Published online Nov 7, 2009. doi: 10.3748/wjg.15.5236
Revised: September 7, 2009
Accepted: September 14, 2009
Published online: November 7, 2009
Giant esophageal inflammatory fibrous polyp (especially > 17 cm in size) is seen rarely. Endoscopic removal has been reported rarely because the procedure is technically demanding and the hemostasis is difficult to ascertain. Here, we describe a case of a giant upper esophageal inflammatory fibrous polyp that was resected successfully by endoscopy.
- Citation: Zhang J, Hao JY, Li SWH, Zhang ST. Successful endoscopic removal of a giant upper esophageal inflammatory fibrous polyp. World J Gastroenterol 2009; 15(41): 5236-5238
- URL: https://www.wjgnet.com/1007-9327/full/v15/i41/5236.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.5236
Giant esophageal inflammatory fibrous polyp (especially > 17 cm in size) is seen rarely[1]. Surgical excision is usually advised[2-5]. Endoscopic removal has been reported rarely[6] because the procedure is technically demanding and hemostasis is difficult to ascertain. Here, we described a giant upper esophageal inflammatory fibrous polyp that was resected successfully by endoscopy.
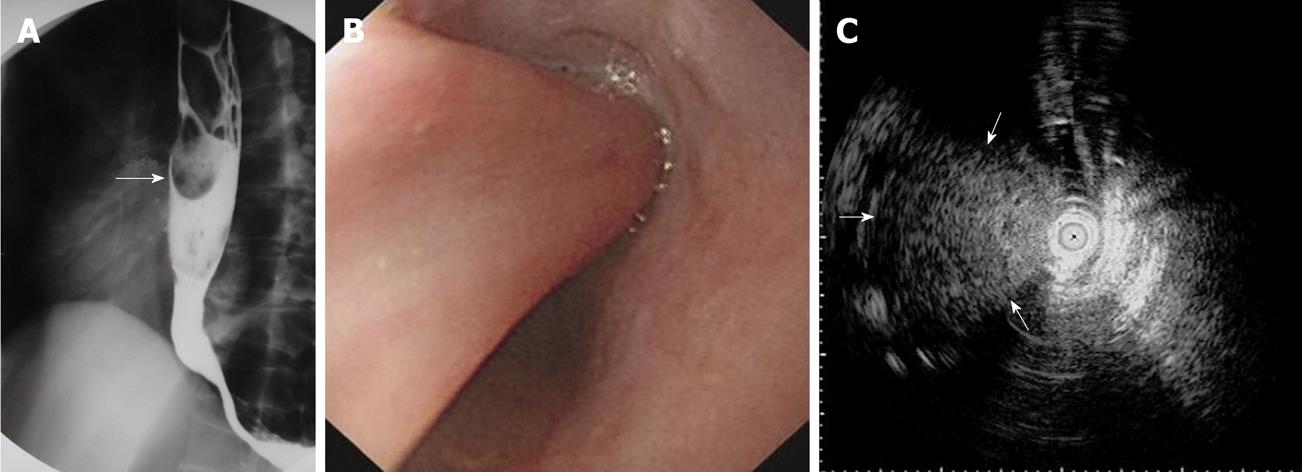
A 50-year-old man presented to our hospital with a 6-mo history of progressive difficulty in swallowing, initially, solid and then liquid food for the past 2 mo. Physical examination and blood tests, including coagulation parameters, were normal. Barium swallow revealed a 17-cm polypoid filling defect inside the esophagus that moved with deglutition (Figure 1). Contrast thoracic computed tomography (CT) revealed a localized isodense upper esophageal lesion, which was free from the lower part of the esophagus. The esophageal wall was intact and there was no evidence of infiltration into adjacent organs or any mediastinal lymphadenopathy. Gastroscopy showed a giant polyp with smooth overlying mucosa, extending from 18 to 35 cm (measured from the incisors), and endoscopic ultrasonography (EUS) revealed well-distributed, low-echo-level lesions at the root of the polyp, excluding echoless lumen-like structures (no large blood vessels inside the lesions) (Figure 1). Therefore, the esophageal polyp was a benign lesion. Endoscopic removal of the polyp with an electrosurgical snare was attempted, using the ICC 200 (ERBE, Tubingen, Germany). The procedure was performed under general anesthesia with elective intubation and airway protection. Equipment for hemostasis, including hemoclips, Coagrasper, injection needle and adrenaline for injection was prepared before the procedure.
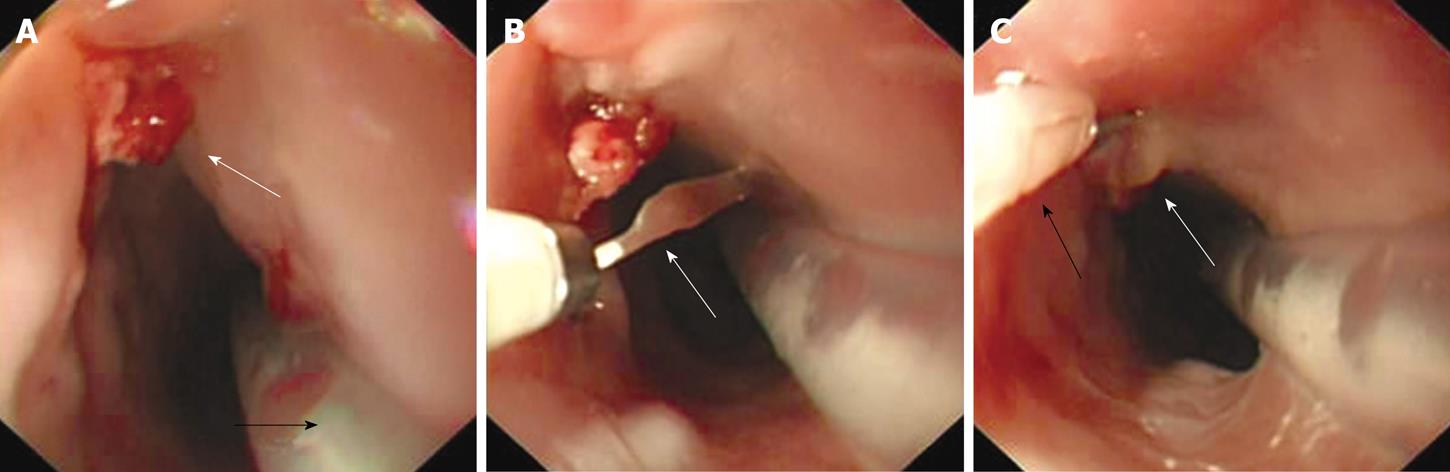
Firstly, we inserted a detachable loop of appropriate stiffness and size through the biopsy channel. Then, the detachable loop was placed from the base to the neck of the esophageal polyp. The loop was closed gradually and the polyp was lifted away from the esophageal wall. Polypectomy was performed and air was inflated to distend the esophagus. The setting of the electrosurgical units was as follows: COAG mode (effect 350 W) was first applied for 2 s, so that the small blood vessels over the mucosa were coagulated. Then, we employed the endo-cut mode (effect 380 W) to CUT. Near the end of polypectomy, COAG mode was resumed to minimize bleeding from the central blood vessel. Adequate air insufflation and distension of the esophagus minimized the risk of burning and esophageal perforation. Only minor bleeding was noted at the polypectomy site. The hemostasis was achieved securely with 1:10 000 adrenaline injection and application of two hemoclips over the polypectomy site (Figure 2).
In addition, a 16-Fr nasogastric tube was placed to remove all the blood and gastric fluid during the procedure (Figure 2). If the esophageal polyp failed to be removed or there was any complication, an on-site thoracic surgeon assessed the patient urgently for operation.
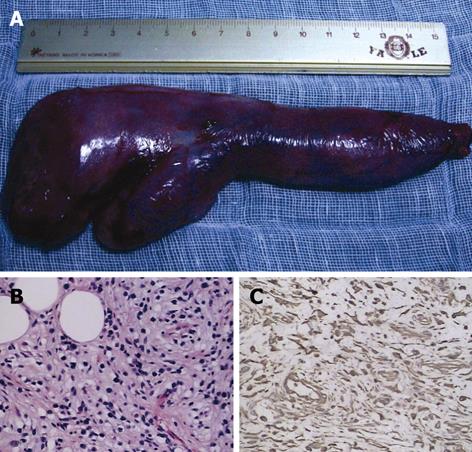
The resected esophageal polyp specimen (Figure 3) was retrieved with the snare and sent to the pathology laboratory for pathological examination. Hematoxylin and eosin (HE) staining of the removed esophageal specimen showed the presence of lots of fibroblasts, with some adipocytes, plasma cells and acidophilic cells (Figure 3). Immunostaining revealed CD 117 (-), CD 34 (-), S-100 (-), desmin (-), actin (-), cytokeratin (-), HMB45 (-) and vimentin (+) (Figure 3). The histological diagnosis was inflammatory fibrous polyp. The patient remained well and was discharged 1 wk after the procedure. Follow-up gastroscopy 4 wk later was normal.
Inflammatory fibrous polyp, also known as inflammatory pseudotumor, is a benign intraluminal tumor that consists of a mixture of inflamed fibrous, granulation tissue and lipomatous elements, which is covered by normal squamous epithelium[7]. Giant esophageal inflammatory fibrous polyp (especially > 17 cm in size) is seen rarely[1,8]. The presenting symptoms of dysphagia and sensation of a mass in esophageal inflammatory fibrous polyp are the same as in other esophageal tumors (such as leiomyoma and gastrointestinal stromal tumor), unless there is development of regurgitation of the polyp through the mouth or asphyxiation[9]. Some cases may stay asymptomatic or with heartburn for a long time[10,11]. Inflammatory fibroid polyps should be considered in the differential diagnosis of submucosal and polypoid esophageal masses, although distinctive radiographic features are not found[12]. Usually, the diagnosis is made by imaging or endoscopic studies. Barium-enhanced contrast of the esophagus usually shows a sausage-shaped mass with multiple filling defects, which originates in the cervical esophagus and extends to the lower esophagus[10]. Endoscopy usually shows an intraluminal mass that is mobile and covered with normal mucosa. Careful examination of the upper esophageal sphincter may reveal the stalk of the pedunculated mass. It is not difficult to distinguish esophageal inflammatory fibrous polyp from leiomyoma, which is usually relatively flat, and non-pedunculated intramural lesions in the middle and lower third of the esophagus[13]. EUS has been reported as a method to demonstrate the submucosal origin of analogical polyps[14,15].
As a result of its special origin, there may be uncontrollable bleeding during endoscopic resection. Endoscopic removal of giant upper esophageal lesions requires thorough assessment before the procedure. Therefore, multiple modalities (barium, CT, EUS and gastroscopy) are important to delineate the nature and origin of the lesion. EUS provides information on the diameter of the polyp as well as its vascularity and insertion point[6]. Special precautions during hemostasis and elective airway protection are necessary to prevent bleeding and aspiration. The placement of the nasogastric tube, adequate insufflation and distension of the esophagus can minimize the risk of burning and esophageal perforation. The site of snare polypectomy should be kept away from the base of stalk to prevent esophageal perforation. Advances in the techniques of endoscopic treatment and the improvement of endoscopic accessories make endoscopic removal of giant esophageal polyps feasible. Post-polypectomy hemostasis can be achieved with adrenaline injection and hemoclips. If hemostasis fails, one can use Coagrasper to coagulate even a small area of bleeding.
In conclusion, with thorough assessment with multiple imaging modalities, and the availability of good endoscopic accessories, giant upper esophageal inflammatory fibrous polyp can be resected by endoscopy safely and successfully.
| 1. | Solito B, Anselmino M, Tognetti A, Vignati S, Rossi M. Rare case of inflammatory fibrous polyp of the esophagus. Dis Esophagus. 2002;15:326-329. |
| 2. | Ozcelik C, Onat S, Dursun M, Arslan A. Fibrovascular polyp of the esophagus: diagnostic dilemma. Interact Cardiovasc Thorac Surg. 2004;3:260-262. |
| 3. | Bosch O, González Campos C, Jurado A, Guijo I, Miro C, Renedo G, Porres JC. Esophageal inflammatory fibroid polyp. Endoscopic and radiologic features. Dig Dis Sci. 1994;39:2561-2566. |
| 4. | Iván L, Paczona R, Szentpáli K, Jóri J. Peroral endoscopic removal: as a minimally invasive long-term surgical treatment of a regurgitated giant polisegmented fibrovascular polyp of the esophagus. Eur Arch Otorhinolaryngol. 2009;266:1031-1034. |
| 5. | Kanaan S, DeMeester TR. Fibrovascular polyp of the esophagus requiring esophagectomy. Dis Esophagus. 2007;20:453-454. |
| 6. | McLean JN, DelGaudio JM. Endoscopic resection of a giant esophageal polyp: case report and review of the literature. Am J Otolaryngol. 2007;28:115-117. |
| 7. | LiVolsi VA, Perzin KH. Inflammatory pseudotumors (inflammatory fibrous polyps) of the esophagus. A clinicopathologic study. Am J Dig Dis. 1975;20:475-481. |
| 8. | Minutolo V, Rinzivillo C, Li Destri G, Scilletta B, Cammisuli F, Puleo S. Giant esophageal polyp: a rare and benign neoplasm. Chir Ital. 1999;51:313-316. |
| 9. | Pham AM, Rees CJ, Belafsky PC. Endoscopic removal of a giant fibrovascular polyp of the esophagus. Ann Otol Rhinol Laryngol. 2008;117:587-590. |
| 10. | Ginai AZ, Halfhide BC, Dees J, Zondervan PE, Klooswijk AI, Knegt PP. Giant esophageal polyp: a clinical and radiological entity with variable histology. Eur Radiol. 1998;8:264-269. |
| 11. | Yamane T, Uchiyama K, Ishii T, Ishii H, Takizawa R, Omura M, Fujise K, Tajiri H. Case of inflammatory fibroid polyp of the esophagogastric junction. Dig Endosc. 2009;21:97-100. |
| 12. | Simmons MZ, Cho KC, Houghton JM, Levine CD, Javors BR. Inflammatory fibroid polyp of the esophagus in an HIV-infected individual: case study. Dysphagia. 1995;10:59-61. |
| 13. | Levine MS. Benign tumors of the esophagus: radiologic evaluation. Semin Thorac Cardiovasc Surg. 2003;15:9-19. |
| 14. | Lawrence SP, Larsen BR, Stacy CC, McNally PR. Echoendosonographic and histologic correlation of a fibrovascular polyp of the esophagus. Gastrointest Endosc. 1994;40:81-84. |
| 15. | Costa PM, Marques A, Távora , Oliveira E, Diaz M. Inflammatory fibroid polyp of the esophagus. Dis Esophagus. 2000;13:75-79. |
Peer reviewer: Nageshwar D Reddy, Professor, Asian Institute of Gastroenterology, 6-3-661, Somajiguda, Hyderabad - 500 082, India
S- Editor Li LF L- Editor Kerr C E- Editor Zheng XM