Published online Sep 28, 2010. doi: 10.3748/wjg.v16.i36.4589
Revised: June 1, 2010
Accepted: June 8, 2010
Published online: September 28, 2010
AIM: To evaluate the therapeutic usefulness and safety of endoscopic resection in patients with gastric ectopic pancreas.
METHODS: A total of eight patients with ectopic pancreas were included. All of them underwent endoscopic ultrasonography before endoscopic resection. Endoscopic resection was performed by two methods: endoscopic mucosal resection (EMR) by the injection-and-cut technique or endoscopic mucosal dissection (ESD).
RESULTS: We planned to perform EMR in all eight cases but EMR was successful in only four cases. In the other four cases, saline spread into surrounding normal tissues and the lesions became flattened, which made it impossible to remove them by EMR. In those four cases, we performed ESD and removed the lesions without any complications.
CONCLUSION: If conventional EMR is difficult to remove gastric ectopic pancreas, ESD is a feasible alternative method for successful removal.
- Citation: Ryu DY, Kim GH, Park DY, Lee BE, Cheong JH, Kim DU, Woo HY, Heo J, Song GA. Endoscopic removal of gastric ectopic pancreas: An initial experience with endoscopic submucosal dissection. World J Gastroenterol 2010; 16(36): 4589-4593
- URL: https://www.wjgnet.com/1007-9327/full/v16/i36/4589.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i36.4589
Ectopic pancreas, also called heterotopic or aberrant pancreas, is defined as pancreatic tissue lying outside its normal location and lacking anatomic or vascular connections with the pancreas. It has been found in 0.6% to 13% of autopsies and has also been noted in approximately one of every 500 surgical operations involving the upper abdomen[1]. Ectopic pancreas is mostly found in the upper gastrointestinal tract adjacent to the pancreas; in 90% of patients with ectopic pancreas, it was found in the stomach, duodenum, or proximal part of the jejunum[2]. Histologic diagnosis of ectopic pancreas is usually difficult when tissue specimens are obtained using a standard endoscopic biopsy forceps[3].
Pathological diagnosis of ectopic pancreas is usually unachievable for two reasons: because adequate tissue samples cannot usually be taken during endoscopic biopsy using standard forceps[3] and because surgery is usually unnecessary for most asymptomatic patients. Recently, endoscopic ultrasonography (EUS) was reported to be helpful for diagnosing ectopic pancreas[4,5]. However, the accuracy of EUS for the diagnosis of subepithelial tumors is limited[6].
Most patients with ectopic pancreas are asymptomatic although a minority may present with a variety of symptoms, the most common being epigastric pain[7]. Options for treatment for gastric ectopic pancreas include observation, surgery[7,8], or endoscopic resection[6,9-11]. However, previous reports describing various methods of endoscopic resection were based on a limited number of cases. Therefore, we evaluated the therapeutic usefulness and safety of endoscopic resection in eight cases of gastric ectopic pancreas.
We retrospectively analyzed our database of all patients who underwent endoscopic resection at Pusan National University Hospital from July 2006 to December 2009. We identified a total of eight patients who were diagnosed as ectopic pancreas after endoscopic resection. All of them underwent EUS before endoscopic resection. This study was reviewed and approved by the Institutional Review Board at Pusan National University Hospital.
EUS was performed with a radial scanning 20 MHz catheter probe (UM3D-DP20-25R, Olympus, Tokyo, Japan). The probe was passed through the instrument channel of a one-channel endoscope (GIF-H260, Olympus) or a two-channel endoscope (GIF-2T240, Olympus). All examinations were performed under intravenous conscious sedation (midazolam with or without meperidine). Scanning of the lesion was performed after filling the stomach with 400-800 mL of deaerated water. EUS features of the lesions such as size, sonographic layer of origin, border appearance, echogenicity, and homogeneity were evaluated.
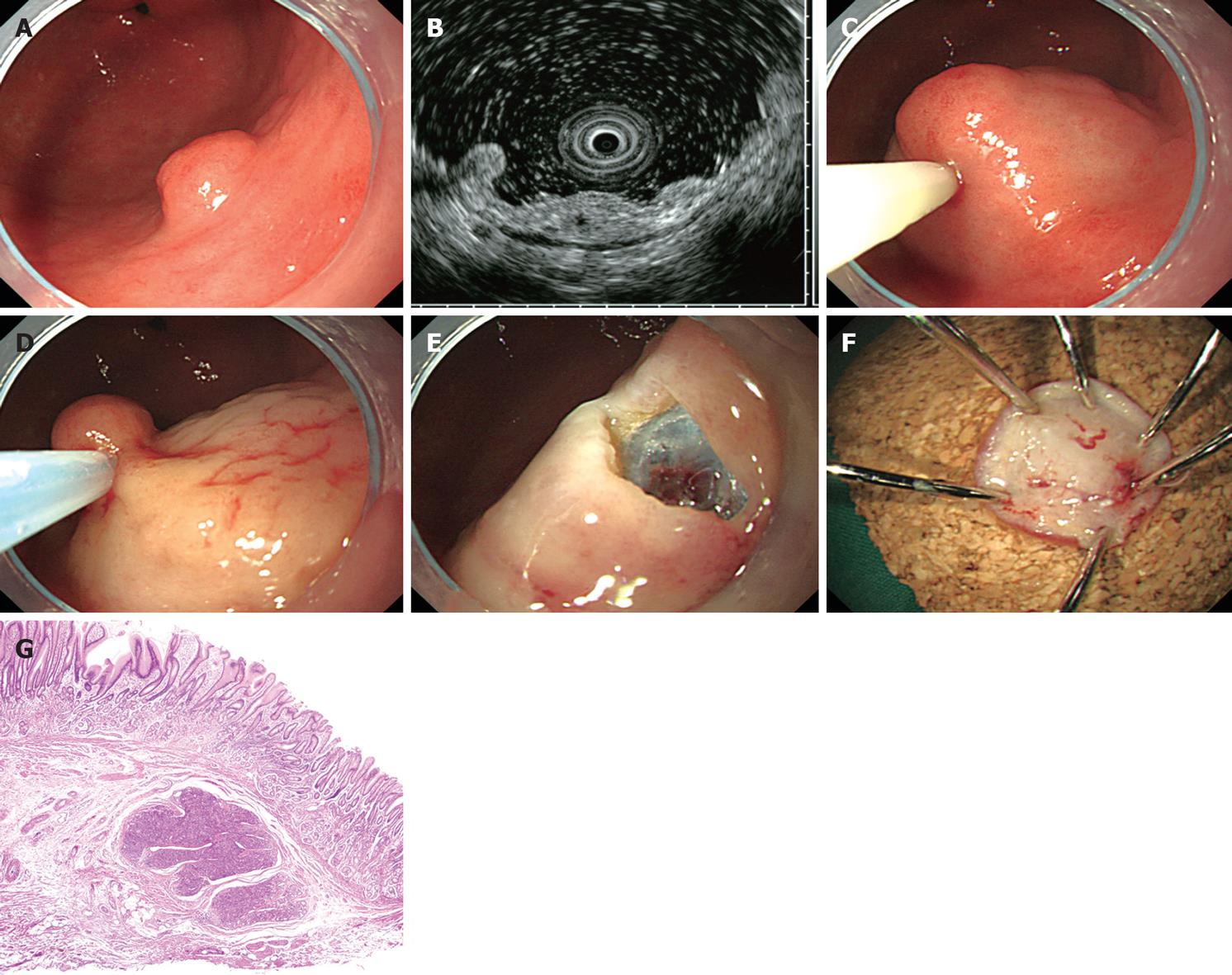
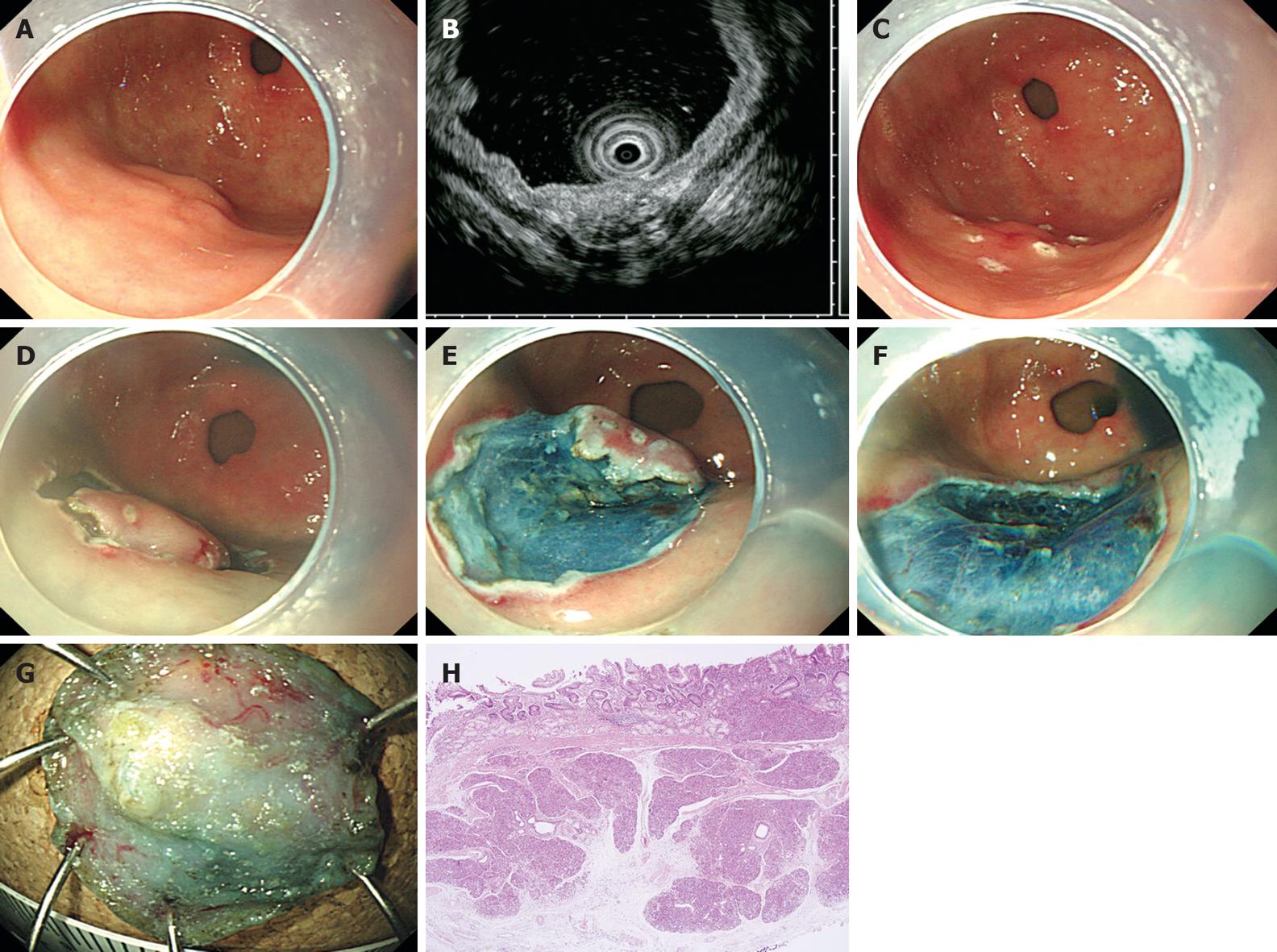
Endoscopic resection was performed by two methods. If the lesion was properly elevated after saline injection, endoscopic mucosal resection (EMR) was performed by the injection-and-cut technique (Figure 1). If the lesion was not properly elevated after saline injection, endoscopic mucosal dissection (ESD) was performed (Figure 2). First, the margins of the lesion were marked by needle knife and submucosal saline injection with a small amount of epinephrine (0.025 mg/mL) and indigo carmine was used to lift the lesion. Then, a circumferential incision into the submucosa and submucosal dissection was performed around the lesion with an insulation-tipped (IT) knife. After removal, the en bloc pathologic specimen was mounted and oriented to facilitate histologic examination.
The eight patients included one man and seven women and ranged in age from 18 to 57 years (mean, 36 years). Four patients presented with dyspepsia or epigastric pain. The subepithelial lesions were incidentally diagnosed in the other four patients without preceding symptoms. Five lesions were located at the antrum and three lesions were located at the lower body. None of the lesions showed endoscopic findings such as umbilication or central dimpling. Conventional biopsies were performed on five lesions, but none were diagnosed as ectopic pancreas as based on pathology.
According to EUS, the lesions were mainly located in the second (deep mucosal) or third (submucosal) layer and ranged from 6 to 12 mm (mean 8 mm) in size (Table 1). All lesions were hypoechoic; five lesions were homogenous and three lesions were heterogeneous. The border was distinct in five lesions (5/8, 62.5%) and indistinct in three lesions (3/8, 37.5%). An undulated margin was observed in six lesions (6/8, 75%) and anechoic cystic or tubular structures appeared in three lesions (3/8, 37.5%).
| Case | Sex | Age (yr) | Symptoms | Location | EUS features | Treatment | Follow-up period (mo) | |||||
| Layer | Size (cm) | Echogenicity | Homogenicity | Border | Anechoic area | |||||||
| 1 | F | 18 | Dyspepsia | Antrum | 2, 3 | 0.9 | Hypoechoic | Homogenous | Distinct | Absent | EMR | 28 |
| 2 | F | 44 | None | Antrum | 2, 3 | 0.6 | Hypoechoic | Homogenous | Distinct | Absent | EMR | 40 |
| 3 | F | 37 | None | Antrum | 3 | 0.7 | Hypoechoic | Heterogeneous | Indistinct | Absent | EMR | 35 |
| 4 | M | 45 | None | Lower body | 3 | 0.9 | Hypoechoic | Homogenous | Distinct | Present | EMR | 21 |
| 5 | F | 43 | None | Lower body | 3 | 0.8 | Hypoechoic | Homogenous | Distinct | Absent | ESD | 27 |
| 6 | F | 22 | Epigastric pain | Antrum | 3 | 0.6 | Hypoechoic | Heterogeneous | Indistinct | Present | ESD | 38 |
| 7 | F | 57 | Epigastric pain | Antrum | 2, 3 | 1.2 | Hypoechoic | Heterogeneous | Indistinct | Present | ESD | 26 |
| 8 | F | 24 | Dyspepsia | Lower body | 2, 3 | 0.9 | Hypoechoic | Homogenous | Distinct | Absent | ESD | 24 |
For accurate diagnosis of the subepithelial lesions, EMR was performed. To decrease the risk of perforation or bleeding, we first planned to remove the lesions by EMR. In all cases, we injected saline solution including a small amount of epinephrine and indigo carmine beneath the lesions. In four cases, the lesions were properly elevated and then were resected by the injection-and-cut technique. However, in the other four cases, the saline spread into surrounding normal tissue and the lesions became flattened, which made it impossible to remove the lesions via the injection-and-cut technique. Therefore, we decided to perform ESD on these four lesions and removed them successfully without any complications. There were no recurrences during the median follow-up period of 30 mo (range 24 to 40 mo).
Most patients with ectopic pancreas are asymptomatic, but symptoms may rarely occur due to the irritating effect of hormones and enzymes secreted by the ectopic pancreas[8]. Rare complications resulting from ectopic pancreas have been reported, including gastric outlet obstruction, obstructive jaundice, intestinal obstruction, and intussusceptions[8]. Asymptomatic patients with ectopic pancreas can generally be monitored with treatment reserved for patients who are symptomatic, have enlarging lesions or require diagnostic certainty.
Ectopic pancreas is most often detected as an incidental finding during routine upper endoscopy. The typical endoscopic finding is a firm round or oval subepithelial lesion with a central depression, which corresponds to the opening of a duct. The gross appearance of central dimpling or umbilication implies a presumptive diagnosis of ectopic pancreas during preoperative endoscopy[12]. The characteristic EUS features of ectopic pancreas, including indistinct margins, heterogeneous echogenicity (mainly hypoechoic accompanied by scattered small hyperechoic areas), presence of an anechoic area and fourth-layer thickening, and location within the second, third, and/or fourth layers are very useful for establishing a preoperative diagnosis of ectopic pancreas[4,12]. Heterogeneous hypoechoic or mixed echogenicity, resembling that of the normal pancreatic parenchyma, corresponds to the presence of acinous tissue with scattered adipose tissue within the lesion[4]. Anechoic areas indicate duct dilatation, and fourth-layer thickening is considered a consequence of the hypertrophy of the muscularis propria[4].
Although these endoscopic and EUS findings are suggestive of ectopic pancreas, the accuracy for the diagnosis of subepithelial tumors is limited[6,13]. In fact, none of our cases showed typical endoscopic findings such as central dimpling or umbilication and four of them did not exhibit a characteristic anechoic duct structure by EUS. Therefore, three lesions with anechoic duct structure were diagnosed as ectopic pancreas but the other five lesions, without anechoic duct structure, were suspicious as ectopic pancreas or were diagnosed as other diseases such as inflammatory fibrinoid polyp.
Histological diagnosis of ectopic pancreas is usually difficult when tissue specimens are obtained using conventional endoscopic biopsy forceps. For precise histological diagnosis, endoscopic techniques for obtaining deeper specimens are necessary, such as EUS-guided biopsy or combined strip biopsy and bite-on-bite biopsy[14-16]. Endoscopic removal of gastric ectopic pancreas is also useful for accurate diagnosis and treatment[11]. The diagnosis of ectopic pancreas was not made based on the pathological appearance of specimens taken with standard endoscopic biopsy forceps in any our cases.
EUS provides the most useful information regarding tumor location within the gastric wall, helps to distinguish subepithelial lesions, and assists in establishing indications for endoscopic removal[4]. Endoscopic removal of submucosal lesions, especially ESD, is considered dangerous because of the risk of perforation or bleeding[17]. There have only been a few reports describing EMR methods for gastric ectopic pancreas, such as strip biopsy[6,10], cap-assisted EMR[9,18], or ligation-assisted EMR[11]. In the present study, we first planned to remove the lesions by EMR and we therefore injected saline beneath the lesions. However, in four cases, we were forced to switch to ESD and removed the lesions without any complications. The current series, to our knowledge, is the first to describe the use of ESD for removal of gastric ectopic pancreas. Therefore, in cases for which conventional EMR is difficult or impossible, ESD may be used as an alternative method for successful removal of ectopic pancreas.
Ectopic pancreas is mostly found in the upper gastrointestinal tract adjacent to the pancreas; in 90% of patients with ectopic pancreas, it was found in the stomach, duodenum, or proximal part of the jejunum. Histologic diagnosis of ectopic pancreas is usually difficult when tissue specimens are obtained using a standard endoscopic biopsy forceps. Recently, endoscopic ultrasonography (EUS) was reported to be helpful for diagnosing ectopic pancreas. However, the accuracy of EUS for the diagnosis of subepithelial tumors is limited.
Options for treatment for gastric ectopic pancreas include observation, surgery, or endoscopic resection. There have only been a few reports describing endoscopic mucosal resection (EMR) for gastric ectopic pancreas, such as strip biopsy, cap-assisted EMR, or ligation-assisted EMR. In the present study, the authors first planned to remove the lesions by EMR and we therefore injected saline beneath the lesions. However, in some cases, they were forced to switch to endoscopic submucosal dissection (ESD) and removed the lesions without any complications. The current series is the first to describe the use of ESD for removal of gastric ectopic pancreas
To decrease the risk of perforation or bleeding, EMR is usually used to remove submucosal lesions. Usually saline solution including a small amount of epinephrine and indigo carmine is injected beneath the lesions. Then, the lesions are properly elevated and are resected by the injection-and-cut technique. However, in some cases, the saline spreads into surrounding normal tissue and the lesions become flattened, which makes it impossible to remove the lesions via the injection-and-cut technique. In these cases, ESD may be used as an alternative method for successful removal of subepithelial lesions.
When conventional EMR is difficult or impossible, ESD may be used as an alternative method for successful removal of subepithelial lesions such as ectopic pancreas.
Ectopic pancreas, also called heterotopic or aberrant pancreas, is defined as pancreatic tissue lying outside its normal location and lacking anatomic or vascular connections with the pancreas. It has been found in 0.6% to 13% of autopsies and has also been noted in approximately one of every 500 surgical operations involving the upper abdomen.
The paper is well written and easy to read. It is also well supported by excellent endoscopic images and pathology slides.
Peer reviewer: Dr. Massimo Raimondo, Division of Gastroenterology and Hepatology, Mayo Clinic, 4500 San Pablo Road, Jacksonville, FL 32224, United States
S- Editor Wang YR L- Editor O’Neill M E- Editor Ma WH
| 1. | DeBord JR, Majarakis JD, Nyhus LM. An unusual case of heterotopic pancreas of the stomach. Am J Surg. 1981;141:269-273. |
| 2. | Burke GW, Binder SC, Barron AM, Dratch PL, Umlas J. Heterotopic pancreas: gastric outlet obstruction secondary to pancreatitis and pancreatic pseudocyst. Am J Gastroenterol. 1989;84:52-55. |
| 3. | Yoshida T, Sakamoto A, Kuroki K, Kojo A, Watanabe H. Electrocoagulation biopsy of aberrant pancreas of the stomach. A case of aberrant gastric pancreas. Am J Gastroenterol. 1976;66:554-558. |
| 4. | Matsushita M, Hajiro K, Okazaki K, Takakuwa H. Gastric aberrant pancreas: EUS analysis in comparison with the histology. Gastrointest Endosc. 1999;49:493-497. |
| 5. | Kim JH, Lim JS, Lee YC, Hyung WJ, Lee JH, Kim MJ, Chung JB. Endosonographic features of gastric ectopic pancreases distinguishable from mesenchymal tumors. J Gastroenterol Hepatol. 2008;23:e301-e307. |
| 6. | Kojima T, Takahashi H, Parra-Blanco A, Kohsen K, Fujita R. Diagnosis of submucosal tumor of the upper GI tract by endoscopic resection. Gastrointest Endosc. 1999;50:516-522. |
| 7. | Lai EC, Tompkins RK. Heterotopic pancreas. Review of a 26 year experience. Am J Surg. 1986;151:697-700. |
| 8. | Ormarsson OT, Gudmundsdottir I, Mårvik R. Diagnosis and treatment of gastric heterotopic pancreas. World J Surg. 2006;30:1682-1689. |
| 9. | Faigel DO, Gopal D, Weeks DA, Corless C. Cap-assisted endoscopic submucosal resection of a pancreatic rest. Gastrointest Endosc. 2001;54:782-784. |
| 10. | Sun S, Wang M, Sun S. Use of endoscopic ultrasound-guided injection in endoscopic resection of solid submucosal tumors. Endoscopy. 2002;34:82-85. |
| 11. | Khashab MA, Cummings OW, DeWitt JM. Ligation-assisted endoscopic mucosal resection of gastric heterotopic pancreas. World J Gastroenterol. 2009;15:2805-2808. |
| 12. | Chen SH, Huang WH, Feng CL, Chou JW, Hsu CH, Peng CY, Yang MD. Clinical analysis of ectopic pancreas with endoscopic ultrasonography: an experience in a medical center. J Gastrointest Surg. 2008;12:877-881. |
| 13. | Brand B, Oesterhelweg L, Binmoeller KF, Sriram PV, Bohnacker S, Seewald S, De Weerth A, Soehendra N. Impact of endoscopic ultrasound for evaluation of submucosal lesions in gastrointestinal tract. Dig Liver Dis. 2002;34:290-297. |
| 14. | Vilmann P, Hancke S, Henriksen FW, Jacobsen GK. Endoscopic ultrasonography-guided fine-needle aspiration biopsy of lesions in the upper gastrointestinal tract. Gastrointest Endosc. 1995;41:230-235. |
| 15. | Karita M, Tada M. Endoscopic and histologic diagnosis of submucosal tumors of the gastrointestinal tract using combined strip biopsy and bite biopsy. Gastrointest Endosc. 1994;40:749-753. |
| 16. | Cantor MJ, Davila RE, Faigel DO. Yield of tissue sampling for subepithelial lesions evaluated by EUS: a comparison between forceps biopsies and endoscopic submucosal resection. Gastrointest Endosc. 2006;64:29-34. |
| 17. | Ponsaing LG, Hansen MB. Therapeutic procedures for submucosal tumors in the gastrointestinal tract. World J Gastroenterol. 2007;13:3316-3322. |
| 18. | Lee TH, Wang HP, Huang SF, Wang TH, Lin JT. Endoscopic mucosal resection for treatment of heterotopic pancreas in the stomach. J Formos Med Assoc. 1999;98:643-645. |