Published online Mar 28, 2010. doi: 10.3748/wjg.v16.i12.1545
Revised: November 27, 2009
Accepted: December 4, 2009
Published online: March 28, 2010
We report a unique case of intramucosal carcinoma in a tubulovillous adenoma arising from a single diverticulum. Endoscopic mucosal resection (EMR) was carried out successfully and completely with the assistance of laparoscopy. A 71-year-old man was admitted to our hospital because of melena and anemia. Emergent colonoscopy showed diverticulosis in the right-sided colon. However, endoscopy could not exactly detect the bleeding site. A flat elevated polyp was found within a single diverticulum located in the descending colon and diagnosed as an intramucosal carcinoma, as magnifying chromoendoscopy revealed a type IV pit pattern. As his diverticular bleeding repeated, a right-sided hemicolectomy was decided for treatment, the polyp within the diverticulum was also completely removed by EMR with the assistance of laparoscopy. Although a colonic perforation was detected immediately after EMR, the perforation was closed with endoclips intraluminally and also repaired laparoscopically from the serosal side. Histologically, the resected lesion was an intramucosal well-differentiated adenocarcinoma and the surgical margin was free of tumor.
- Citation: Fu KI, Hamahata Y, Tsujinaka Y. Early colon cancer within a diverticulum treated by magnifying chromoendoscopy and laparoscopy. World J Gastroenterol 2010; 16(12): 1545-1547
- URL: https://www.wjgnet.com/1007-9327/full/v16/i12/1545.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i12.1545
Colonic neoplasia can arise from the normal mucosa near or within a diverticulum. Adenoma or adenocarcinoma located within a diverticulum is, however, a very rare phenomenon and only sporadic cases have been reported to date[1-8]. The reported cases are often cases of advanced cancers and could only be diagnosed postoperatively. Therefore, the association of adenoma or early cancer with a diverticulum is exceptionally rare[3,4,6-8]. We herein describe a case of intramucosal carcinoma in a tubulovillous adenoma developed in a colonic diverticulum, which could be correctly diagnosed by magnifying chromoendoscopy and was subsequently treated by endoscopic mucosal resection (EMR) with the assistance of laparoscopy.
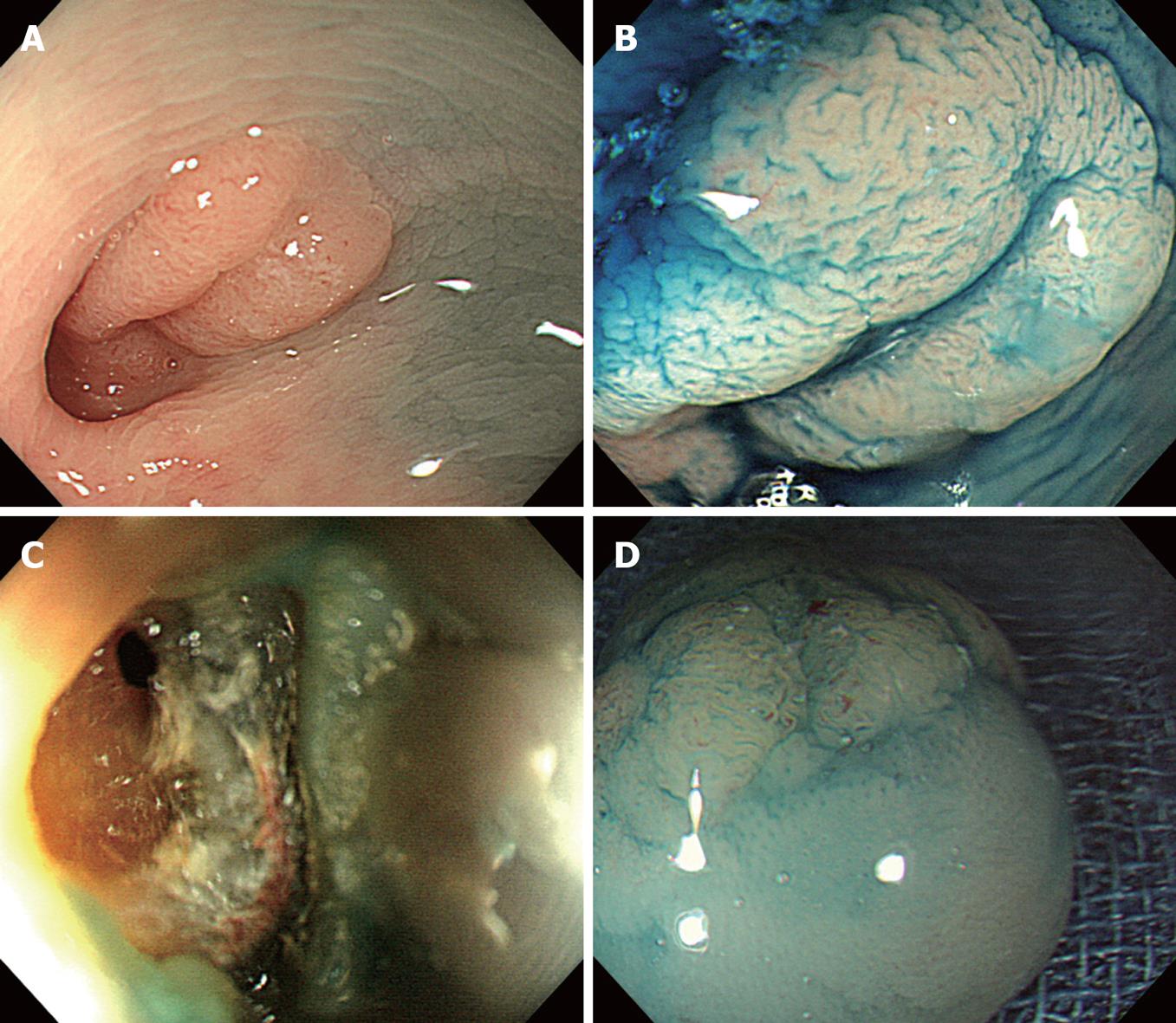
A 71-year-old man was admitted to our hospital because of melena and anemia. Emergent colonoscopy showed diverticulosis in the right-sided colon. However, endoscopy could not definitely detect the bleeding source. Additionally, colonoscopy showed a single diverticulum in the descending colon, and a flat elevated polyp, 15 mm in diameter, within the diverticulum (Figure 1A). Magnifying chromoendoscopy using 0.4% indigo-carmine dye spraying revealed a type IV pit pattern according to Kudo’s classification (non-invasive pattern according to Fujii’s classification)[9,10] (Figure 1B). Therefore, an endoscopic diagnosis of intramucosal carcinoma was established, and endoscopic resection was thus considered as the first line treatment. As his diverticular bleeding repeated, which could not be managed endoscopically, multiple blood transfusions were thus needed. Right hemicolectomy was decided for treatment. During laparoscopically assisted right hemicolectomy, EMR was also performed to remove the polyp within the diverticulum located in the descending colon. Glycerol was first injected into the submucosal layer to lift the polyp well (non-lifting sign negative), and subsequently EMR was successfully carried out. After EMR, a pin-hole perforation was detected endoscopically and laparoscopically (Figure 1C). Metal clips were used endoscopically to close the perforation which was also repaired laparoscopically. Magnifying chromoendoscopy of the removed lesion disclosed no neoplastic lesions at the surgical lateral margin (Figure 1D). The patient developed anal bleeding 6 d after surgery, and an urgent colonoscopy revealed bleeding at the anastomotic site of right hemicolectomy but not at the EMR site, and the bleeding was successfully stopped with metal clips. Histologically, the removed polyp was an intramucosal well-differentiated adenocarcinoma in a tubulovillous adenoma. No adenoma and adenocarcinoma were found at the lateral and vertical margin of the removed lesion. No muscle layer was identified in the removed lesions on histology.
Cancer arising from diverticula may be diagnosed at the advanced stage despite its small size. As colonic diverticula lack of muscular coats, and thus cancer can more easily extend into the serosal surface than that arising from the normal mucosa apart from the diverticulum[7]. We performed EMR to remove this lesion, as magnifying chromoendoscopy provided an endoscopic diagnosis of an intramucosal lesion. It is commonly accepted that colorectal cancers limited within the mucosal layer do not carry risks of lymph node metastasis and therefore are good candidates for endoscopic resection. Therefore, to avoid unnecessary surgery or endoscopic treatment, it is important to endoscopically evaluate the invasion depth of colorectal cancers before removal. The mucosal crypt patterns have been reported to be closely related to the histology and are helpful in endoscopic diagnosis by magnifying chromoendoscopy[9,10].
Histologically, diverticula have a characteristically thin wall without muscular layer. Surgical treatment is, therefore, recommended even for mucosal cancer or adenomatous polyp near or within a diverticulum, as colonic perforation may easily occur after endoscopic resection for such lesions. As anticipated, our case developed a colonic perforation immediately after EMR. Iatrogenic perforation is one of the most serious potential complications of colonoscopy[11]. Treatment strategies for colonic perforation include non-operative management with or without endoscopic closure, laparoscopic repair, and open surgery. EMR was performed for this case in our department with the assistance of laparoscopy to treat the diverticular bleeding in the right-sided colon[11,12]. Therefore, the perforation site of this case was first closed with endoclips intraluminally and thereafter repaired laparoscopically from the serosal side. In our opinion, this kind of pin-hole perforation can be managed only endoscopically with endoclips, and we would have tried EMR without laparoscopic assistance if there was no uncontrolled diverticular bleeding.
In conclusion, intramucosal cancer in a tubulovillous adenoma developed within a diverticulum can be correctly diagnosed by magnifying chromoendoscopy and successfully treated with minimally invasive surgery including EMR with the assistance of laparoscopy.
| 1. | Drut R. Adenoacanthoma arising in a diverticulum of the colon: report of a case. Dis Colon Rectum. 1974;17:258-261. |
| 2. | Hines JR, Gordon RT. Adenocarcinoma arising in a diverticular abscess of the colon: report of a case. Dis Colon Rectum. 1975;18:49-51. |
| 3. | McCraw RC, Wilson SM, Brown FM, Gardner WA. Adenocarcinoma arising in a sigmoid diverticulum: report of a case. Dis Colon Rectum. 1976;19:553-556. |
| 4. | Martich V, Kutashy M, Gasparaitis A. Polyp arising in a colonic diverticulum. AJR Am J Roentgenol. 1992;159:1348. |
| 5. | Cohn KH, Weimar JA, Fani K, DeSoto-LaPaix F. Adenocarcinoma arising within a colonic diverticulum: report of two cases and review of the literature. Surgery. 1993;113:223-226. |
| 6. | Kajiwara H, Umemura S, Mukai M, Sadahiro S, Tsutsumi Y. Adenocarcinoma arising within a colonic diverticulum. Pathol Int. 1996;46:538-539. |
| 7. | Kikuchi T, Kotanagi H, Kon H, Koyama K, Ito S, Otaka M. Mucosal carcinoma within a colonic diverticulum. J Gastroenterol. 1999;34:622-625. |
| 8. | Kobayashi N, Hirabayashi K, Matsui T, Hirahara Y, Kurihara H, Igarashi S, Ishikawa T, Sekiguchi R. Depressed-type colon cancer in a patient with diverticulosis. Endoscopy. 2008;40 Suppl 2:E44. |
| 9. | Kato S, Fujii T, Koba I, Sano Y, Fu KI, Parra-Blanco A, Tajiri H, Yoshida S, Rembacken B. Assessment of colorectal lesions using magnifying colonoscopy and mucosal dye spraying: can significant lesions be distinguished. Endoscopy. 2001;33:306-310. |
| 10. | Matsuda T, Fujii T, Saito Y, Nakajima T, Uraoka T, Kobayashi N, Ikehara H, Ikematsu H, Fu KI, Emura F. Efficacy of the invasive/non-invasive pattern by magnifying chromoendoscopy to estimate the depth of invasion of early colorectal neoplasms. Am J Gastroenterol. 2008;103:2700-2706. |
| 11. | Taku K, Sano Y, Fu KI, Saito Y, Matsuda T, Uraoka T, Yoshino T, Yamaguchi Y, Fujita M, Hattori S. Iatrogenic perforation associated with therapeutic colonoscopy: a multicenter study in Japan. J Gastroenterol Hepatol. 2007;22:1409-1414. |
| 12. | Hansen AJ, Tessier DJ, Anderson ML, Schlinkert RT. Laparoscopic repair of colonoscopic perforations: indications and guidelines. J Gastrointest Surg. 2007;11:655-659. |
Peer reviewer: Yutaka Saito, Professor, Division of Endoscopy, National Cancer Center Hospital, 5-1-1, Tsukiji, Chuo-ku, Tokyo 104-0045, Japan
S- Editor Wang YR L- Editor Wang XL E- Editor Lin YP