less medication after Stretta treatment. This is in line with results from Tam et al[15]. They report that at 12 mo after treatment, 75% of the patients are off all medication. Noar et al[9] presented 4-year of follow-up in 109 patients treated with the Stretta procedure. In their follow-up, medication usage decreased significantly from 100% of patients on twice-daily PPI therapy at baseline to 75% of patients showing elimination of medications or only as-needed use of antacids/over-the-counter PPIs. In a European study, Meier et al[21] report that at 6 mo after treatment, 45% and at 12 mo 38% of the patients are off all medication. Perhaps the lower percentage of patients that were off medication in Meier’s study was caused by the patient population having slightly different characteristics. 8.5% of their population had hiatal hernia > 2 cm, while other studies only included patients with hiatal hernia < 2 cm.
The Stretta procedure produced significant improvements in oesophagitis grade. Despite most patients being off therapy at 6 mo, only mild erosive reflux oesophagitis (grade A) was noted in 19.5% of the patients while remainder had no visible mucosal breaks. This is in line with results from Tam et al[23]. They report that at 6 mo after treatment, half of the patients had no macroscopic mucosal breaks and half of the patients had mild erosive reflux oesophagitis (Los Angeles grade A).
Taken together, the patients in this study had statistically significant improvement and a sustained effect in all parameters. In these patients, the observed improvement was superior to that achieved with escalated PPI therapy above baseline dosing. The Stretta procedure is a viable, well tolerated, minimally invasive endoluminal procedure[24,25]. This procedure should be considered for patients who are not satisfied with pharmacologic therapy and who are considering anti-reflux surgery.
Gastroesophageal reflux disease (GERD) is one of the most common illnesses of the gastrointestinal tract, with a large proportion of the population affected. GERD is associated with severe health-related quality-of-life impairment, which is comparable to patients afflicted with diabetes mellitus, congestive heart failure, or arthritis. Although antisecretory medications such as PPIs are considered as the mainstay of GERD treatment, up to 20% of patients do not have adequate symptom control despite these drugs effectively control GERD in most patients by reducing acid reflux. These patients may seek antireflux surgery, which has high success rates but may wane over time, with 50% of patients requiring medications to control recurrent reflux symptoms. The invasiveness, high costs, and risks associated with surgery, and the dependence and long-term costs of medical management have caused patients and physicians alike to pursue the minimally invasive, effective, and durable treatment methods.
The devices of endoluminal minimally invasive treatment of gastro-oesophageal reflux disease, which included endoluminal fundoplication(EndoCinch, NDO Plicator), biopolymer injection (Enteryx), and Stretta procedure, have gained popularity over the last several years. Endoluminal minimally invasive treatment of gastroesophageal reflux disease has been shown to be safe and effective in recent studies.
The experience with Stretta procedure confirms that it is well tolerated, safe, effective, and durable in the treatment of GERD. It has produced significant improvements in symptom control and oesophagitis grade and decreased medication usage. Stretta procedure is a new minimally invasive endoluminal therapeutic technique.
The Stretta procedure provides the drug-refractory patients with a new minimally invasive method. The Stretta procedure improves GERD symptoms, quality of life, esophageal acid exposure, and eliminates the need for antisecretory drugs in most patients.
Refractory GERD: Refractory GERD is a patient-driven phenomenon. What constitutes refractory GERD remains an area of controversy. Many investigators suggest that only patients who exhibit incomplete or lack of response to PPI, twice daily, should be considered as PPI failures. Others believe that a lack of symptomatic response to PPI once a day is sufficient to consider patients as PPI failures.
This is an interesting work. The study is useful in order to take advantages from a new therapeutic technique, above all for such a widespread disease like the gastroesophageal reflux. Moreover the possibility to avoid the more invasive surgery would be a desirable outcome for patients with severe GERD.
| 1. | Wiklund I. Review of the quality of life and burden of illness in gastroesophageal reflux disease. Dig Dis. 2004;22:108-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 142] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 2. | Chen D, Barber C, McLoughlin P, Thavaneswaran P, Jamieson GG, Maddern GJ. Systematic review of endoscopic treatments for gastro-oesophageal reflux disease. Br J Surg. 2009;96:128-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Spicák J. Treatment of gastroesophageal reflux disease: endoscopic aspects. Dig Dis. 2007;25:183-187. [PubMed] |
| 4. | Jafri SM, Arora G, Triadafilopoulos G. What is left of the endoscopic antireflux devices? Curr Opin Gastroenterol. 2009;25:352-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | White B, Jeansonne LO, Cook M, Chavarriaga LF, Goldenberg EA, Davis SS, Smith CD, Khaitan L, Lin E. Use of endoluminal antireflux therapies for obese patients with GERD. Obes Surg. 2009;19:783-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Comay D, Adam V, da Silveira EB, Kennedy W, Mayrand S, Barkun AN. The Stretta procedure versus proton pump inhibitors and laparoscopic Nissen fundoplication in the management of gastroesophageal reflux disease: a cost-effectiveness analysis. Can J Gastroenterol. 2008;22:552-558. [PubMed] |
| 7. | Higuchi K, Fujiwara Y, Okazaki H, Tabuchi M, Kameda N, Kadouchi K, Machida H, Tanigawa T, Shiba M, Watanabe T. Feasibility, safety, and efficacy of the Stretta procedure in Japanese patients with gastroesophageal reflux disease: first report from Asia. J Gastroenterol. 2007;42:205-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Aziz AM, El-Khayat HR, Sadek A, Mattar SG, McNulty G, Kongkam P, Guda MF, Lehman GA. A prospective randomized trial of sham, single-dose Stretta, and double-dose Stretta for the treatment of gastroesophageal reflux disease. Surg Endosc. 2010;24:818-825. [PubMed] |
| 9. | Noar MD, Lotfi-Emran S. Sustained improvement in symptoms of GERD and antisecretory drug use: 4-year follow-up of the Stretta procedure. Gastrointest Endosc. 2007;65:367-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Velanovich V. Comparison of symptomatic and quality of life outcomes of laparoscopic versus open antireflux surgery. Surgery. 1999;126:782-788; discussion 782-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Carlsson R, Dent J, Bolling-Sternevald E, Johnsson F, Junghard O, Lauritsen K, Riley S, Lundell L. The usefulness of a structured questionnaire in the assessment of symptomatic gastroesophageal reflux disease. Scand J Gastroenterol. 1998;33:1023-1029. [PubMed] |
| 12. | Spechler SJ, Lee E, Ahnen D, Goyal RK, Hirano I, Ramirez F, Raufman JP, Sampliner R, Schnell T, Sontag S. Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. JAMA. 2001;285:2331-2338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 660] [Cited by in RCA: 590] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 13. | Richards WO. Is the Stretta procedure safe and effective for the long-term control of symptoms in patients with refractory GERD? Nat Clin Pract Gastroenterol Hepatol. 2007;4:654-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Noar MD, Noar E. Gastroparesis associated with gastroesophageal reflux disease and corresponding reflux symptoms may be corrected by radiofrequency ablation of the cardia and esophagogastric junction. Surg Endosc. 2008;22:2440-2444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Tam WC, Holloway RH, Dent J, Rigda R, Schoeman MN. Impact of endoscopic suturing of the gastroesophageal junction on lower esophageal sphincter function and gastroesophageal reflux in patients with reflux disease. Am J Gastroenterol. 2004;99:195-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Utley DS, Kim M, Vierra MA, Triadafilopoulos G. Augmentation of lower esophageal sphincter pressure and gastric yield pressure after radiofrequency energy delivery to the gastroesophageal junction: a porcine model. Gastrointest Endosc. 2000;52:81-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 91] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Triadafilopoulos G, Dibaise JK, Nostrant TT, Stollman NH, Anderson PK, Edmundowicz SA, Castell DO, Kim MS, Rabine JC, Utley DS. Radiofrequency energy delivery to the gastroesophageal junction for the treatment of GERD. Gastrointest Endosc. 2001;53:407-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 103] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Kim MS, Holloway RH, Dent J, Utley DS. Radiofrequency energy delivery to the gastric cardia inhibits triggering of transient lower esophageal sphincter relaxation and gastroesophageal reflux in dogs. Gastrointest Endosc. 2003;57:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | DiBaise JK, Brand RE, Quigley EM. Endoluminal delivery of radiofrequency energy to the gastroesophageal junction in uncomplicated GERD: efficacy and potential mechanism of action. Am J Gastroenterol. 2002;97:833-842. [PubMed] [DOI] [Full Text] |
| 20. | Corley DA, Katz P, Wo JM, Stefan A, Patti M, Rothstein R, Edmundowicz S, Kline M, Mason R, Wolfe MM. Improvement of gastroesophageal reflux symptoms after radiofrequency energy: a randomized, sham-controlled trial. Gastroenterology. 2003;125:668-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 212] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 21. | Meier PN, Nietzschmann T, Akin I, Klose S, Manns MP. Improvement of objective GERD parameters after radiofrequency energy delivery: a European study. Scand J Gastroenterol. 2007;42:911-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Wolfsen HC, Richards WO. The Stretta procedure for the treatment of GERD: a registry of 558 patients. J Laparoendosc Adv Surg Tech A. 2002;12:395-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 55] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Tam WC, Schoeman MN, Zhang Q, Dent J, Rigda R, Utley D, Holloway RH. Delivery of radiofrequency energy to the lower oesophageal sphincter and gastric cardia inhibits transient lower oesophageal sphincter relaxations and gastro-oesophageal reflux in patients with reflux disease. Gut. 2003;52:479-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 89] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 24. | Zagol B, Mikami D. Advances in transoral fundoplication for oesophageal reflux. Dig Liver Dis. 2011;43:361-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Toydemir T, Yerdel MA. Laparoscopic antireflux surgery after failed endoscopic treatments for gastroesophageal reflux disease. Surg Laparosc Endosc Percutan Tech. 2011;21:17-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
Peer reviewers: Salvatore Leonardi, Assistant Professor, Department of Pediatrics, University of Catania, Via S. Sofia 78, 95100, Catania, Italy; Richard A Awad, Professor, Experimental Medicine and Motility Unit, Mexico City General Hospital, Dr. Balmis 148, Mexico DF, 06726 Mexico; Cesare Tosetti, MD, Department of Primary Care, Health Care Agency of Bologna Via Rosselli 21, 40046 Porretta Terme (BO), Italy
S- Editor Tian L L- Editor Ma JY E- Editor Xiong L