Published online Mar 7, 2010. doi: 10.3748/wjg.v16.i9.1158
Revised: December 6, 2009
Accepted: December 13, 2009
Published online: March 7, 2010
Transjugular intrahepatic portosystemic shunt (TIPSS) is considered a valid therapeutic option for the treatment of portal hypertension and its complications. The guidelines for this procedure have already been established on the basis of the normal vascular anatomy and of various technical radiological aspects. In some few rare cases, diagnosis of a congenital vascular anomaly can be made accidentally by interventional radiologists, making the procedure of the TIPSS placement extremely difficult or in some cases technically impossible. This report describes a rare vascular malformation characterized by the absence of the right superior vena cava and persistence of the left superior vena cava in a patient with a diagnosis of advanced liver cirrhosis who needed a TIPSS placement in order to control refractory ascites.
- Citation: Petridis I, Miraglia R, Marrone G, Gruttadauria S, Luca A, Vizzini GB, Gridelli B. Transjugular intrahepatic portosystemic shunt with accidental diagnosis of persistence of the left superior vena cava. World J Gastroenterol 2010; 16(9): 1158-1160
- URL: https://www.wjgnet.com/1007-9327/full/v16/i9/1158.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i9.1158
The transjugular intrahepatic portosystemic shunt (TIPSS) is a well known life saving procedure that is performed in patients with complications of portal hypertension, such as variceal bleeding and refractory ascites[1-5]. The standard technique for this treatment is the right internal jugular vein (RIJV) approach, although some authors have reported the left internal jugular vein (LIJV) approach when the RIJV is not available or cannot be used, due, for example, to vein thrombosis[6]. Few cases of patients with the absence of the right superior vena cava (RSVC) and the persistence of the left superior vena cava (LSVC) have been described in the literature[7]. Even if this is an extremely rare situation, it can create problems during the interventional procedure. We briefly report a case in which a TIPSS was successfully created in a patient with absence of RSVC and persistence of the LSVC.
A 69-year-old female with a diagnosis of hepatitis C virus-related cirrhosis was referred to our institute in order to be evaluated for a TIPSS placement because of refractory ascites. In the physical examination the patient had tense ascites despite a consistent use of high dose diuretics and periodic paracentesis (every 1-2 wk). She was well oriented to time and to space and had no episodes of portosystemic encephalopathy in the past. An abdominal computed tomography (CT) scan of the abdomen and a liver Doppler sonography (US) were performed excluding presence of hypervascular focal lesions in the liver and showing patency of the portal vein (PV). The CT scan also showed signs of portal hypertension such as tense ascites, presence of splenogastrorenal shunt, large esophageal and perigastric varices and patency of the umbilical vein. A large volume paracentesis was performed at admission with removal of almost 15 liters of clear ascites. No evidence of infection was found in the fluid (white blood cell count, Gram stain, and culture were negative).
The patient was hemodynamically stable with no need of inotropic drugs. Child-Pugh score was B-8 with a Meld score of 10. She had mild coagulopathy (international normalized ratio 1.4, platelet count 56 000/μL), but with good liver function tests (LFTs) (total bilirubin 1.29 mg/dL, albumin 3.4 g/dL). A transthoracic echocardiography showed no evidence of valvular heart disease, and the diameters of the cardiac chambers were within normal limits. Systolic and diastolic functions of the left ventricle were in the normal range. Estimated pulmonary vein pressure was 35 mmHg.
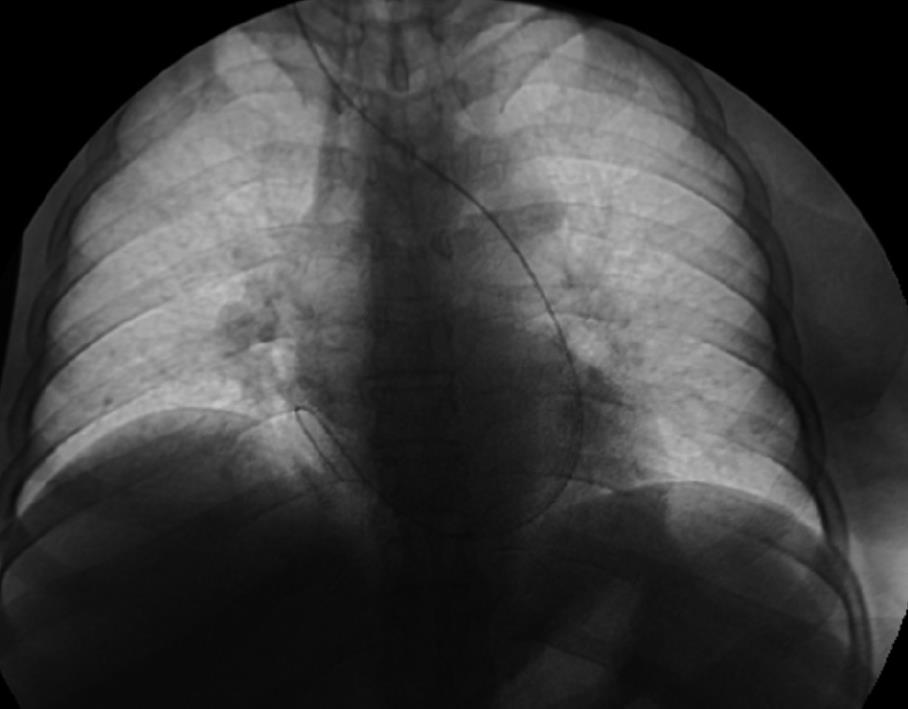
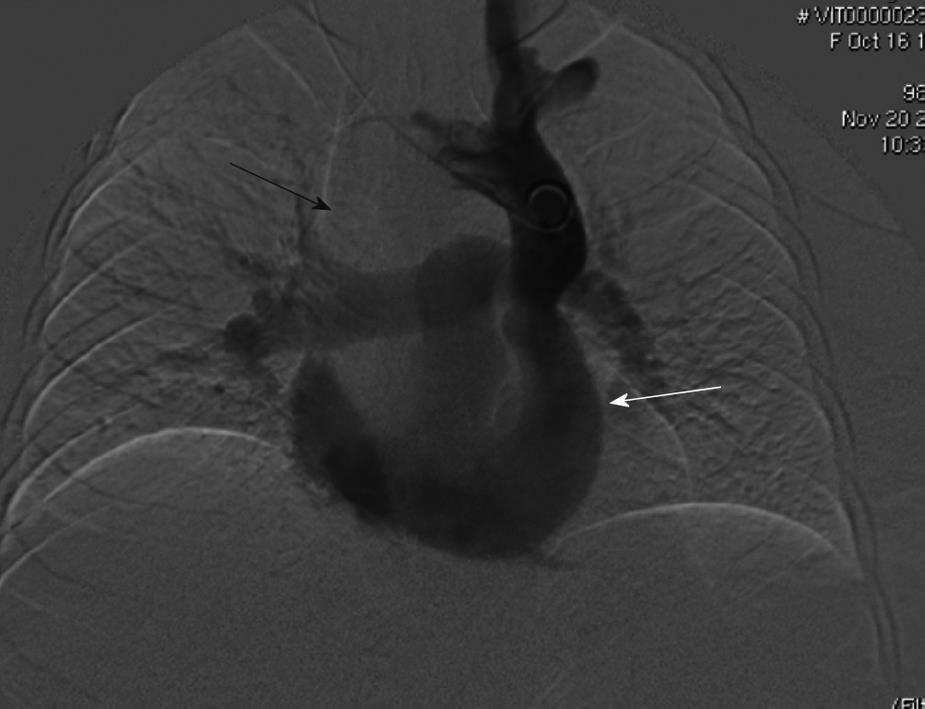
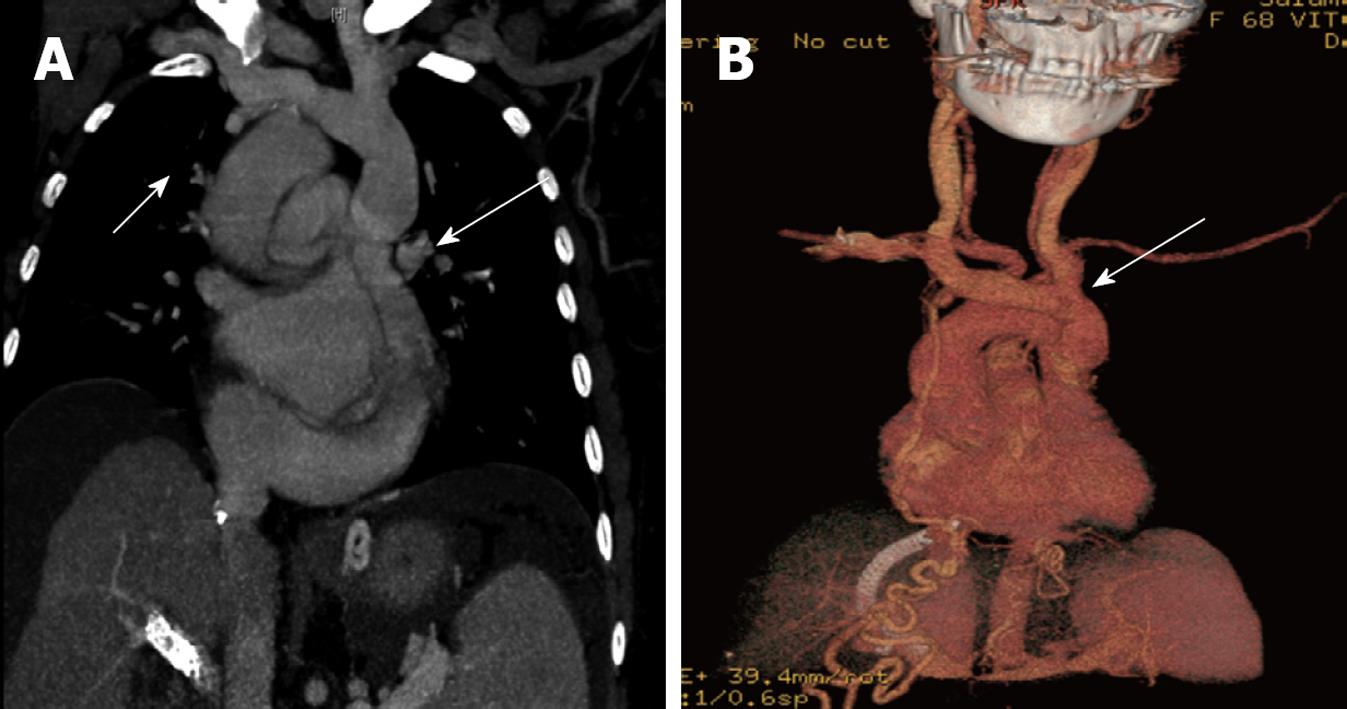
As a result, we decided to perform a TIPSS procedure in order to treat portal hypertension. The procedure was carried out in an angiographic suite under monitored anesthesia care. The right femoral artery was prepared, and an angiogram revealed patency of the superior mesenteric artery. In the venous phase the superior mesenteric and main portal vein were visualized. After sonographic guidance, the RIJV was cannulated, and under fluoroscopic guidance the metallic flexible guidewire was advanced and seen to curve to the left, until reaching the right atrium (Figure 1). A 5 French (F) pig tail catheter was advanced in the right atrium and a venogram revealed a patent LSVC that drained in the coronary sinus and an absent RSVC but in the presence of a viscero-atrial situs solitus (Figure 2). Because of the excessive curvature, which made insertion of the Colapinto needle impossible, we decided to use the LIJV and perform a new venogram. Under sonographic guidance, a new catheter was advanced through the LSVC and the coronary situs to the right atrium and from the inferior vena cava to the right hepatic vein. The Colapinto coaxial system was applied. The right branch of the main PV was punctured, under fluoroscopic guidance, and a 5F hydrophilic catheter was advanced over a hydrophilic guidewire. Portal hemodynamic measurements were performed and showed free hepatic vein pressure (FHVP) of 12.5 mmHg, right atrial pressure (RAP) of 12 mmHg, and portal vein pressure (PVP) of 23.5 mmHg. A shunt was created employing an 8-mm diameter Viattor-covered stent which was dilated with a 6-mm angioplasty balloon. New hemodynamic measurements showed FHVP of 14.5 mmHg, RAP of 14 mmHg and PVP of 19 mmHg. A venogram performed after the TIPSS placement showed patency of the stent (Figures 3 and 4) with reduction of the gradient from the portal vein to the right atrium from 11.5 mmHg before stent placement to 5 mmHg after stent placement.
A Doppler US control was performed the day after the TIPSS placement showing good patency and blood flow within the stent. The patient had a good post-procedure course with no complications and was discharged 48 h after the TIPSS creation.
Since then, the patient has had regular clinical and radiological follow-up, having a US exam of the TIPSS and laboratory tests every 3 mo. The last US exam was carried out 19 mo post-TIPSS creation showing patency of the TIPSS and absence of ascites. Currently the patient is doing well, her Child-Pugh score is B-7, with stable LFTx and no signs of hepatic decompensation.
Absence of the right SVC with persistent left SVC in viscero-atrial situs solitus is a rare congenital cardiovascular malformation and one of the most common rare thoracic vein anomalies. It is found in < 1% of the general population and in up to 10% of patients with congenital heart disease[8,9]. The first case was described in 1862 by Halbertsma[10].
This anomaly is usually diagnosed accidentally, for example, during anesthesiological procedures, such as central vein placement[7] or, more frequently, during diagnostic and therapeutic cardiovascular procedures, such as right heart catheterization or pacemaker placement[11,12]. Moreover, it may also emerge during cardiac procedures in pediatric patients (foramen ovale or atrial septal defect transcatheter closure).
Nowadays, TIPSS is considered to be a valid procedure for the treatment of complications of portal hypertension such as refractory ascites and variceal bleeding. The left internal jugular approach has been reported in previous studies[6]. To our knowledge, there are a few cases reported in the literature of successful TIPSS placement through the LSVC approach[13], some of them in patients with a diagnosis of “situs inversus totalis”[14,15]. Interventional radiologists should be aware of this rare, but possible, vascular anatomy, and understand that it may not represent an absolute contraindication for TIPSS insertion.
| 1. | Rosado B, Kamath PS. Transjugular intrahepatic portosystemic shunts: an update. Liver Transpl. 2003;9:207-217. |
| 2. | Hassoun Z, Pomier-Layrargues G. The transjugular intrahepatic portosystemic shunt in the treatment of portal hypertension. Eur J Gastroenterol Hepatol. 2004;16:1-4. |
| 4. | Wong F. The use of TIPS in chronic liver disease. Ann Hepatol. 2006;5:5-15. |
| 5. | Colombato L. The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension. J Clin Gastroenterol. 2007;41 Suppl 3:S344-S351. |
| 6. | Hausegger KA, Tauss J, Karaic K, Klein GE, Uggowitzer M. Use of the left internal jugular vein approach for transjugular portosystemic shunt. AJR Am J Roentgenol. 1998;171:1637-1639. |
| 7. | Ratliff HL, Yousufuddin M, Lieving WR, Watson BE, Malas A, Rosencrance G, McCowan RJ. Persistent left superior vena cava: case reports and clinical implications. Int J Cardiol. 2006;113:242-246. |
| 8. | Lenox CC, Zuberbuhler JR, Park SC, Neches WH, Mathews RA, Fricker FJ, Bahnson HT, Siewers RD. Absent right superior vena cava with persistent left superior vena cava: implications and management. Am J Cardiol. 1980;45:117-122. |
| 9. | Chandra A, Reul GJ Jr. Persistent left superior vena cava discovered during placement of central venous catheter. Tex Heart Inst J. 1998;25:90. |
| 10. | Halbertsma MJ. Abnormalitaet der vena cava superior. Ned Tijdschr Geneeskd. 1862;6:610-612. |
| 11. | Ashida Y, Mori T, Kuroda H, Ishiguro S, Hara Y, Tonomoto N. Transvenous dual chamber pacing via a unilateral left superior vena cava. Pacing Clin Electrophysiol. 1998;21:137-139. |
| 12. | Bartram U, Van Praagh S, Levine JC, Hines M, Bensky AS, Van Praagh R. Absent right superior vena cava in visceroatrial situs solitus. Am J Cardiol. 1997;80:175-183. |
| 13. | Bahramipour P, Abu-Judeh HH, Miller J. Transjugular intrahepatic portosystemic shunt placement in a patient with absent right superior vena cava and persistent left superior vena cava. AJR Am J Roentgenol. 1999;173:631-632. |
| 14. | Chovanec V, Krajina A, Lojík M, Hůlek P, Vanásek T. TIPS creation in a patient with situs inversus totalis. Cardiovasc Intervent Radiol. 2002;25:447-449. |
| 15. | Postoak DW, Ferral H, Washburn WK, Speeg KV, Wholey MH. Transjugular intrahepatic portosystemic shunt creation in a patient with situs inversus. J Vasc Interv Radiol. 2002;13:755-756. |
Peer reviewer: Hussein M Atta, MD, PhD, Department of Surgery, Faculty of Medicine, Minia University, Mir-Aswan Road, El-Minia 61519, Egypt
S- Editor Wang JL L- Editor Webster JR E- Editor Zheng XM