INTRODUCTION
Annular pancreas is a rare congenital anomaly, which consists of a ring of pancreatic tissue, confluent with the head of the pancreas, and partially or completely encircling the second segment of the duodenum. It was first described by Tiedemann in 1818[1] and first named “pancreas anulare “ by Ecker in 1862[2].
Studies based on cases where the diagnosis was made on autopsy or during surgery estimate the incidence of annular pancreas of 3 in 20 000[3,4]. When the diagnosis is based on modern imaging methods, such as multislice computed tomography (MSCT), magnetic resonance imaging (MRI), magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP), the incidence seems to be higher; up to 1 in 250[5,6]. About 700 cases of annular pancreas have been reported in the literature[7]. During normal organogenesis, the pancreas is formed by merging the ventral with the dorsal pancreatic bud during the first four to nine weeks of gestation. Two main theories, sustained by Lecco[8] and Badwin[9] respectively, describe the pathogenesis of annular pancreas. Lecco[8] explained the development of the anomaly as an adherence of the ventral pancreatic bud to the duodenum, which leads to an improper rotation of the ventral bud, resulting in the encirclement of the duodenum. Badwin[9] contends that the persistence and enlargement of the left ventral bud causes the pancreatic obstructing ring. Although the pancreatic band usually adheres to the muscularis of the duodenum, it may also be loosely applied to the serosa of the duodenum[10]. The annular pancreas has been associated with other congenital anomalies, such as trisomy 21, tracheoesophageal fistula, cardiac anomalies, and intestinal malrotation[7]. Association of annular pancreas with malignancy is rare. It has been described only 14 times in the English literature (five pancreatic carcinomas, six ampullary carcinomas, two cholangiocarcinomas, and one Insulinoma)[11-22]. A review of 151 cases of annular pancreas in Japan by Ogawa et al[11] revealed an association with malignant tumors of the duodenopancreatobiliary system in 15 patients (five cholangiocarcinomas, four gallbladder carcinomas, four duodenal, and two pancreatic carcinomas). Primary carcinoma of the duodenum is rare, representing about 0.3% of all malignant neoplasms of the gastrointestinal tract and 25%-45% of malignant neoplasms of the small intestine[23].
We report what is, to the best of our knowledge, the first case in the English literature of duodenal adenocarcinoma in a patient with annular pancreas.
CASE REPORT
A 55-year-old Caucasian woman was admitted to our hospital with a six-week history of persistent postprandial nausea and vomiting, associated with a weight loss of 7 kg compared to a total weight of 70 kg. There was no associated pain, hematemesis, fever, diarrhoea, or jaundice. Domperidone therapy was ineffectual. Four years prior to the diagnosis, the patient had intermittent occasional mild epigastric pain. She also reported occasional vomiting during the previous 15 years, which was not medically investigated.
On clinical examination, the patient appeared weak and dehydrated. Her abdomen was soft, without tenderness or palpable masses. Laboratory results revealed a hypokalemia of 1.9 mmol/L, which was substituted, and a metabolic alkalosis with an initial pH of 7.65. Serum amylase, bilirubin, and C-reactive protein (CRP) levels were not elevated.
Gastroscopy showed a reflux esophagitis, a massive distension of the stomach and the first part of the duodenum, respectively, and a stenosis of the second part of the duodenum, which could not be passed with the thin gastroscope.
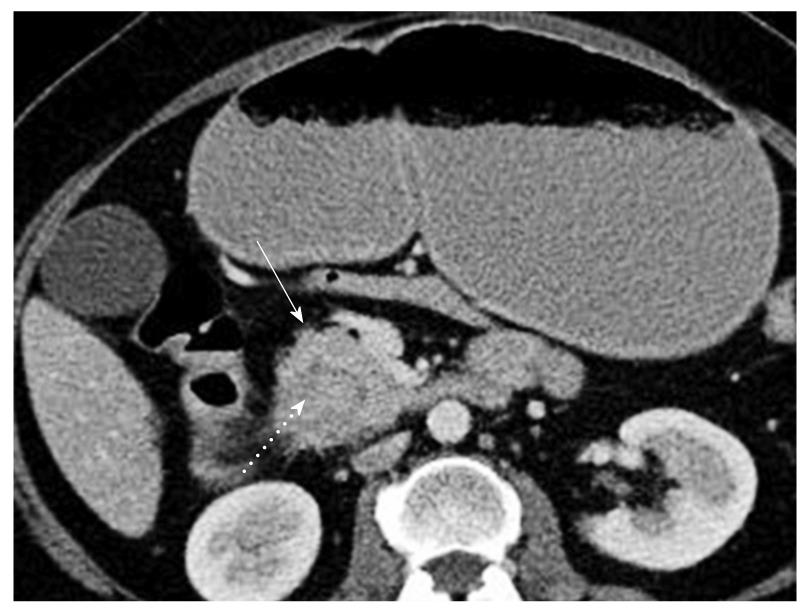
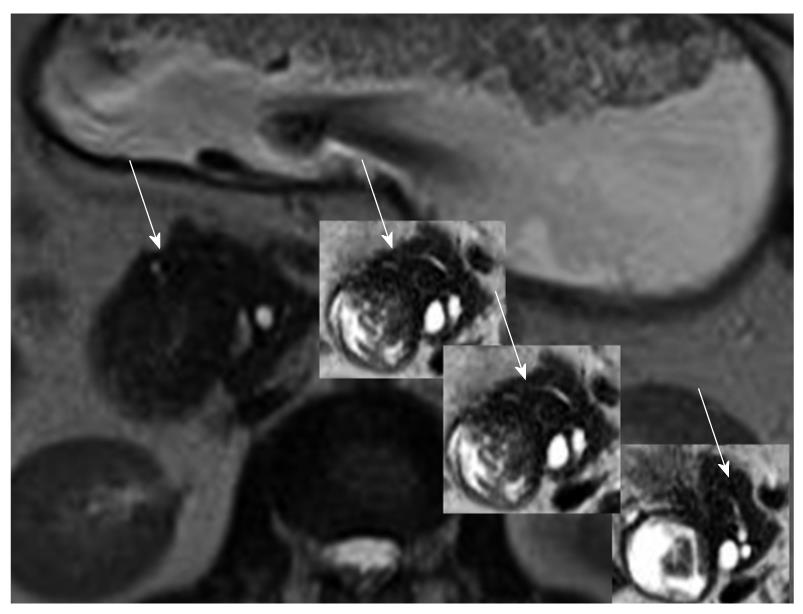
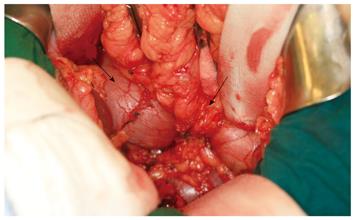
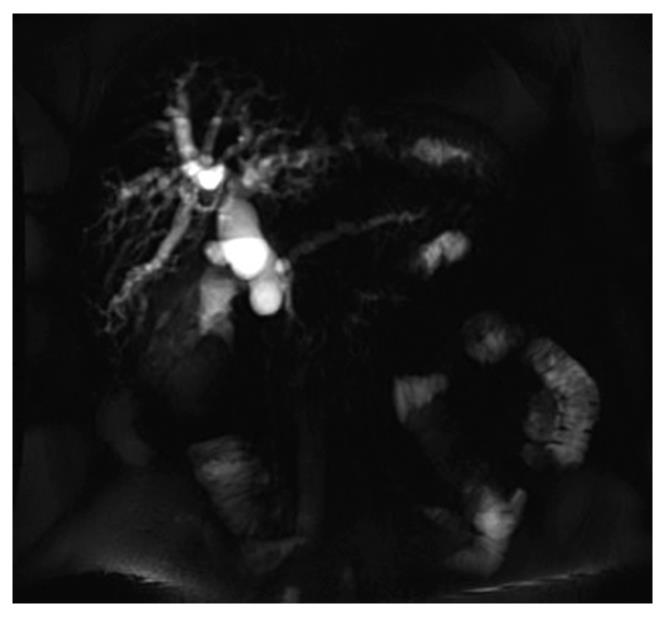
Abdominal MSCT depicted a fluid filled stomach and second segment of the duodenum (Figure 1). The pancreatic head was enlarged, surrounding the second segment of the duodenum; no dilation of the main pancreatic duct and common bile duct was noticed. For further evaluation, an MRCP was done. This showed an aberrant pancreatic duct encircling the duodenum, linked to the main pancreatic duct (Figure 2). No dilation of the common hepatic bile duct or the main pancreatic duct was evident. Due to the annular pancreas, there was an obstruction at the level of the second segment of the duodenum. During surgery, we found a massively distended and elongated first segment with a conic stenosis of the second segment of the duodenum due to the annular pancreas (Figure 3). A duodenojejunostomy was performed. There was no visible prestenotic tumor in the duodenum and the duodenal mucosa appeared to be normal. No tumor mass was palpated. The patient had an uneventful recovery and was discharged home with no complaints nine days later. After eight weeks, the patient was readmitted presenting with painless jaundice. She had no other complaints. No further weight loss was reported. Laboratory investigations showed elevated total bilirubin (112 μmol/L; reference range: 5-18) and alkaline phosphatases (178 U/L; reference range: < 104). An MRCP demonstrated dilatation of the common bile duct (Figure 4). On explorative laparotomy, a hard mass was palpated in the pancreatic head region. The frozen section of one of several suspicious superior pancreatic lymph nodes revealed adenocarcinoma cells. A duodenopancreatectomy was performed. The tumor was clearly located in the duodenum, with infiltration of the surrounding structures (Figure 5). No tumor was observed in the head of the pancreas. Pathological examination showed a poorly differentiated, infiltrating adenocarcinoma of the duodenum, surrounded by the incomplete annular pancreas (Figure 5). The tumor stage was pT4, pN1 (8/12), G3, L0, V0, R0. The tumor seemed to have arisen from the duodenal epithelium.
Figure 1 Multislice computed tomography.
A fluid filled stomach and enlargement of the pancreatic head (arrow) are detected, which encircles the second segment of the duodenum (dotted arrow).
Figure 2 T2 weighted magnetic resonance cholangiopancreatography images depict the aberrant pancreatic duct, which encircles the duodenum and connects with the main pancreatic duct (arrows).
Figure 3 During surgery, a massively distended and elongated first segment (left arrow) and a conic stenosis of the second segment of the duodenum were observed due to the annular pancreas (right arrow).
Figure 4 Eight weeks later, T1 w post contrast axial MR shows dilatation of the common bile duct.
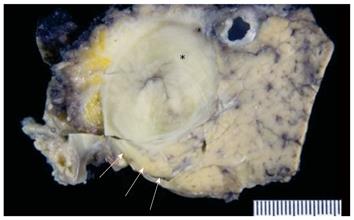
Figure 5 Cross sectional view showing the tumor within the duodenum (asterisk).
The duodenum is surrounded by the incomplete annular pancreas (arrows).
DISCUSSION
Symptoms
Clinical manifestation of annular pancreas can occur at any age, from neonatal period to adulthood. When the duodenal constriction is minimal or absent, annular pancreas can remain asymptomatic lifelong[24]. In infants, the common clinical symptoms are vomiting and feeding intolerance[7]. Clinical manifestation in adults can present with cramping epigastric pain, postprandial fullness, vomiting, and weight loss[10,25,26]. Association with pancreatitis, or a gastric/duodenal ulcer, can also occur[7,25]. The most frequent symptom in adult annular pancreas seems to be abdominal pain[7,10]. Most adults become symptomatic between the ages of 20 and 50[25]. The differential diagnosis includes other upper gastrointestinal pathologies, such as peptic ulcer disease, duodenal web, pancreatitis, or pancreatic carcinoma[19,27]. Obstructive jaundice is described as a rare direct result of annular pancreas, but appears in coexisting periampullary malignancies[19]. Of the above-mentioned 14 cases of carcinoma associated with annular pancreas, 10 presented obstructive jaundice. The most common symptoms of primary carcinoma of the duodenum are abdominal pain and weight loss[28]. Upon her first hospitalisation, our patient’s main symptoms were postprandial nausea and vomiting, associated with a significant weight loss. No abdominal pain was reported. Neither pancreatitis nor obstructive jaundice was apparent. Four years prior to diagnosis, the patient had been complaining intermittent occasional mild epigastric pain. In addition, over the previous 15 years, she had reported occasional vomiting. Fifteen years had passed from first symptoms until diagnosis of annular pancreas. Upon her second hospitalisation, her only symptom was jaundice.
Diagnosis/radiology
Annular pancreas is diagnosed by ERCP or by CT[29]. Since MRCP has become widely used, annular pancreas can be diagnosed non-invasively[30,31]. A recent study reviewed 55 cases with annular pancreas in adults[7]. Diagnosis was made with ERCP in 47%, MSCT in 18%, with MRCP in 16%, and in 13% of the patients, diagnosis was made at the time of surgery. We were able to make the diagnosis of annular pancreas non-invasively by abdominal MSCT (Sensation 16, Siemens Medical Solutions, Erlangen, Germany) and MRCP using a 1.5T scanner (1.5T Symphony, Siemens Medical Solutions, Erlangen, Germany). Due to the duodenal obstruction by the pancreatic ring, ERCP was not a feasible diagnostic alternative. Upon readmission, dilatation of the common bile duct was demonstrated by MRCP. Malignancy was found during explorative laparotomy. The final diagnosis was made by the pathologist. During her first hospitalisation, malignancy was not suspected either by preoperative diagnostics nor laparotomy. Upper gastrointestinal tract endoscopy is the most frequently performed test to diagnose duodenal adenocarcinoma[28]. In the present case, the tumor was hidden behind the annular pancreas and not within reach of the endoscope.
Therapy and prognosis
The treatment of annular pancreas is always surgical. The goal is to relieve the duodenal or gastric outlet obstruction. Dissection of the pancreatic ring should be avoided due to a high incidence of complications, including duodenal leak, pancreatic fistula, and postoperative pancreatitis[10]. Different surgical approaches have been described. Bypass surgery, such as duodenojejunostomy in pediatric surgery, and duodenoduodenostomy or gastrojejunostomy in adults is preferred. The safest and most successful way of bypassing the annular constriction seems to be duodenoduodenostomy or duodenojejunostomy[10]. The presence of a periampullary malignancy must be considered in adult patients with annular pancreas presenting with obstructive jaundice[19]. In cases of annular pancreas associated with proven or suspected periampullary malignancy, duodenopancreatectomy might be the treatment of choice[19]. This should also be performed when annular pancreas is associated with pancreatolithiasis and localized chronic pancreatitis[32]. Long-term survival of patients with duodenal adenocarcinoma can be achieved with a surgical procedure that produces negative resection margins, such as pancreaticoduodenectomy[28]. Adjuvant therapy seems not to improve the survival rate[33]. Initially, our patient did not show jaundice and imaging did not present a tumoral mass.
We decided to perform a duodenojejunostomy to bypass the stenosis. The postoperative course was uneventful. Five days after intervention, the patient was able to eat solid food.
After eight weeks, painless jaundice appeared and MR imaging revealed dilatation of the common bile duct but no tumoral mass. Intraoperatively, a hard mass was palpated in the pancreatic head region and adenocarcinoma cells were found in a pancreatic lymph node at frozen section. We performed a duodenopancreatectomy and the patient received no adjuvant therapy.
In conclusion, annular pancreas should be kept in mind when symptoms of upper gastrointestinal obstruction occur, but the presence of annular pancreas should not distract from a possible coexisting malignancy. As in the present case, such a malignancy can also be present without obstructive jaundice and without being visible through preoperative diagnostics. In such a case, pancreaticodudoenectomy might be the only way to exclude the coexistence of duodenal carcinoma with annular pancreas.