Published online Sep 28, 2010. doi: 10.3748/wjg.v16.i36.4594
Revised: May 10, 2010
Accepted: May 17, 2010
Published online: September 28, 2010
AIM: To evaluate the effect of double balloon endoscope (DBE) on the endoscopic retrograde cholangiopancreatography (ERCP) success rate in patients with a history of Billroth II (B II) gastrectomy.
METHODS: From April 2006 to March 2007, 32 patients with a B II gastrectomy underwent 34 ERCP attempts. In all cases, the ERCP procedures were started using a duodenoscope. If intubation of the afferent loop or reaching the papilla failed, we changed to DBE for the ERCP procedure (DBE-ERCP). We assessed the success rate of afferent loop intubation, reaching the major papilla, selective cannulation, possibility of therapeutic approaches, procedure-related complications, and the overall success rate.
RESULTS: Among the 32 patients with a history of B II gastrectomy, the duodenoscope was successfully passed up to the papilla in 22 patients (69%), and cannulation was successfully performed in 20 patients (63%). Six patients (2 with failure in afferent loop intubation and 4 with failure in reaching the papilla) underwent DBE-ERCP. The DBE reached the papilla in all the 6 patients (100%) and selective cannulation was successful in 5 patients (83%). Four patients (67%) who had common bile duct stones were successfully treated. One patient underwent diagnostic ERCP only and the other one, in whom selective cannulation failed, was diagnosed with papilla cancer proven by biopsy. There were no complications related to the DBE. The overall ERCP success rate increased to 88% (28/32).
CONCLUSION: The overall ERCP success rate increases with DBE in patients with a previous B II gastrectomy.
- Citation: Lin CH, Tang JH, Cheng CL, Tsou YK, Cheng HT, Lee MH, Sung KF, Lee CS, Liu NJ. Double balloon endoscopy increases the ERCP success rate in patients with a history of Billroth II gastrectomy. World J Gastroenterol 2010; 16(36): 4594-4598
- URL: https://www.wjgnet.com/1007-9327/full/v16/i36/4594.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i36.4594
Endoscopic retrograde cholangiopancreatography (ERCP) is an important procedure for the diagnosis and treatment of hepatobiliary and pancreatic diseases. The ERCP success rate exceeds 95% in patients with a normal gastrointestinal anatomy[1,2]. ERCP is also increasingly carried out in patients with a history of Billroth II (B II) gastrectomy, but its success rate in this group of patients is low (60%-92%)[3-7]. This procedure is more difficult because of problems encountered in entering the afferent loop, maneuvering the endoscope through the afferent loop to reach the major papilla, retrograde cannulation of the common bile duct, and performing an endoscopic sphincterotomy (EST) in a reverse direction[3,4]. The traditional examination method, using a side-viewing duodenoscope, is not always successful in some of these patients. If percutaneous transhepatic cholangiography and drainage (PTCD) or repeat surgery is not possible when the traditional method fails, double balloon endoscope (DBE) may be an excellent alternative treatment for these patients.
DBE was first introduced by Yamamoto et al[8] in 2001 as a novel endoscopic technique that allows examination of the entire small bowel. Presently, DBE is not only applied in diagnosis but also in endoscopic therapeutic interventions such as argon plasma coagulation for hemostasis, polypectomy, balloon dilation of small bowel strictures, and placement of enteral stents[9-12]. ERCP using DBE has been performed in patients with Roux-en-Y anastomosis[13-16], demonstrating that DBE system can be used to perform ERCP in patients with a surgically altered anatomy. In this paper, we describe the use of DBE in the ERCP procedure (DBE-ERCP) to increase the overall ERCP success rate in patients with a history of B II gastrectomy. In these patients, the ERCP procedure using a traditional duodenoscope was unsuccessful after afferent loop intubation or reaching the major papilla with a long afferent loop failed.
The study was approved by the Ethics Committee of the Chang Gung Memorial Hospital. From April 2006 to March 2007, ERCP procedure was performed for 968 patients in our therapeutic endoscopy center. Of the 968 patients, 32 (21 men and 11 women) who had a previous B II gastrectomy underwent 34 ERCP attempts (3.5%). The mean age of these 32 patients was 75.8 years (range 45-91 years). The procedure was always started with a side-viewing duodenoscope. If afferent loop intubation or reaching the papilla using the traditional duodenoscope was not possible, we changed to DBE for the ERCP procedure.
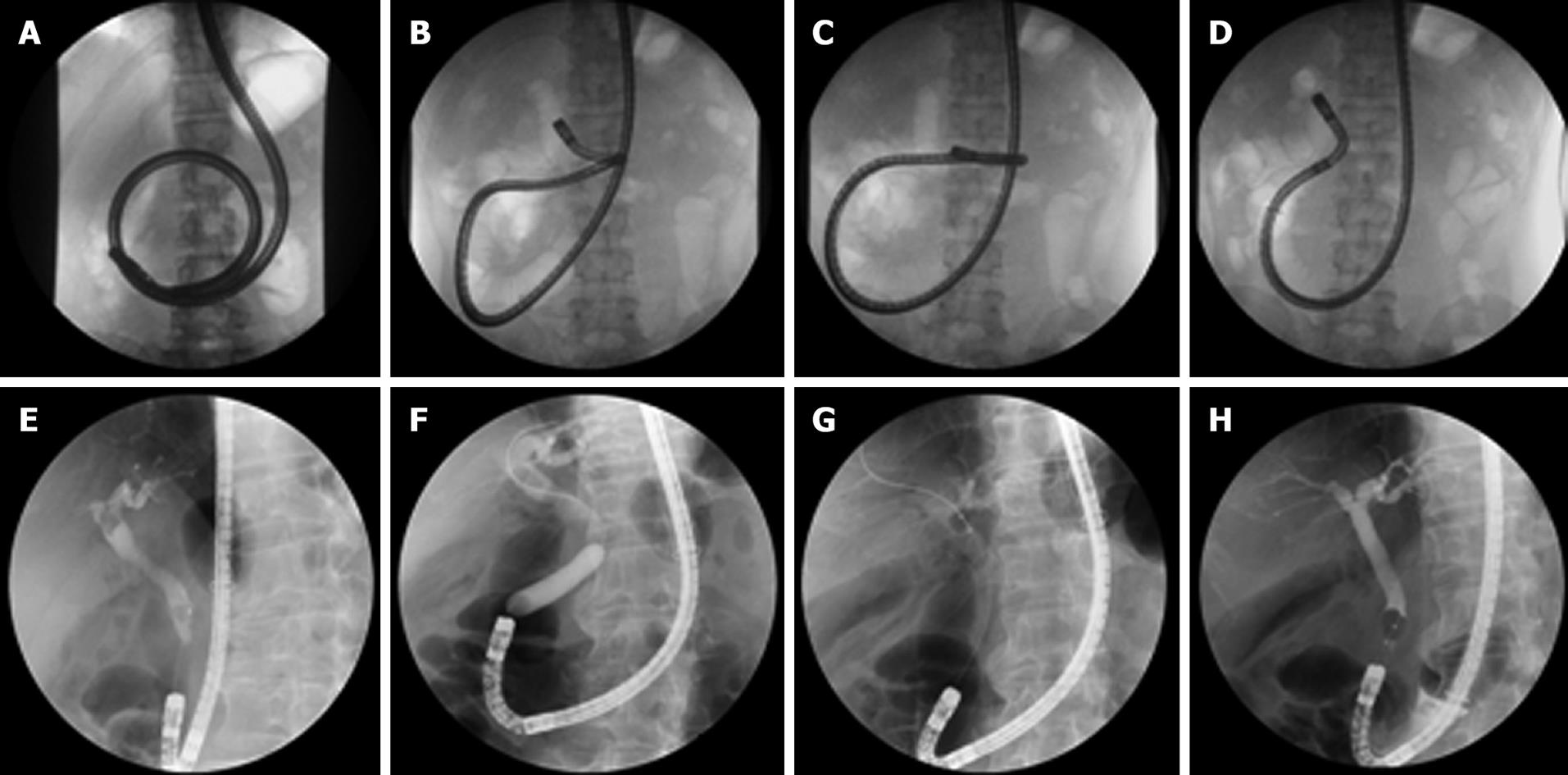
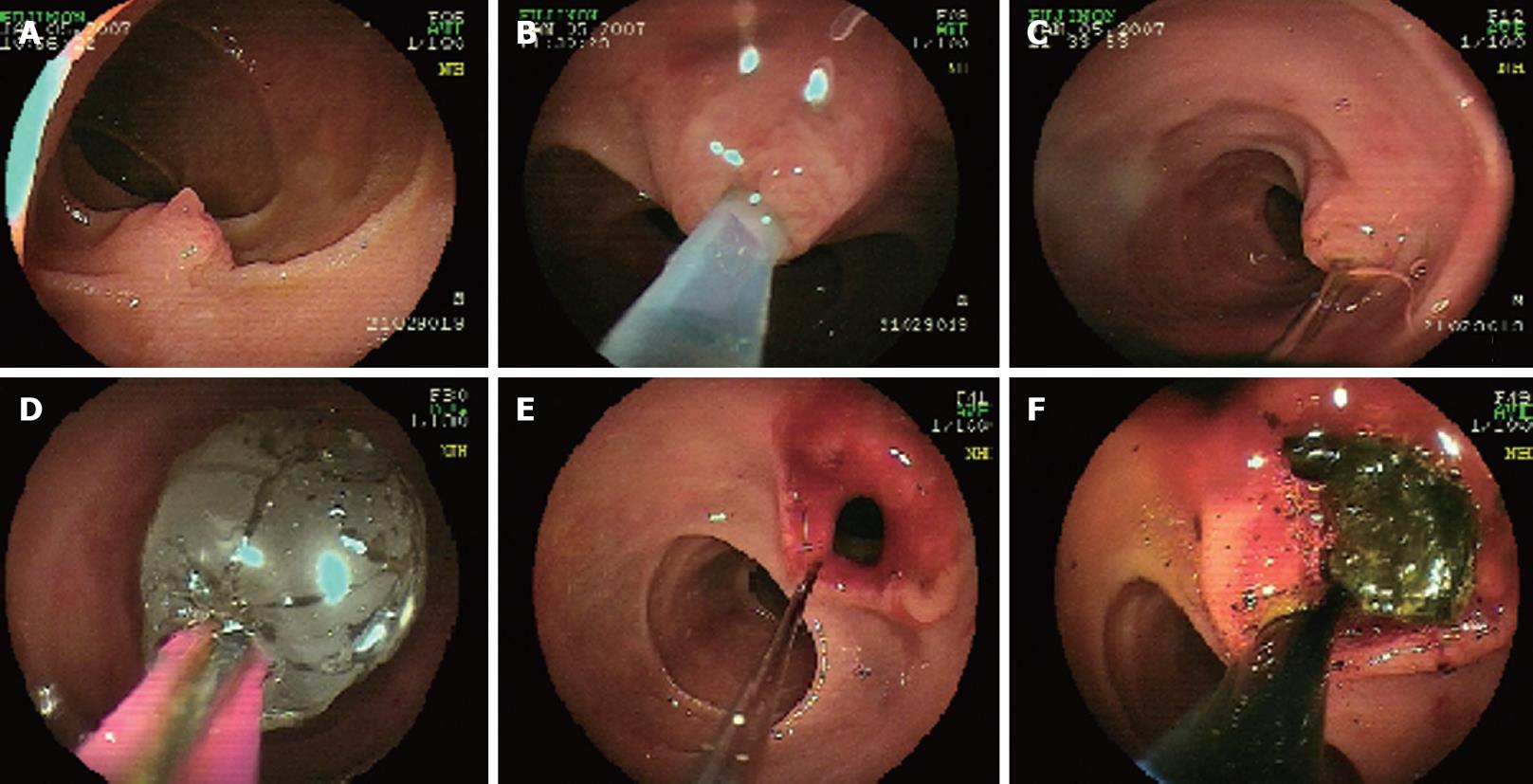
The DBE-ERCP procedure was performed using a 200-cm-long Fujinon double balloon endoscopy system which is 9.4 mm in diameter (EN-450 T5/W, Fuji Photo Optical Co., Ltd., Omiya, Japan). This double balloon endoscope has a 2.8-mm accessory channel through which therapeutic interventions may be carried out. Biliary cannulation was achieved using a long catheter (Glo-tip ERCP catheter, GT-1-TE, 320-cm, Cook Endoscopy, Winston-Salem, NC) and a long Axcess 21 guide wire (AX-21-650E, 650-cm, Cook Endoscopy, Winston-Salem, NC). After successful biliary cannulation, a controlled radial expansion (CRE) balloon dilation catheter (Boston Scientific Corporation, Natick, MA) was used for endoscopic papillary balloon dilation (EPBD). A long extraction balloon (ESCORT II double lumen extraction balloon, EBL-18-320E, 320-cm, Cook Endoscopy) was used for retrieval of biliary stones. Fluoroscopic pictures of the DBE-ERCP procedure are shown in Figure 1, and endoscopic pictures are shown in Figure 2.
The endoscopic procedure was performed under conscious sedation with midazolam (median dose 3.5 mg, range 2-6 mg), and pethidine (median dose 40 mg, range 30-60 mg). The DBE-ERCP was performed using a standard push-and-pull technique. The patients were placed in the prone position with their blood pressure, heart rate, and pulse oximetry monitored. Oxygen was administered if its saturation level dropped below 90%. The DBE-ERCP technique was explained to the patients and their family members. Written informed consent was obtained from all patients.
Among the 32 patients with a history of B II gastrectomy, the side-viewing duodenoscope was successfully passed up to the papilla in 22 patients (69%), and a successful cannulation was performed in 20 patients (63%). Two patients in whom selective biliary cannulation (n = 2, 6%) failed were successfully treated with a rendezvous technique. ERCP using a duodenoscope was unsuccessful in 10 patients (31%) when afferent loop intubation (n = 2, 6%), or in reaching the papilla failed because of a long afferent loop (n = 6, 19%), or endoscope-related small bowel perforation (n = 2, 6%) (Table 1).
| Characteristic | n (%) |
| Endoscope successfully reached the papilla | 22 (69) |
| Successful cannulation | 20 (63) |
| Cannulation by the rendezvous technique | 2 (6) |
| Failed attempt | 10 (31) |
| Failure in afferent loop intubation | 2 (6) |
| Failure in reaching to the papilla | 6 (19) |
| Endoscope-related perforation | 2 (6) |
Of the 8 patients (2 with failure in afferent loop intubation and 6 with failure in reaching the papilla, excluding those with perforation) who underwent ERCP using DBE, 2 were excluded because they refused to undergo DBE-ERCP since it was not covered by our national health insurance. The main indications for ERCP using DBE were biliary stones (n = 3, 50%), painless jaundice (n = 1, 17%), biliary pancreatitis (n = 1, 17%), and a dilated bile duct (n = 1, 17%). The DBE reached the papilla in all the 6 patients (100%). Selective cannulation and endoscopic treatment were successful in 5 patients (83%, 4 with bile duct stones and 1 underwent diagnostic ERCP). A biopsy for the diagnosis of papilla of Vater tumor was needed in the remaining patients. There were no immediate or short-term complications related to the DBE-ERCP. Therapeutic interventions using DBE were EBPD with stone extraction in 4 patients (66%), papilla of Vater tumor biopsy in 1 patient (17%), and diagnostic ERCP in 1 patient (17%). The overall success rate of traditional side-viewing duodenoscopic ERCP and DBE-ERCP was 69% (22/32) and 88% (28/32), respectively, in the patients with a history of B II gastrectomy.
Because of anatomical changes, ERCP is more challenging in patients who have undergone B II gastrectomy. The success rate of ERCP is lower in such patients than in those with a normal gastrointestinal anatomy[3-7]. ERCP is difficult because endoscopists encounter problems in afferent loop intubation, reaching the papilla, selective cannulation, and performing an EST in a reverse direction[3,4]. ERCP for patients with a history of B II gastrectomy is associated with a higher rate of perforation and other complications due to the above mentioned technical difficulties. It was reported that the overall complication, perforation, and mortality rates are 8%-13%, 0.6%-11%, and 1%, respectively[3-5,17-19].
In our series, the side-viewing duodenoscope was successfully passed up to the papilla in 69% of the patients with a history of B II gastrectomy, and the cannulation was successful in 63% of the patients. Six percent of the patients who failed in selective biliary cannulation were successfully treated with the rendezvous technique. ERCP using the duodenoscope was unsuccessful in 31% of the patients when afferent loop intubation and reaching the papilla failed, or endoscope-related small bowel perforation occurred in 6%, 19%, and 6% of the patients, respectively. The perforations, detected immediately after the procedure, usually occurred due to endoscope looping and over-manipulation, which caused tearing of the jejunal wall rather than direct perforation by the scope tip. Kim et al[7] have published a comparative study on the use of forward-viewing endoscope and side-viewing duodenoscope for ERCP in patients with a history of B II gastrectomy, and found that side-viewing duodenoscope leads to considerably more bowel perforations, indicating that it may be safer to use a forward-viewing endoscope when a ERCP is performed for patients with a history of B II gastrectomy. However, we prefer to use a side-viewing duodenoscope first, which allows the endoscopist to view the papilla en face. During therapeutic interventions such as EST, stenting, EPBD, and stone extraction, the manipulation of accessories is much easier using the elevator.
PTCD or surgery may be too invasive for patients in whom the afferent loop cannot be entered because of a sharp gastrojejunal anastomotic curve or the papilla cannot be reached because of the long afferent loop using a duodenoscope. In these cases, DBE is an excellent alternative treatment modality. DBE is a novel endoscopic procedure that allows examination of the entire small bowel in non-surgical patients[8]. In addition, it has been used for diagnostic and therapeutic ERCP in patients with Roux-en-Y anastomosis[13-16], demonstrating that the DBE system can be used to perform ERCP in patients with a surgically altered anatomy. Most of the complications that occur in patients with a history of B II gastrectomy during ERCP examination with a duodenoscopy are due to the tortuous afferent loop and over-manipulation of the duodenoscope. The advantage of DBE is that the push-and-pull method can overcome the sharp angulation of the anastomosis, and shorten the tortuous and long afferent loop. In addition, too much pressure on the small bowel wall can be avoided, and the endoscope can be inserted more smoothly and deeply. The DBE method can also avoid some complications of duodenoscopic ERCP, such as perforation.
In the present study, the overall success rate of traditional side-viewing duodenoscopic ERCP and DBE-ERCP was 69% and 88%, respectively, in the patients with a history of B II gastrectomy. Our study has some limitations, such as a small number of patients, and the study conducted at a single center. Multicenter, controlled studies are needed to confirm our results.
In conclusion, DBE can be used in ERCP for patients with a history of B II gastrectomy due to failure in afferent loop intubation or reaching the papilla using the traditional duodenoscope, and is a useful, safe, and effective procedure for diagnosis and therapeutic interventions. The procedure increases the overall success rate of ERCP in this group of patients.
Performing endoscopic retrograde cholangiopancreatography (ERCP) for patients with a history of Billroth II (B II) gastrectomy is more difficult because of problems encountered in afferent loop intubation, reaching the papilla, selective cannulation and sphincterotomy.
This is the first study using the double balloon endoscopy (DBE) for ERCP (DBE-ERCP) to increase the overall ERCP success rate in patients with a history of B II gastrectomy.
From the literature review, the success rate of ERCP is lower in patients with a history of B II gastrectomy than in those with a normal gastrointestinal anatomy. The results of this study demonstrate that the overall success rate of traditional side-viewing duodenoscopic ERCP and DBE-ERCP was 69% and 88%, respectively, for the patients with a history of B II gastrectomy.
The results of this study suggest that using DBE for ERCP in patients with a history of B II gastrectomy, when afferent loop intubation or reaching the papilla using the traditional duodenoscope fails, is a useful, safe, and effective procedure for diagnosis and therapeutic interventions.
This manuscript, describing experiences of the authors in performance of the "DBE-ERCP", corresponds to a series of patients and the analysis of their results. As a conclusion, this is an interesting manuscript that describes and comments the results obtained by the authors with DBE-ERCP.
| 1. | Vaira D, D'Anna L, Ainley C, Dowsett J, Williams S, Baillie J, Cairns S, Croker J, Salmon P, Cotton P. Endoscopic sphincterotomy in 1000 consecutive patients. Lancet. 1989;2:431-434. |
| 2. | Farrell RJ, Howell DA, Pleskow DK. New technology for endoscopic retrograde cholangiopancreatography: improving safety, success, and efficiency. Gastrointest Endosc Clin N Am. 2003;13:539-559. |
| 3. | Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986;27:1193-1198. |
| 4. | Forbes A, Cotton PB. ERCP and sphincterotomy after Billroth II gastrectomy. Gut. 1984;25:971-974. |
| 5. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. |
| 6. | Hintze RE, Veltzke W, Adler A, Abou-Rebyeh H. Endoscopic sphincterotomy using an S-shaped sphincterotome in patients with a Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:74-78. |
| 7. | Kim MH, Lee SK, Lee MH, Myung SJ, Yoo BM, Seo DW, Min YI. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29:82-85. |
| 8. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. |
| 9. | May A, Nachbar L, Wardak A, Yamamoto H, Ell C. Double-balloon enteroscopy: preliminary experience in patients with obscure gastrointestinal bleeding or chronic abdominal pain. Endoscopy. 2003;35:985-991. |
| 10. | Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006;38:42-48. |
| 11. | Mönkemüller K, Weigt J, Treiber G, Kolfenbach S, Kahl S, Röcken C, Ebert M, Fry LC, Malfertheiner P. Diagnostic and therapeutic impact of double-balloon enteroscopy. Endoscopy. 2006;38:67-72. |
| 12. | Ross AS, Semrad C, Waxman I, Dye C. Enteral stent placement by double balloon enteroscopy for palliation of malignant small bowel obstruction. Gastrointest Endosc. 2006;64:835-837. |
| 13. | Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66:1038-1041. |
| 14. | Haber GB. Double balloon endoscopy for pancreatic and biliary access in altered anatomy (with videos). Gastrointest Endosc. 2007;66:S47-S50. |
| 15. | Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068-1071. |
| 16. | Mönkemüller K, Bellutti M, Neumann H, Malfertheiner P. Therapeutic ERCP with the double-balloon enteroscope in patients with Roux-en-Y anastomosis. Gastrointest Endosc. 2008;67:992-996. |
| 17. | Cohen SA, Siegel JH, Kasmin FE. Complications of diagnostic and therapeutic ERCP. Abdom Imaging. 1996;21:385-394. |
| 18. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. |
Peer reviewer: De Aretxabala Xabier, Professor of Surgery, Universidad de Chile, Santos Dumont 999, Santiago, 8380000, Chile
S- Editor Wang JL L- Editor Wang XL E- Editor Zheng XM