INTRODUCTION
Mean transit time (MTT) and permeability surface area product (PS) of contrast material are two important parameters of perfusion computed tomography (CT). MTT is defined as the time that a contrast agent takes to go through the liver, from entry to exit and averaged over all possible paths. The PS is considered as the speed of transfer of a contrast agent from the capillary endothelium to the intercellular space (one-way). These parameters are, to a certain extent, two descriptors of parenchymal microvascular changes.
In chronic liver diseases, a capillarization of the sinusoids is observed, which is characterized by endothelial defenestration, collagen deposition in the extravascular Disse’s space, formation of basal laminae[1–3], and increased intrahepatic vascular resistance[45]. All these microvascular changes in cirrhosis have great influence on the development of the hepatic function[6–8]. In order to evaluate the quantitative and qualitative microvascular alterations in liver cirrhosis, these hepatic perfusion parameters (both MTT and PS) were measured in patients with liver cirrhosis by perfusion CT and the results compared to those of healthy volunteers.
MATERIALS AND METHODS
Patients
Sixty-eight adult patients were studied, including 29 controls and 39 patients with cirrhosis (22 with compensated cirrhosis and 17 with decompensated cirrhosis, divided by two experienced physicians specialized in hepatology). Four additional patients with cirrhosis were excluded because of surgically confirmed hepatocellular carcinoma. Three cirrhotic patients were excluded due to a disagreement on the assignment to the compensated or decompensated cirrhosis group. The 29 controls without liver disease (8 women, 21 men; age range: 28-78 years; average age: 49.5 years) performed perfusion CT examination of the abdomen for unrelated causes. In these 29 controls, lack of liver disease was documented by history, physical examination, laboratory screening, and Doppler sonography of the liver. Twenty-two patients (4 women, 18 men; age range: 31-78 years; average age: 58.6 years) had compensated cirrhosis. Among them, one had alcoholic cirrhosis, two had primary biliary cirrhosis, three had cryptogenic cirrhosis and 16 had posthepatitic cirrhosis. Seventeen patients (5 women, 12 men; age range: 31-78 years; average age: 55.9 years) had decompensated cirrhosis. The origin of cirrhosis in these cases was alcohol in one, hepatitis C virus in one, cryptogenic in one, primary biliary cirrhosis in one, and hepatitis B in the remaining 13 patients. All diagnoses were confirmed by appropriate clinical and laboratory examinations, No patient had portal thrombosis at ultrasonography. The study was approved by the ethics committee at our institution and was in conformity with the ethical guidelines of the 1975 Declaration of Helsinki[9]. The patients gave informed consent to participate in the study.
Imaging
After an overnight fast, multiple-slices dynamic sequences were carried out. A fixed 5 mm thick slice, which was selected to include the right hepatic lobe, spleen and portal trunk, was repeatedly scanned with cine mode. Scanning was carried out using a low radiation dose (120 kV, 60 mA), cine-scan mode, standard reconstruction algorithm, 35 cm display field of view (LightSpeed RT, GE Medical Systems, Milwaukee, WI) with a 50 s of continuous scanning time set at 8 s after the injection of contrast material. A bolus infusion of 50 mL of contrast material [Omnipaque (iohexol); 350 mg I/mL; Beijing, China] was given at 5.5 mL/s via a 20 gauge intravenous catheter in the antecubital vein. Patients were advised to hold their breath as long as possible, and oxygen inhalation at 2 L/min was provided to facilitate long breathholding during scanning.
Data analysis
These images were transferred to a workstation (GE Advantage workstation 4.2) for data analysis by using Perfusion 3 software. Three regions of interest (ROI) were set on the abdominal aorta, the portal vein trunk, and the right liver lobe respectively, by two radiologists with 10 years of experience in gastrointestinal and hepatobiliary imaging. The former two ROIs were set as input function. The latter ROI of the right liver lobe was drawn on the whole visible right lobe carefully, avoiding blood vessels and margin of liver parenchyma. The value of the latter ROI was measured and averaged for the hepatic perfusion parameters.
Statistical analysis
The results of the two perfusion parameters (MTT, PS) were expressed as the mean ± SD. All data were analyzed by SPSS 11.5 software. The independent samples t test was used to determine differences between cirrhotics and controls. Data of the three groups (normal control subjects, patients with compensated cirrhosis, and patients with decompensated cirrhosis) were compared using one-way analysis of variance. Bonferroni’s correction was applied. Statistical significance was defined as a P < 0.05.
DISCUSSION
A simple, noninvasive technique to separately quantify the changes of arterial and portal venous components in cirrhosis has always been a long-standing ambition of both pathologists and physicians. Most authors have reached an agreement on the notion that the increase of intrahepatic vascular resistance leads to a decrease of the portal fraction of liver perfusion[45]. This decreased portal perfusion is partially compensated by an increase of arterial flow, with the total liver perfusion being reduced in cirrhotic patients[41011]. More importantly, since the changes of the hepatic microcirculation in cirrhosis influence the progression of the disease, such a technique would be of greater value in hepatology. Various methods exist for the determination of hepatic microcirculation in clinical practice[12–15]. Most of them, however, are invasive or of controversial significance[1216]. It’s possible to measure both arterial and portal venous flow at the level of the main vessels using Doppler sonography, but this gives an indirect measurement of the circulation at parenchymal level. It is much harder to assess alterations in capillary blood, i.e. at the level of the microcirculation. Nuclear medicine techniques have been hindered by limited spatial and temporal resolution, and used only to estimate the arterial relative to the portal venous blood flow[17–19], since they can hardly differentiate the overlapping fractions of hepatic artery and portal vein perfusion within the liver tissue.
Reports have shown that the hepatic microcirculation can be estimated by the hepatic clearance of sorbitol[813] due to its high extraction fraction in normal subjects. The clearance of sorbitol is flow-limited and reflects hepatic microcirculation through functional sinusoids. However, sorbitol has been used as a marker of functional perfusion, which raises the issue of the decrease of the hepatocyte extraction of sorbitol in cirrhosis[20]. Moreover, the sorbitol clearance method cannot separate the measurements of arterial and portal flows. In addition, it needs to collect urine to determine the renal clearance of sorbitol after several hours, which may cause logistic problems in a busy clinical department[20].
CT is suited for the measurement of perfusion. Because of the high spatial and temporal resolution, modern CT scanners have been used widely in clinical studies, diagnosis and treatment. The methods for quantifying tissue perfusion by dynamic CT were described previously[1421]. Many studies have been conducted using this similar method with the use of iodinated contrast agents[52223]. This technique measures the slope of the time-attenuation curve, and only the peak time-points of the aortic and portal time-attenuation curves have been applied. The procedure can quantify the arterial and portal venous blood flow at tissue level, but the use of single-slice CT hampers its limited temporal resolution and Z-axis spatial resolution[222425]. Some respiratory motion artifacts are unavoidable, and they considerably influence the quantification. We used here a 16 slices spiral-CT with super high Z-axis spatial resolution and temporal resolution, which avoided the motion artifacts in an efficient way. The perfusion parameters were measured by the deconvolution method, which uses a well-established compartmental modeling technique[26]. Several points of the time-attenuation curves were used. Arterial and portal venous perfusion was detected quantitatively. In particular, the MTT and the PS could be quantified. These parameters were important and critical to assess the function of liver, as shown by many studies in humans and animals.
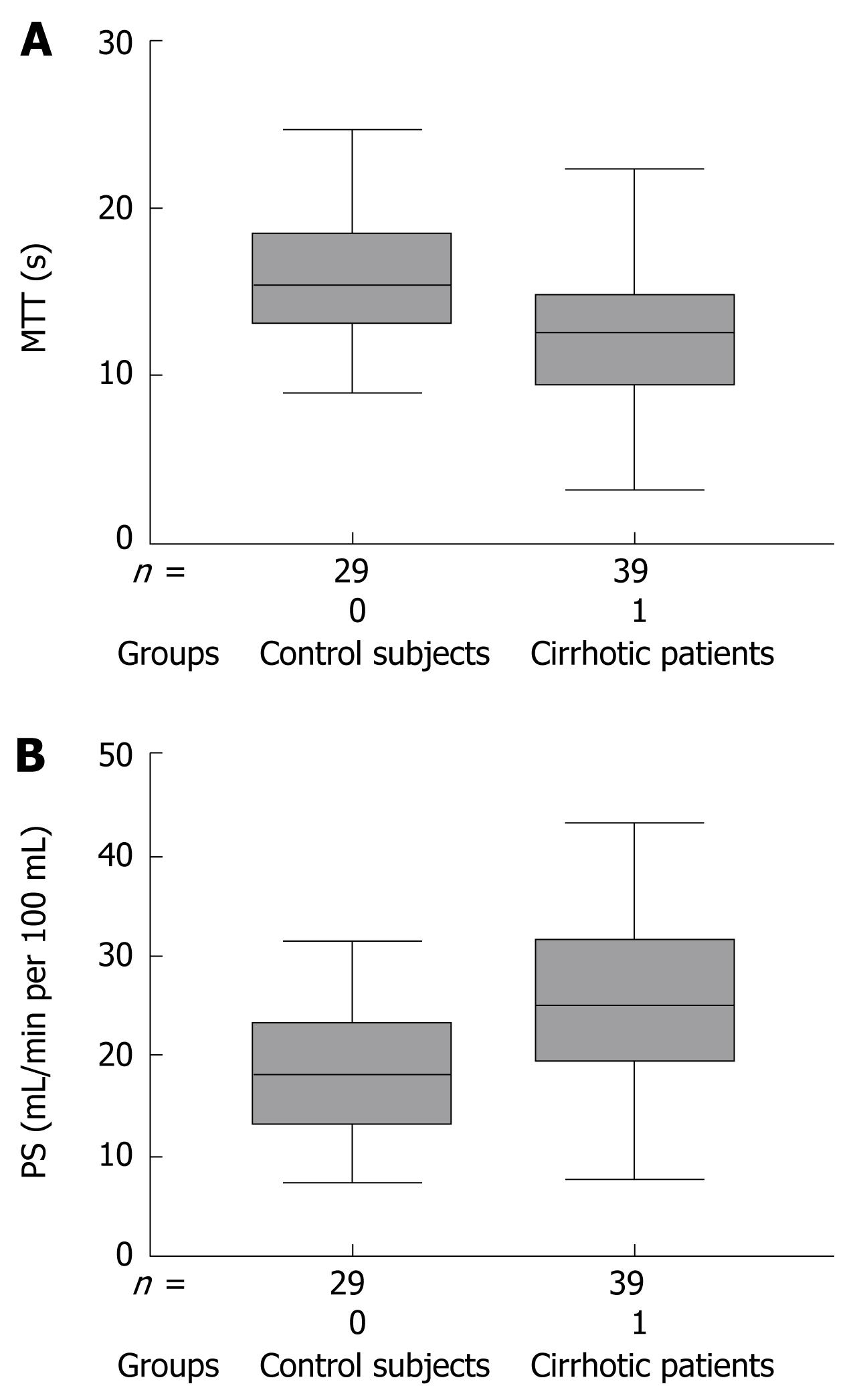
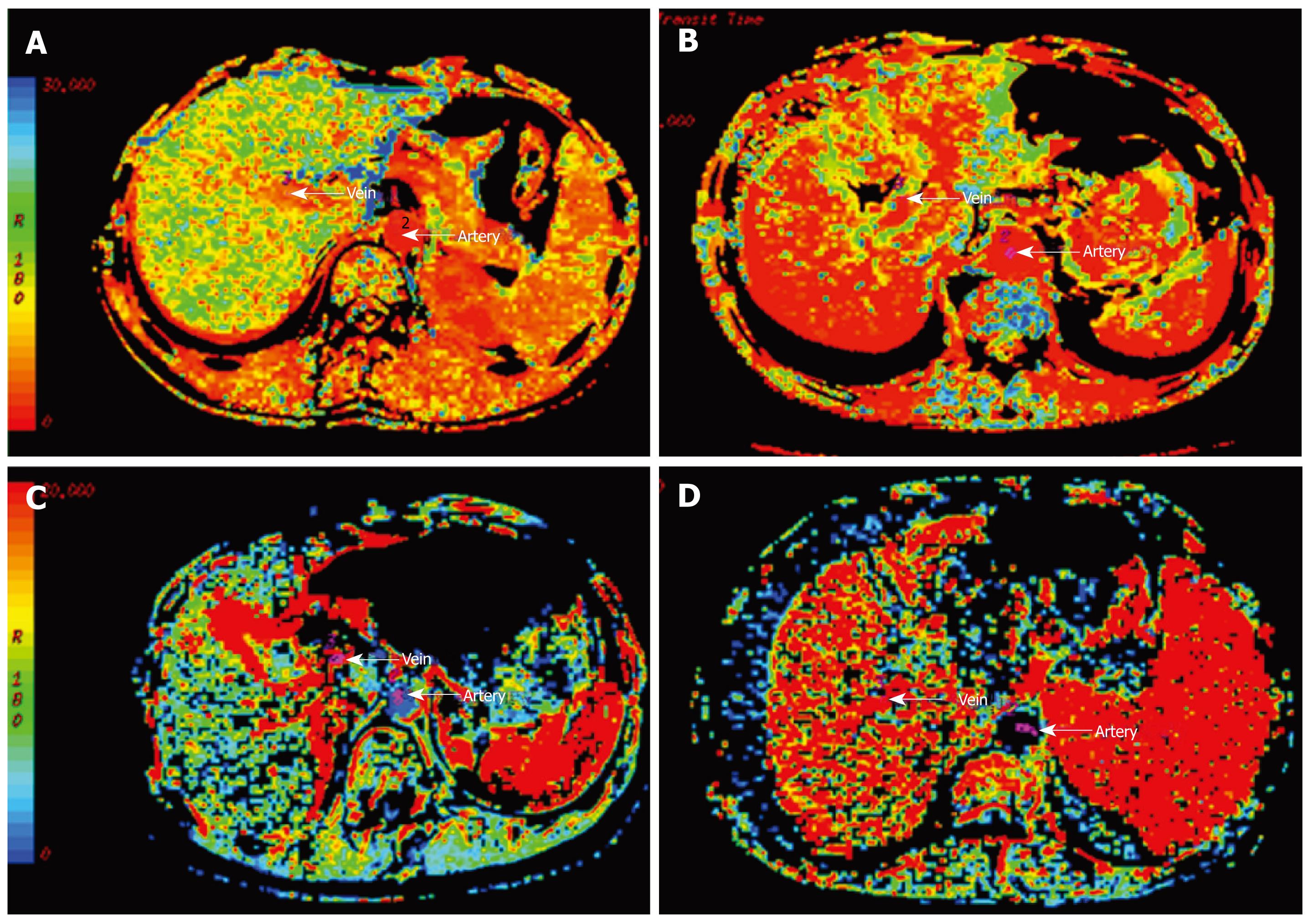
The MTT mainly reflects the blood capillary’s time. Some early studies almost exclusively depended on ex vivo evaluations using the same multiple indicator dilution technique described previously[813]. A study[25] on MTT had already relied upon CT, and its results were in agreement with the findings of the indicator dilution techniques. These investigators observed that the small-molecular-weight contrast agent used in their study had an increased transit time in cirrhotic patients. Some other studies[2728] reported no difference in MTT between controls and cirrhotic patients. In the present study, however, the MTT values observed in control subjects (Figure 3A) were higher than in cirrhotic patients (Figure 3B). The MTT of contrast agent measured in the cirrhotic livers was significantly shorter than among controls (P = 0.002) (Figure 1A). He et al[29] had already reported similar results, but the difference was not statistically significant. We hypothesize that there may be some differences as to etiopathogenesis, disease severity and gender distribution among the cirrhotic patients in previous studies[53031]. The patients enrolled in our study (women/men: 9/30) had a cirrhosis mostly due to hepatitis B virus (29/39) and only few had alcoholic cirrhosis (2/39), whereas no patients with hepatitis B virus infection and nine alcoholics of 18 cirrhotic patients (women/men: 6/12) were included in a previous study[25]. Histopathological examinations have shown that in the cirrhotic liver several sinusoids become capillarized and many terminal hepatic venules are distended[3233]: the combination of these changes may lead to low-resistivity, high-speed vascular flow, with increased inflow and outflow. In addition, intrahepatic portal veins and hepatic veins cross cirrhotic areas, leading directly or indirectly into the central venous compartment. All of the above causes may have brought about the shorter MTT in cirrhotic patients.
Figure 3 MTT and PS maps between controls and cirrhotic patients.
MTT in a control subject (A) was higher than in a cirrhotic patient (B). PS in a control subject (C) was lower than in a cirrhotic patient (D).
The PS shows the permeability of blood capillaries. As shown in this study, PS may be quantified noninvasively using perfusion CT scans acquired from control subjects and patients with cirrhosis. We observed that the PS of controls (Figure 3C) was lower than in cirrhotic patients (Figure 3D): PS was in fact significantly increased in cirrhosis (P = 0.003), (Figure 1B). This change may be explained by the results obtained with multiple indicator dilution techniques in human cirrhosis or rat cirrhotic liver. The increased microvascular resistance in the cirrhotic liver reduces capillary blood flow; the reduction in capillary blood flow is compensated by liver arterialization, increasing the capillary perfusion[41011].
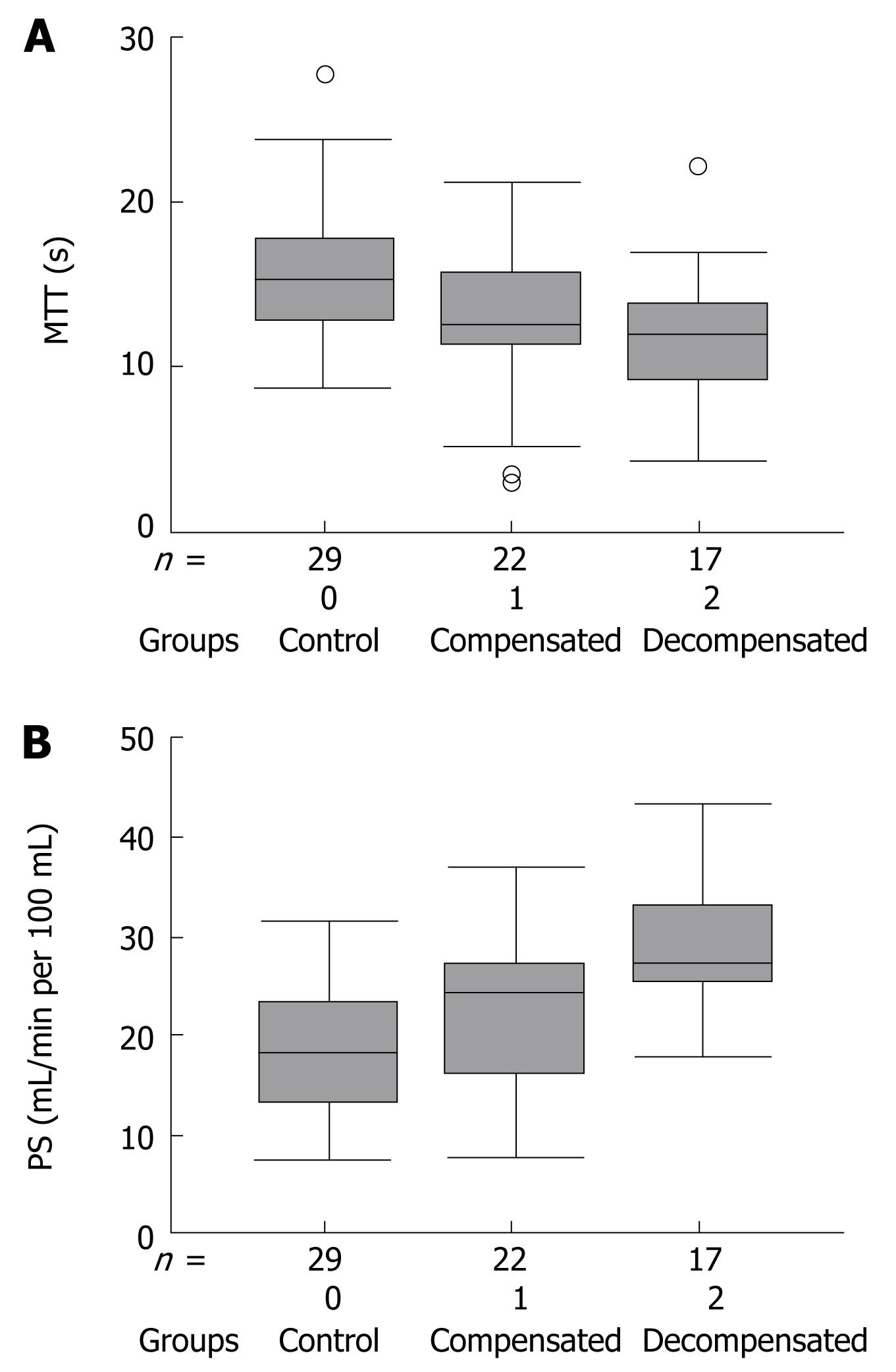
In addition, we observed that MTT and PS measured by the perfusion CT tended to change significantly in patients with decompensated cirrhosis (Table 2). Compared to controls, the MTT of patients with compensated cirrhosis was decreased, while the PS was increased: however, these differences failed to reach a statistically significant level in our study. We cannot exclude that some microvascular changes might indeed occur also in cases with compensated cirrhosis (Figure 2),
and that the differences between compensated cirrhotic patients and the other groups may become significant simply by increasing the size of the study population. In contrast, the microvascular perfusion parameters (both MTT and PS) were significantly altered in decompensated cirrhosis.
However, because it was difficult to control all the aspects of the study, there are several limitations associated with this study. First, the radiation dose may be one of the most important issues when using the perfusion CT, especially with cine-scan mode. Secondly, during CT imaging, patients are requested to hold their breath for long periods of time. Besides, a further limitation of our study is the small overall sample size. Perhaps, the differences between compensated cirrhosis group and the other groups would turn significant if the overall sample size increased.
Despite these limitations, our study with perfusion CT has proven that the perfusion parameters (MTT and PS) are significantly changed in patients with cirrhosis. The decreased MTT and increased PS of an iodinated contrast agent correlate with the severity of liver cirrhosis. They may be two acceptable indicators of the degree of hepatic microcirculation alteration in patients with cirrhosis. In addition, the quantification by perfusion CT may also improve our understanding of the effects on the hepatic microcirculation of vasoactive drugs and interventional procedures for the treatment of cirrhosis[34–36].
These findings underscore the possibility of using perfusion CT as a marker of hepatic microcirculation. Perfusion CT may be used as a noninvasive tool to quantify hepatic microvascular parameters in cirrhotic liver.
COMMENTS
Background
Hepatic microcirculation is of great importance in hepatology. Its changes in cirrhosis may heavily influence the progression of the disease. Various methods exist for the determination of hepatic microcirculation in clinical practice. However, most of them are invasive or controversial.
Research frontiers
Mean transit time (MTT) and permeability surface (PS) area product of contrast material for quantifying hepatic vascular changes by dynamic computed tomography (CT) were rarely measured in previous studies. The research hotspot is whether hepatic microvascular changes can be quantified by perfusion CT and what kind of modifications can be measured.
Innovations and breakthroughs
Previous applications of perfusion CT to the cirrhotic liver focused on hepatic haemodynamics. Most studies have reached an agreement on the fact that the increase of intrahepatic vascular resistance leads to a decrease of the portal fraction of liver perfusion. This decreased portal perfusion is partially compensated by an increase of arterial inflow, while the total liver perfusion is reduced in cirrhotic patients. However, hepatic microvascular changes were ignored. Few studies on MTT and PS have already relied upon CT. In order to explore hepatic microvascular parameters in patients with liver cirrhosis by using the perfusion CT, the authors compared hepatic microvascular parameters in patients with cirrhosis with those found in healthy volunteers. MTT and PS were significantly altered in liver cirrhosis. In order to obtain some meaningful correlations of the MTT and PS values with the severity of cirrhosis, they measured these parameters in three groups: control subjects, and patients with compensated or decompensated cirrhosis. They found that these parameters were significantly altered in patients with decompensated cirrhosis.
Applications
Hepatic microvascular parameters may be used to quantitatively assess hepatic microcirculation: the findings correlate with the severity of liver cirrhosis. These data may improve our understanding of the hepatic microcirculation effects of vasoactive drugs and interventional procedures for the treatment of cirrhosis.
Terminology
MTT: Mean transit time, a parameter defined as the time that a contrast agent takes to cross the liver, from entry to exit, averaged across all possible paths. PS: Permeability surface area product, which is considered as the speed of a contrast agent from the capillary endothelium to the intercellular space (one-way).
Peer review
The authors examined the differences in MTT and PS between normal individuals and patients with cirrhosis; they propose that perfusion CT may be utilized to quantify changes in microcirculation among stages of cirrhosis. Overall, an interesting study.