Published online Oct 7, 2010. doi: 10.3748/wjg.v16.i37.4747
Revised: May 31, 2010
Accepted: June 7, 2010
Published online: October 7, 2010
Gastrointestinal bleeding from small-bowel varices is a rare and difficult to treat complication of portal hypertension. We describe the case of a 79-year-old female patient with recurrent severe hemorrhage from small-bowel varices 30 years after a complicated cholecystectomy. When double balloon enteroscopy was unsuccessful to reach the site of bleeding, a rendezvous approach was favored with intraoperative endoscopy. Active bleeding from varices within a biliodigestive anastomosis was found and controlled by endoscopic injection of cyanoacrylate. Intraoperative endoscopy should be considered in the case of life-threatening gastrointestinal hemorrhage that is not accessible by conventional endoscopy.
- Citation: Brechmann T, Schmiegel W, Nicolas V, Reiser M. Gastrointestinal bleeding 30 years after a complicated cholecystectomy. World J Gastroenterol 2010; 16(37): 4747-4750
- URL: https://www.wjgnet.com/1007-9327/full/v16/i37/4747.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i37.4747
Hemorrhage from small-bowel varices is a rare but life-threatening condition. Despite sophisticated endoscopic techniques such as single- or double-balloon endoscopy, localization and treatment of the site of bleeding can be challenging. No controlled trials have evaluated the best strategies in these situations, however, successful endoscopic obliteration of jejunal varices by injection of cyanoacrylate has been described in individual case reports. We describe the rare case of a small-bowel variceal hemorrhage within a biliodigestive anastomosis in a 79-year-old female patient. Active bleeding was controlled by cyanoacrylate occlusion using an interdisciplinary approach.
A 79-year-old Caucasian woman was admitted to our hospital because of recurrent gastrointestinal bleeding. The patient had been well until 4 wk earlier when she presented to another hospital with melena and anemia (hemoglobin 7.2 g/dL). Upper and lower gastrointestinal endoscopy were negative without detection of the source of bleeding. Multiple units of blood were transfused. Repeated episodes of melena were observed during the following weeks and the patient was transferred to our department.
Two years earlier, a diagnosis of autoimmune hepatitis was made with a positive antinuclear antibody titer of 1:2000, however, no biopsy was performed for confirmation. She had received prednisone, which was tapered and discontinued. At the time of presentation, she received no immunosuppressive therapy and liver function tests were normal. Her former history included hypertension, minor depression and a complicated cholecystectomy approximately 30 years earlier.
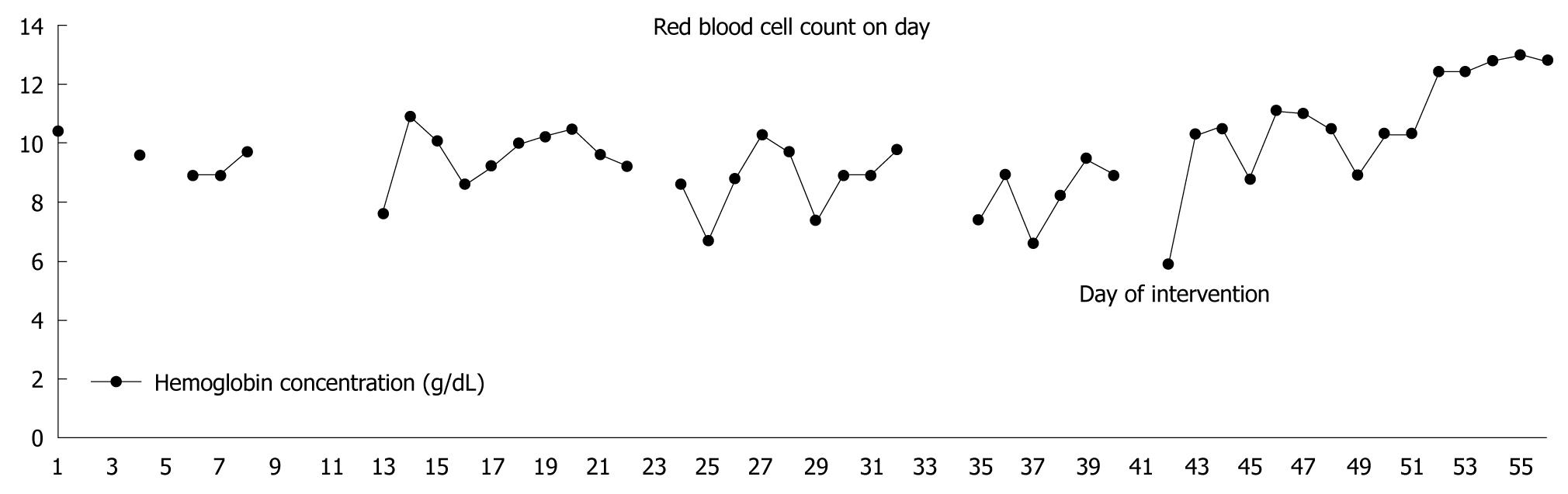
On admission to our hospital, the hemoglobin concentration was 10.4 g/dL. Rectal examination confirmed the presence of melena and a guaiac stool test was positive. Abdominal ultrasound showed a slightly enlarged liver with a prominent caudate lobe but normal echogenicity. Visualization of the hilar region and the pancreas was incomplete due to meteorism; the spleen was normal. Laboratory test results are shown in Table 1 and Figure 1.
| Laboratory test | On admission |
| Creatinine (mg/dL) | 1.0 |
| Potassium (mmol/dL) | 3.8 |
| Total protein (g/dL) | 3.4 |
| AST (U/L) | 25 |
| ALT (U/L) | 27 |
| γ-GT (U/L) | 22 |
| INR | 1 |
| RBC (g/dL) | 9.6 |
| WBC (/nL) | 5.5 |
| Platelets (/nL) | 290 |
| IgG (mg/dL) | 1140 |
| IgA (mg/dL) | 559 |
| IgM (mg/dL) | 98 |
| Reticulocytes (0.1%) | 41 |
| ANA, AMA, AMA-M2, LKM-1, SLA, ANCA | Negative |
| Ferritin (μg/L) | 9 |
| Cobalamine (ng/L) | 401 |
| Folic acid (μg/L) | 5.2 |
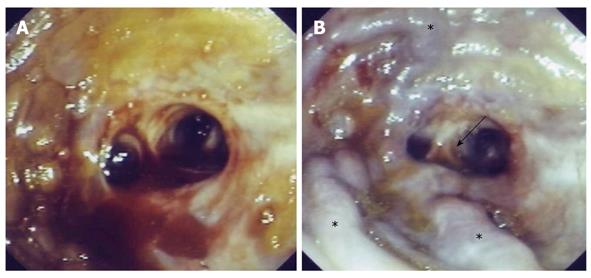
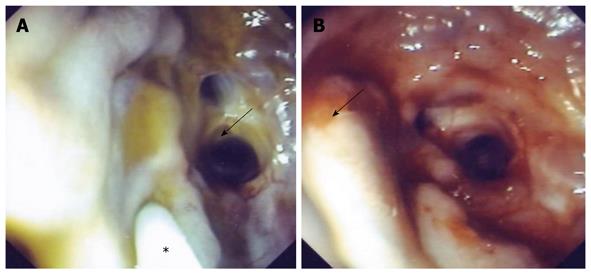
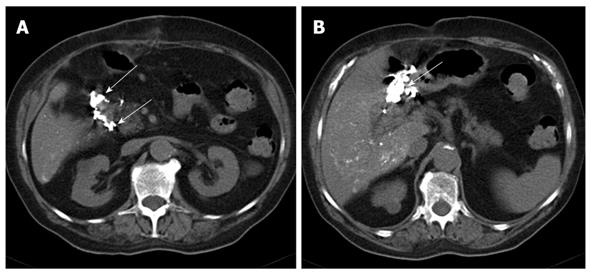
Repeated conventional upper and lower endoscopy did not detect the site of bleeding. An axial computed tomography (CT) scan of the abdomen showed air within the intrahepatic bile ducts, and cavernous transformation of the portal vein. Therefore, bleeding within a biliodigestive anastomosis was suspected and double balloon enteroscopy (Fuji) was performed. Approximately 180 cm aborally fresh blood was seen in the jejunum, however, a biliodigestive anastomosis or any other potential source of bleeding could not be detected. A decision was made to take the patient to the operating room, and a laparotomy with intraoperative colonoscopy was performed. An end-to-side biliodigestive anastomosis was detected with active bleeding from varices within the anastomosed small-bowel loop (Figures 2 and 3). N-butyl-2-cyanoacrylate (histoacryl) 1.0 mL mixed with lipiodol 1.0 mL was injected at two sites (total volume 2.0 mL), after which, bleeding stopped (Figures 2 and 3). A CT scan of the abdomen obtained 5 d after the intervention showed contrast-enhancing histoacryl-lipiodol deposits within the varices (Figure 4). The patient recovered uneventfully and was in good health with no signs of recurrent gastrointestinal bleeding and a normal hematocrit at 6 mo of follow-up.
Small-bowel varices can be found in approximately 8% of patients with portal hypertension using video capsule endoscopy[1]. Varices within jejunal anastomoses have been reported in anecdotal cases only[2]. Hemorrhage from jejunal varices, although a rare event, is often severe and can be fatal due to limited endoscopic access[3,4]. To the best of our knowledge, this could be the first description of hemorrhage from varices within a biliodigestive anastomosis.
Successful endoscopic obliteration of jejunal varices by injection of cyanoacrylate has been described in individual case reports[5,6]. Transjugular intrahepatic portosystemic shunt (TIPS) is another treatment option with demonstrated efficacy[7-10]. Cavernous transformation of the portal vein precluded decompression by TIPS in our case. In addition, surgical intervention would have carried a high risk of bleeding. As far as we are aware, no prospective trials have explored the management of small-bowel varices. Therefore, treatment must be individualized and depends on the experience of the team and availability of resources. Endoscopy can be considered the first-line approach, however, endoscopic access of the site of bleeding might be difficult, even with the use of push enteroscopy. If conventional endoscopy or push enteroscopy is unsuccessful, as in the present case, a rendezvous approach with intraoperative endoscopy should be considered to limit the extent of surgery. Our case demonstrates the efficacy and tolerability of histoacryl blockage for small-intestinal varices, which is a standard procedure in the stomach and esophagus.
| 1. | De Palma GD, Rega M, Masone S, Persico F, Siciliano S, Patrone F, Matantuono L, Persico G. Mucosal abnormalities of the small bowel in patients with cirrhosis and portal hypertension: a capsule endoscopy study. Gastrointest Endosc. 2005;62:529-534. |
| 2. | Tang SJ, Jutabha R, Jensen DM. Push enteroscopy for recurrent gastrointestinal hemorrhage due to jejunal anastomotic varices: a case report and review of the literature. Endoscopy. 2002;34:735-737. |
| 3. | Yuki N, Kubo M, Noro Y, Kasahara A, Hayashi N, Fusamoto H, Ito T, Kamada T. Jejunal varices as a cause of massive gastrointestinal bleeding. Am J Gastroenterol. 1992;87:514-517. |
| 4. | Joo YE, Kim HS, Choi SK, Rew JS, Kim HR, Kim SJ. Massive gastrointestinal bleeding from jejunal varices. J Gastroenterol. 2000;35:775-778. |
| 5. | Hekmat H, Al-toma A, Mallant MP, Mulder CJ, Jacobs MA. Endoscopic N-butyl-2-cyanoacrylate (Histoacryl) obliteration of jejunal varices by using the double balloon enteroscope. Gastrointest Endosc. 2007;65:350-352. |
| 6. | Getzlaff S, Benz CA, Schilling D, Riemann JF. Enteroscopic cyanoacrylate sclerotherapy of jejunal and gallbladder varices in a patient with portal hypertension. Endoscopy. 2001;33:462-464. |
| 7. | Shibata D, Brophy DP, Gordon FD, Anastopoulos HT, Sentovich SM, Bleday R. Transjugular intrahepatic portosystemic shunt for treatment of bleeding ectopic varices with portal hypertension. Dis Colon Rectum. 1999;42:1581-1585. |
| 8. | Kochar N, Tripathi D, McAvoy NC, Ireland H, Redhead DN, Hayes PC. Bleeding ectopic varices in cirrhosis: the role of transjugular intrahepatic portosystemic stent shunts. Aliment Pharmacol Ther. 2008;28:294-303. |
| 9. | Vangeli M, Patch D, Terreni N, Tibballs J, Watkinson A, Davies N, Burroughs AK. Bleeding ectopic varices--treatment with transjugular intrahepatic porto-systemic shunt (TIPS) and embolisation. J Hepatol. 2004;41:560-566. |
| 10. | Vidal V, Joly L, Perreault P, Bouchard L, Lafortune M, Pomier-Layrargues G. Usefulness of transjugular intrahepatic portosystemic shunt in the management of bleeding ectopic varices in cirrhotic patients. Cardiovasc Intervent Radiol. 2006;29:216-219. |
Peer reviewer: Seng-Kee Chuah, MD, Division of Hepatogastroenterology, Kaohsiung Chang Gang Memorial Hospital, 123, Ta-Pei Road, Niaosung Hsiang, Kaohsiung 833, Taiwan, China
S- Editor Wang YR L- Editor Kerr C E- Editor Ma WH