Published online Sep 21, 2011. doi: 10.3748/wjg.v17.i35.4001
Revised: March 11, 2011
Accepted: March 18, 2011
Published online: September 21, 2011
AIM: To investigate the rates of polyp detection in a mixed risk population using standard definition (SDC) vs high definition colonoscopes (HDC).
METHODS: This was a retrospective cohort comparative study of 3 colonoscopists who each consecutively performed 150 SDC (307, 200 pixel) and 150 HDC (792, 576 pixels) in a community teaching hospital.
RESULTS: A total of 900 colonoscopies were evaluated (mean age 56, 46.8% men), 450 with each resolution. Polyps of any type were detected in 46.0% of patients using SDC and 43.3% with HDC (P = 0.42). There was no significant difference between the overall number of polyps, HDC (397) and SDC (410), detected among all patients examined, (P = 0.73). One or more adenomatous polyps were detected in 24.2% of patients with HDC and 24.9% of patients with SDC colonoscopy (P = 0.82). There was no significant difference between HDC (M = 0.41) and SDC (M = 0.42) regarding adenomatous polyp (P = 0.88) or advanced adenoma (P = 0.56) detection rate among all patients examined.
CONCLUSION: HDC did not improve yield of adenomatous polyp, advanced adenoma or overall polyp detection in a population of individuals with mixed risk for colorectal cancer.
- Citation: Erim T, Rivas JM, Velis E, Castro F. Role of high definition colonoscopy in colorectal adenomatous polyp detection. World J Gastroenterol 2011; 17(35): 4001-4006
- URL: https://www.wjgnet.com/1007-9327/full/v17/i35/4001.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i35.4001
It is estimated that up to 15 million colonoscopies are performed annually in the United States[1,2]. Colonoscopy and polypectomy have been estimated to prevent 50%-80% of colorectal cancers[3-5]. However, recent trials have implied a lower level of protection and even a failure of colonoscopy to prevent right sided colon cancer[6,7]. With adenoma miss rates of up to 20% demonstrated for moderate sized polyps, the potential of improved polyp detection in preventing colon cancer deaths could be substantial[8-10].
A considerable effort is being spent on optimizing the yield of colonoscopy with respect to polyp detection. Several technologies such as wide-angle, cap-fitted, retroflexion colonoscopy and Third Eye Retroscope colonoscopy have been used in an attempt to increase mucosa exposure. Various optical enhancing technologies such as chromoendoscopy, narrow-band (NBI) and multi-band imaging , high definition, and autofluorescence have been studied as well. While some have been found to be effective in expert hands in tertiary care centers, many techniques suffer from issues of practicality. The rising demand of colon cancer screening and the advent of several different modalities for this purpose, such as computerized tomography colonoscopy, have stressed the importance of improved efficiency in colonoscopy.
At present, the only technical developments that are readily available and in use in routine practice settings in the United States are wide angle, high definition and NBI/multi-band imaging. High-definition endoscopes have been touted by manufacturers to show markedly clearer images in hopes that this would translate into higher polyp detection rates. In the current study, we present a comparison of polyp detection rate of endoscopists using standard definition and high definition endoscopy systems.
Nine hundred consecutive patients who had colonoscopy between May 2007 and May 2008 by three experienced endoscopists (> 6000 colonoscopies each) were selected for analysis retrospectively. Patients were mixed risk and all colonoscopies were performed at the same endoscopy center of a community teaching hospital in Florida, United States. Colonoscopies performed by gastroenterology fellows were excluded from the study. The study was approved by the Institutional Review Board at Cleveland Clinic Florida.
The standard definition colonoscopies (SDC) were performed with an EPK-1000 processor (Pentax), EC-3430LK, EC-3830LK, EC-3470LK, and EC-3870LK model colonoscopes (Pentax), a 19-inch CRT monitor at a resolution of 640 × 480 producing a 307, 200 pixel image at distance of approximately 2.8 m from the endoscopists. The high definition colonoscopies (HDC) were performed with an EPX-4400 digital processor (Fujinon), EC-450HL5 and EC-450LS5 model colonoscopes (Fujinon), a 32-inch LCD monitor at a resolution of 1032 × 768 producing a 792, 576 pixel image at a distance of approximately 2.8 m from the endoscopists. Both standard definition and high definition colonoscopes had a 140° field of view.
The Fujinon system has the capability of multi-band imaging that produces images similar to the NBI endoscopes, commercially termed Fuji Intelligent Chromo Endoscopy (FICE). The difference lies in that the Fujinon system uses software to construct images based on preset RGB wavelength combinations. The NBI systems use optical filters that restrict the bandwidth of a transmitted light signal. Currently available NBI systems utilize 2 narrow-band filters that provide tissue illumination in the blue (415 nm) and green (540 nm) spectrums of light[11]. The Fujinon equipment has ten factory-determined wavelength preset combinations.
Data from one hundred fifty consecutive patients who had colonoscopy with standard definition (SD) equipment were collected for three endoscopists from May - October 2007. Following the installation of the HDC system, all endoscopic procedures in our unit were performed exclusively using the high definition (HD) scopes and data was collected from 150 consecutive patients who had colonoscopy by the same three endoscopists from October 2007 - March 2008. The endoscopists were not aware of the study. Bowel preparation agents used were predominantly sodium phosphate and polyethylene glycol based regimens. The procedures were performed under a nurse administered standard sedation with Meperidine and Midazolam or anesthesiologist administered Propofol. Colonoscopy withdrawal times were recorded by the nursing staff.
Endoscopists were free to use the multi-band feature on the HDC system as needed. The system was initially set on the factory default preset of 0, which produced an image restricted to the following wavelengths: R 500 nm, G 445 nm, and B 415 nm. A push-button on the handle of the colonoscope was programmed to enable switching between conventional white-light image and the preset multi-band image. Endoscopists were also free to change to a different factory preset according to their preferences. The study was designed prior to arrival of the high definition system; however, data collection was started afterwards.
The data was collected from electronic medical records, procedure nursing notes, procedure reports, and pathology reports. The numbers of detected polyps recorded on the procedure reports were corroborated with the pathology reports and the nursing notes. The main outcome parameter was the polyp detection rate in the two groups. Secondary outcome measures included: detection rates of adenomatous polyps, advanced adenomas, and cancer. Advanced adenoma was defined as adenomatous polyps having one or more features of: > 1 cm in diameter, high-grade dysplasia, and villous histology. Additional data was collected with regards to patient age, gender, race, indication for colonoscopy, polyp location, procedure time, withdrawal time, type of sedation, and prep quality.
The Statistical Package for Social Sciences (SPSS 16.0) was used in order to organize, validate and analyze the collected data. Quantitative data were summarized using mean values (M) and standard deviation; Student’s t test were performed in order to detect significant differences between colonoscope types; equality of variances was inspected using Levene’s tests. We examined associations between categorical variables, performing χ2 tests or Fisher’s exact test when appropriate.
A total of 900 colonoscopies were evaluated, comparing 450 patients each who had colonoscopy with SDC equipment and HDC equipment. Each endoscopist performed 300 colonoscopies equally divided between standard and high definition procedures. The mean age of the study population was 56, and 46.8% were men. There were no statistically significant differences in patient characteristics between the two groups with the exception of a higher number of Hispanic patients and those that had screening colonoscopy in the HDC group (Table 1). However, there was no overall difference in adenomatous polyp detection rate in Hispanics (23.9%) vs Non-Hispanics (24.6%) (P = 0.86) and the screening (25.7%) and non-screening (21.7%) groups (P = 0.18).
| Parameters | HD group(n = 450) | SD2 group(n = 450) | P value |
| Patients | |||
| Mean age, years (SD1) | 55 (± 12.5) | 56 (± 11.4) | 0.21 |
| Men | 213 (47.3) | 208 (46) | 0.86 |
| Race | |||
| White | 233 (51.8) | 281 (62.4) | 0.10 |
| African American | 49 (10.9) | 53 (11.8) | 0.75 |
| Hispanic | 139 (30.9) | 95 (21.1) | 0.01 |
| Others | 29 (6.4) | 21 (4.7) | 0.31 |
| Indication | |||
| Screening | 216 (48.0) | 173 (38.4) | 0.07 |
| Non-screening | 234 (52.0) | 277 (61.6) | 0.13 |
| Cecal intubation | 433 (96.2) | 438 (97.3) | 0.92 |
| Poor prepare | 14 (3.1) | 17 (3.8) | 0.72 |
| Withdrawal all procedures, min (SD1) | 11.3 (± 6.1) | 10.8 (± 5.6) | 0.20 |
| Withdrawal non-polypectomy, min (SD1) | 10.0 (± 5.9) | 9.2 (± 4.2) | 0.02 |
Cecal intubation, bowel prep quality and withdrawal times were also not statistically significantly different between the HDC and SDC groups. The cecum was reached in 96.7% of all cases. Average withdrawal time was 11.1 min, which included polypectomy time.
Polyps of any type were detected in 46.0% of patients with SDC and 43.3% of those patients who had HDC (P = 0.42). There was no significant difference between the overall number of polyps, HDC (397) and SDC (410), detected among all patients examined (P = 0.73). One or more adenomatous polyps were detected in 24.2% of patients with HDC and 24.9% of patients with SDC
(P = 0.82). There was no significant difference between HDC (M = 0.41) and SDC (M = 0.42) regarding adenomatous polyp detection rate among all patients examined (P = 0.88). In addition, there was no significant difference between the study groups regarding advanced adenoma polyp detection rates (P = 0.60) or cancer detection rate among all patients examined (P > 0.05) (Table 2). There was no difference in polyp detection rates when each individual endoscopist’s HDC and SDC detection rates were compared (data not shown).
| Parameters | HD group(n = 450) | SD2 group(n = 450) | P value |
| Total polyps detected | 397 | 410 | 0.73 |
| Non-adenomas | 196 (51.3) | 209 (52.0) | 0.81 |
| Non-advanced adenomas | 150 (39.3) | 150 (37.3) | 0.84 |
| Advanced adenomas | 34 (8.9) | 40 (10.0) | 0.60 |
| Cancer | 2 (0.5) | 3 (0.7) | 1.00 |
| Pathology not identified | 15 (3.8) | 8 (2.0) | 0.14 |
| < 6 mm | 325 (81.9) | 340 (82.9) | 0.96 |
| 6-10 mm | 50 (12.6) | 44 (10.7) | 0.45 |
| > 10 mm | 22 (5.5) | 24 (5.9) | 1.00 |
| Size not specified | 0 | 2 | 0.50 |
| All patients | |||
| With non-adenomas | 84 (18.7) | 92 (20.4) | 0.56 |
| With non-advanced adenomas | 84 (18.7) | 83 (18.4) | 1.00 |
| With advanced adenomas | 25 (5.6) | 29 (6.4) | 0.67 |
| With cancer | 2 (0.4) | 3 (0.7) | 1.00 |
| Polyps per pt, mean (SD1) | 0.88 (± 1.63) | 0.91 (± 1.41) | 0.77 |
| Adenomas per pt, mean (SD1) | 0.41 (± 1.04) | 0.42 (± 0.94) | 0.88 |
| Advanced adenoma per pt, mean (SD1) | 0.076 (± 0.35) | 0.089 (± 0.38) | 0.56 |
| Adenocarcinoma per pt (mean) | 0.004 | 0.006 | |
| Screening patients, n | 216 | 173 | 0.07 |
| With non-adenomas | 49 (22.7) | 36 (20.8) | 0.81 |
| With non-advanced adenomas | 41 (19.0) | 32 (18.5) | 1.00 |
| With advanced adenomas | 13 (6.0) | 14 (8.1) | 0.55 |
| With cancer | 1 (0.5) | 0 (0.0) | 1.00 |
| Non-screening patients, n | 234 | 277 | 0.13 |
| With non-adenomas | 35 (15.0) | 56 (20.2) | 0.59 |
| With non-advanced adenomas | 43 (18.4) | 51 (18.4) | 0.21 |
| With advanced adenomas | 12 (5.1) | 15 (5.4) | 1.00 |
| With cancer | 1 (0.4) | 3 (1.1) | 0.63 |
Polyps detected during the procedures were also analyzed according to size. There was no significant difference between the detected number of polyps of sizes < 6 mm, 6-10 mm, and >10 mm in the HDC and SDC groups.
Gender was shown to be a significant variable as men in this study were found to have a higher incidence of all polyps (P < 0.01), adenomatous polyps (P < 0.01) and advanced adenomas (P < 0.01). However, this disparity was consistent in both cohorts with no statistically significant difference between the HDC and SDC groups (Table 3).
| Parameters | HD group(n = 450) | SD group(n = 450) | P value |
| Male | |||
| Total polyps detected | 264 | 245 | 0.74 |
| Patients | 213 | 208 | 0.86 |
| With non-adenomas | 42 (19.7) | 46 (22.1) | 0.48 |
| With non-advanced adenomas | 52 (24.4) | 43 (20.7) | 0.50 |
| With advanced adenomas | 17 (8.0) | 21 (10.1) | 0.50 |
| With cancer | 1 (0.5) | 2 (1.0) | 0.62 |
| Female | |||
| Total polyps detected | 133 | 165 | 0.21 |
| Patients | 237 | 242 | 0.87 |
| With non-adenomas | 42 (17.7) | 46 (19.0) | 0.82 |
| With non-advanced adenomas | 32 (13.5) | 40 (16.5) | 0.45 |
| With advanced adenomas | 8 (3.4) | 8 (3.3) | 1.00 |
| With cancer | 1 (0.4) | 1 (0.4) | 1.00 |
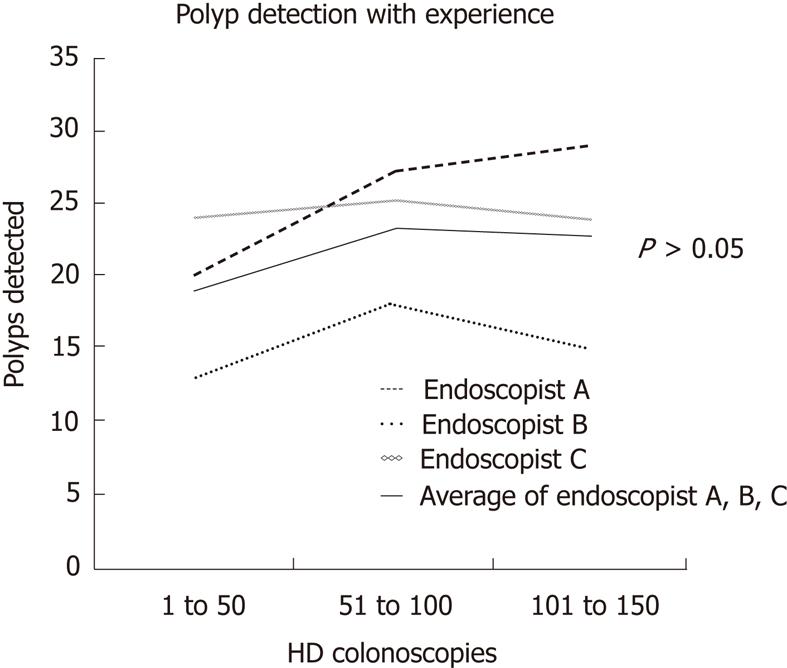
We found that the overall polyp and adenoma detection rates did not change significantly between the first, second or third 50 HDC performed by our endoscopists when the three were coned (P > 0.05). Therefore, there does not seem to be a learning effect associated with use of HDC with on demand multi-band imaging capability by endoscopists who had not used them before (Figure 1).
Our goal in this study was to assess the performance of HDC with regards to polyp detection. Five prior studies
have compared adenoma detection rate between standard and high definition white light colonoscopy with conflicting results. There have been methodological and technical differences between the studies (Table 4)
| Study | Date | Method | n | Colonoscope (resolution) (Angle) (NBI capable) | P value for adenomadetection rates | |
| Group 1 | Group 2 | |||||
| East et al[13] | 2008 | Prospective nonrandomized | 130 | Olympus SD 140 | Olympus HD 140 | 0.200 |
| Pellise et al[12] | 2008 | Prospective randomized | 620 | Olympus SD 140 | Olympus HD 170 | 0.850 |
| Tribonias et al[14] | 2010 | Prospective randomized | 390 | Olympus SD 140 | Olympus HD 170 | 0.160 |
| Burke et al[16] | 2010 | Retrospective | 852 | Olympus SD 140 | Olympus HD 170 | 0.360 |
| Buchner et al[15] | 2010 | Retrospective | 2430 | Olympus SD 140 | Olympus HD 170 NBI | 0.012 |
with all using Olympus colonoscopes, whereas our study
is the first performed using Fujinon HDC with FICE. Among the three prospective studies, Pellisé et al[12] had the largest patient population. It was a prospective randomized controlled trial of 620 patients conducted in Spain involving seven colonoscopists. Patients were randomized to either HDC with wide angle (170°) field or SDC with 140° view, with the investigators finding no difference in adenoma detection rate between the study groups (HDC 26% vs SDC 25%, P = 0.85). The study by East et al[13] was not randomized, consisting of 130 patients who underwent either HDC with 140° view or SC 140° view by a single colonoscopist. Although HDC did not improve the yield of adenomatous polyp detection, there was a trend in this direction (71% vs 60%). The Tribonias et al[14] study randomized 390 patients prospectively into HDC with wide angle vs SDC groups and, although there was a significant difference between the two groups with regards to overall rate of polyp detection, (HDC 63% vs SDC 53%, P = 0.03), there was no significant difference demonstrated in the detection of rate of adenomas (HDC 58% vs SDC 50%, P = 0.16).
The largest patient population study on this topic, by Buchner et al[15], was retrospective involving 2430 patients in two arms: HDC and SDC. The HRC were 170° wide-angle and NBI was used as needed. The SDC in the study had a 140° view and did not have NBI. The study found that the HDC were able to detect a statistically significant higher number of adenomatous polyps compared with SDC (28.8% vs 24.3%, P = 0.012). The most recently published study was by Burke et al[16] and consisted of 426 individuals in each group and found no advantage of HDC in overall polyp detection rate, adenomas or advanced adenomas.
In our study, we found no difference in detection rates of overall polyps, adenomas, advanced adenomas, and cancer between the HD and SD groups. There was no difference in polyp detection rates when each individual endoscopist’s HD and SD detection rates were compared despite having used 32-inch LCD high-resolution monitors with the Fujinon system whereas 19-inch CRT monitors were used with the standard definition colonoscopes. Although there are considerable methodological differences between the Pellisé et al[12] and our study, both studies show very similar results and conclusions. In fact, their adenomatous polyp detection rates are nearly identical to ours in the SD and HD arms: 0.45 ± 1.07 vs our 0.41 ± 1.04 adenomas per patient in SD and 0.43 ± 0.87 vs our 0.42 ± 0.94 adenomas per patient in HD. Our polyp detection rates are well in line with several other studies of white light colonoscopy with regards to prevalence of adenomas, advanced adenomas, cancer, and gender differences[17-19]. We were also able to demonstrate that polyp detection rate did not improve as the endoscopist experience with HDC increased by comparing adenoma detection in consecutive groups of 50 colonoscopies (P > 0.05). This lack of learning effect was also demonstrated by Adler et al[20] in 2008 in a prospective randomized study of NBI vs conventional colonoscopy for adenoma detection. Although prior studies were meant to compare HD and SD, the HD equipment used in these reports also had a wide angle field of view and the study by East is the only one that used 140° scopes in both arms, but it was underpowered for detecting small differences in polyp detection rate. Similar to East, our study design eliminates the confounding factor of the wide angle field of view by using 140° scopes in the HD and SD groups.
There is significant variability amongst endoscopists in adenoma detection rates, making the endoscopist probably the most important variable in adenoma detection rate[21]. We tried to minimize the impact factor of the endoscopist by assigning an equal number of overall cases per endoscopist (300) and dividing these equally amongst the study groups. Our study has a significant advantage in this.
It can be argued that our study’s retrospective design was a limitation, but it may have also served to reduce endoscopist bias. Endoscopist bias is an inherent limitation of nearly all prospective colonoscopy study designs since the equipment cannot be hidden from the performer of the examination. A second limitation is that the population was a mixed-risk sample and there were slight differences with respect to Hispanics and screening patients. However, there was no statistically significant difference in the detection of adenoma, advanced adenoma or cancer between the Hispanic vs Non-Hispanic and screening vs non-screening groups. In fact, there was a slightly higher prevalence of adenomas in the populations that were overrepresented in the HD group. This would have worked to bias the results in favor of HDC had it been a significant difference. In summary, the results of our study are relevant to most practices as the majority of the new colonoscopy equipment purchased in the future will have HD and NBI or multi-band imaging capabilities. Until recently, evidence regarding the potential of this new technology in improving yield of polyp detection was lacking. Complementing the results of Pellise, and Burke, our study concludes that HDC with multi-band imaging capability does not detect more total polyps, adenomas, advanced adenomas or cancer. For now at least, the endoscopist and not the equipment used, continues to be the major factor in polyp detection.
It is estimated that up to 15 million colonoscopies are performed annually in the United States. Colonoscopy and polypectomy have been estimated to prevent 50%-80% of colorectal cancers. A considerable effort is being spent on optimizing the yield of colonoscopy with respect to polyp detection. At present, high definition colonoscopy (HDC) is being widely adapted but whether or not it impacts detection of colon polyps is debatable.
HDC is widely touted by manufacturers to improve polyp detection. Yet, several studies have compared detection of polyps with standard definition colonoscopy (SDC) vs HDC with variation in results.
A major confounding factor in previous studies on this subject is that the endoscopists are aware of the high definition equipment and this may have led to bias in polyp detection rates. This study uniquely eliminates the issue of endoscopist bias by using a retrospective model of consecutive colonoscopies.
By providing added evidence of HDC’s role in polyp detection, this study may shift opinion further to the side of lack of benefit in improving yield.
Standard colonoscopes typically use 640 × 480 resolution monitors producing a 307, 200 pixel image. The HDC with high resolution monitors can produce a 1032 × 768 resolution and a 792, 576 pixel image.
The authors examined whether or not HDC resulted in detection of more polyps. The results show no significant difference in polyp detection between SDC and HDC. The results complement the conclusion of other recent studies in this field and suggest that high definition by itself may not improve yield of polyp detection.
| 1. | Seeff LC, Richards TB, Shapiro JA, Nadel MR, Manninen DL, Given LS, Dong FB, Winges LD, McKenna MT. How many endoscopies are performed for colorectal cancer screening? Results from CDC's survey of endoscopic capacity. Gastroenterology. 2004;127:1670-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 326] [Article Influence: 14.8] [Reference Citation Analysis (2)] |
| 2. | Seeff LC, Manninen DL, Dong FB, Chattopadhyay SK, Nadel MR, Tangka FK, Molinari NA. Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population in the United States? Gastroenterology. 2004;127:1661-1669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 197] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 3. | Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3107] [Cited by in RCA: 3177] [Article Influence: 96.3] [Reference Citation Analysis (1)] |
| 4. | Citarda F, Tomaselli G, Capocaccia R, Barcherini S, Crespi M. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut. 2001;48:812-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 511] [Cited by in RCA: 500] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 5. | Thiis-Evensen E, Hoff GS, Sauar J, Langmark F, Majak BM, Vatn MH. Population-based surveillance by colonoscopy: effect on the incidence of colorectal cancer. Telemark Polyp Study I. Scand J Gastroenterol. 1999;34:414-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 275] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 6. | Robertson DJ, Greenberg ER, Beach M, Sandler RS, Ahnen D, Haile RW, Burke CA, Snover DC, Bresalier RS, McKeown-Eyssen G. Colorectal cancer in patients under close colonoscopic surveillance. Gastroenterology. 2005;129:34-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 304] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 7. | Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1-8. [PubMed] |
| 8. | Rex DK, Cutler CS, Lemmel GT, Rahmani EY, Clark DW, Helper DJ, Lehman GA, Mark DG. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology. 1997;112:24-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1089] [Cited by in RCA: 1057] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 9. | Hixson LJ, Fennerty MB, Sampliner RE, Garewal HS. Prospective blinded trial of the colonoscopic miss-rate of large colorectal polyps. Gastrointest Endosc. 1991;37:125-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 181] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 10. | Heresbach D, Barrioz T, Lapalus MG, Coumaros D, Bauret P, Potier P, Sautereau D, Boustière C, Grimaud JC, Barthélémy C. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy. 2008;40:284-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 381] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 11. | Song LM, Adler DG, Conway JD, Diehl DL, Farraye FA, Kantsevoy SV, Kwon R, Mamula P, Rodriguez B, Shah RJ. Narrow band imaging and multiband imaging. Gastrointest Endosc. 2008;67:581-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 124] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 12. | Pellisé M, Fernández-Esparrach G, Cárdenas A, Sendino O, Ricart E, Vaquero E, Gimeno-García AZ, de Miguel CR, Zabalza M, Ginès A. Impact of wide-angle, high-definition endoscopy in the diagnosis of colorectal neoplasia: a randomized controlled trial. Gastroenterology. 2008;135:1062-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | East JE, Stavrindis M, Thomas-Gibson S, Guenther T, Tekkis PP, Saunders BP. A comparative study of standard vs. high definition colonoscopy for adenoma and hyperplastic polyp detection with optimized withdrawal technique. Aliment Pharmacol Ther. 2008;28:768-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Tribonias G, Theodoropoulou A, Konstantinidis K, Vardas E, Karmiris K, Chroniaris N, Chlouverakis G, Paspatis GA. Comparison of standard vs high-definition, wide-angle colonoscopy for polyp detection: a randomized controlled trial. Colorectal Dis. 2010;12:e260-e266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Buchner AM, Shahid MW, Heckman MG, McNeil RB, Cleveland P, Gill KR, Schore A, Ghabril M, Raimondo M, Gross SA. High-definition colonoscopy detects colorectal polyps at a higher rate than standard white-light colonoscopy. Clin Gastroenterol Hepatol. 2010;8:364-370. |
| 16. | Burke CA, Choure AG, Sanaka MR, Lopez R. A comparison of high-definition vs conventional colonoscopes for polyp detection. Dig Dis Sci. 2010;55:1716-1720. |
| 17. | Kanna B, Schori M, Azeez S, Kumar S, Soni A. Colorectal tumors within an urban minority population in New York City. J Gen Intern Med. 2007;22:835-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Schoenfeld P, Cash B, Flood A, Dobhan R, Eastone J, Coyle W, Kikendall JW, Kim HM, Weiss DG, Emory T. Colonoscopic screening of average-risk women for colorectal neoplasia. N Engl J Med. 2005;352:2061-2068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 344] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 19. | Adler A, Aschenbeck J, Yenerim T, Mayr M, Aminalai A, Drossel R, Schröder A, Scheel M, Wiedenmann B, Rösch T. Narrow-band versus white-light high definition television endoscopic imaging for screening colonoscopy: a prospective randomized trial. Gastroenterology. 2009;136:410-6.e1; quiz 715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 143] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 20. | Adler A, Pohl H, Papanikolaou IS, Abou-Rebyeh H, Schachschal G, Veltzke-Schlieker W, Khalifa AC, Setka E, Koch M, Wiedenmann B. A prospective randomised study on narrow-band imaging versus conventional colonoscopy for adenoma detection: does narrow-band imaging induce a learning effect? Gut. 2008;57:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 190] [Article Influence: 10.6] [Reference Citation Analysis (1)] |
| 21. | Chen SC, Rex DK. Endoscopist can be more powerful than age and male gender in predicting adenoma detection at colonoscopy. Am J Gastroenterol. 2007;102:856-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 310] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
Peer reviewer: Dr. Shinji Tanaka, Director, Department of Endoscopy, Hiroshima University Hospital, 1-2-3 Kasumi, Minami-ku, Hiroshima 734-8551, Japan.
S- Editor Sun H L- Editor Rutherford A E- Editor Xiong L