Published online Jun 21, 2009. doi: 10.3748/wjg.15.2900
Revised: April 14, 2009
Accepted: April 21, 2009
Published online: June 21, 2009
AIM: To evaluate the maximal-outer-diameter (MOD) and the maximal-mural-thickness (MMT) of the appendix in children with acute appendicitis and to determine their optimal cut-off values to diagnose acute appendicitis.
METHODS: In total, 164 appendixes from 160 children between 1 and 17 years old (84 males, 76 females; mean age, 7.38 years) were examined by high-resolution abdominal ultrasound for acute abdominal pain and the suspicion of acute appendicitis. We measured the MOD and the MMT at the thickest point of the appendix. Patients were categorized into two groups according to their medical records: patients who had surgery (surgical appendix group) and patients who did not have surgery (non-surgical appendix group). Data were analyzed by MedCalc v.9.3. The rank sum test (Mann-Whitney test) was used to evaluate the difference in the MOD and the MMT between the two groups. ROC curve analysis was used to determine the optimal cut-off value of the MOD and the MMT on diagnosis of acute appendicitis.
RESULTS: There were 121 appendixes (73.8%) in the non-surgical appendix group and 43 appendixes (26.2%) in the surgical appendix group. The median MOD differed significantly between the two groups (0.37 cm vs 0.76 cm, P < 0.0001), and the median MMT also differed (0.15 cm vs 0.33 cm, P < 0.0001). The optimal cut-off value of the MOD and the MMT for diagnosis of acute appendicitis in children was > 0.57 cm (sensitivity 95.4%, specificity 93.4%) and > 0.22 cm (sensitivity 90.7%, specificity 79.3%), respectively.
CONCLUSION: The MOD and the MMT are reliable criteria to diagnose acute appendicitis in children. An MOD > 0.57 cm and an MMT > 0.22 cm are the optimal criteria.
- Citation: Je BK, Kim SB, Lee SH, Lee KY, Cha SH. Diagnostic value of maximal-outer-diameter and maximal-mural-thickness in use of ultrasound for acute appendicitis in children. World J Gastroenterol 2009; 15(23): 2900-2903
- URL: https://www.wjgnet.com/1007-9327/full/v15/i23/2900.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.2900
Since Puylaert[1] described the role of ultrasound (US) as a diagnostic method for acute appendicitis in 1986, the diagnosis of acute appendicitis has become more dependent on the use of US, especially in the doubtful cases for the clinicians. Because of the smaller trunks and thinner subcutaneous fat layer in children compared to adults, US evaluation of the appendix is easier in children. According to previous reports[1–4], radiologists have used several US findings to diagnose acute appendicitis. Among these findings, the maximal outer diameter (MOD) of the appendix was regarded as the most reliable measurement. When the MOD is > 0.6 cm, radiologists suggest the presence of acute appendicitis is indicated.
However, the MOD may be larger than 0.6 cm without acute inflammation. The concern is that the MOD may be exaggerated by the presence of intra-luminal materials such as gas, feces and fluid[5–7]. To decrease the false positive rate of the MOD criterion, some radiologists have recently attempted to determine another size criterion, the maximal mural thickness (MMT) of the appendix[8–10].
The purpose of this study was to evaluate the diagnostic value of the MOD and the MMT measurements of the appendix in children with clinical suspicion of acute appendicitis and to determine the optimal cut-off values of these measurements in diagnosis of acute appendicitis.
Among the abdominal US of the children who visited our institute for acute abdominal pain and the suspicion of acute appendicitis between July 2004 and November 2008, we selected 160 children who had a visible appendix on US. These children were aged 1-17 years (84 males, 76 females; mean age, 7.38 years).
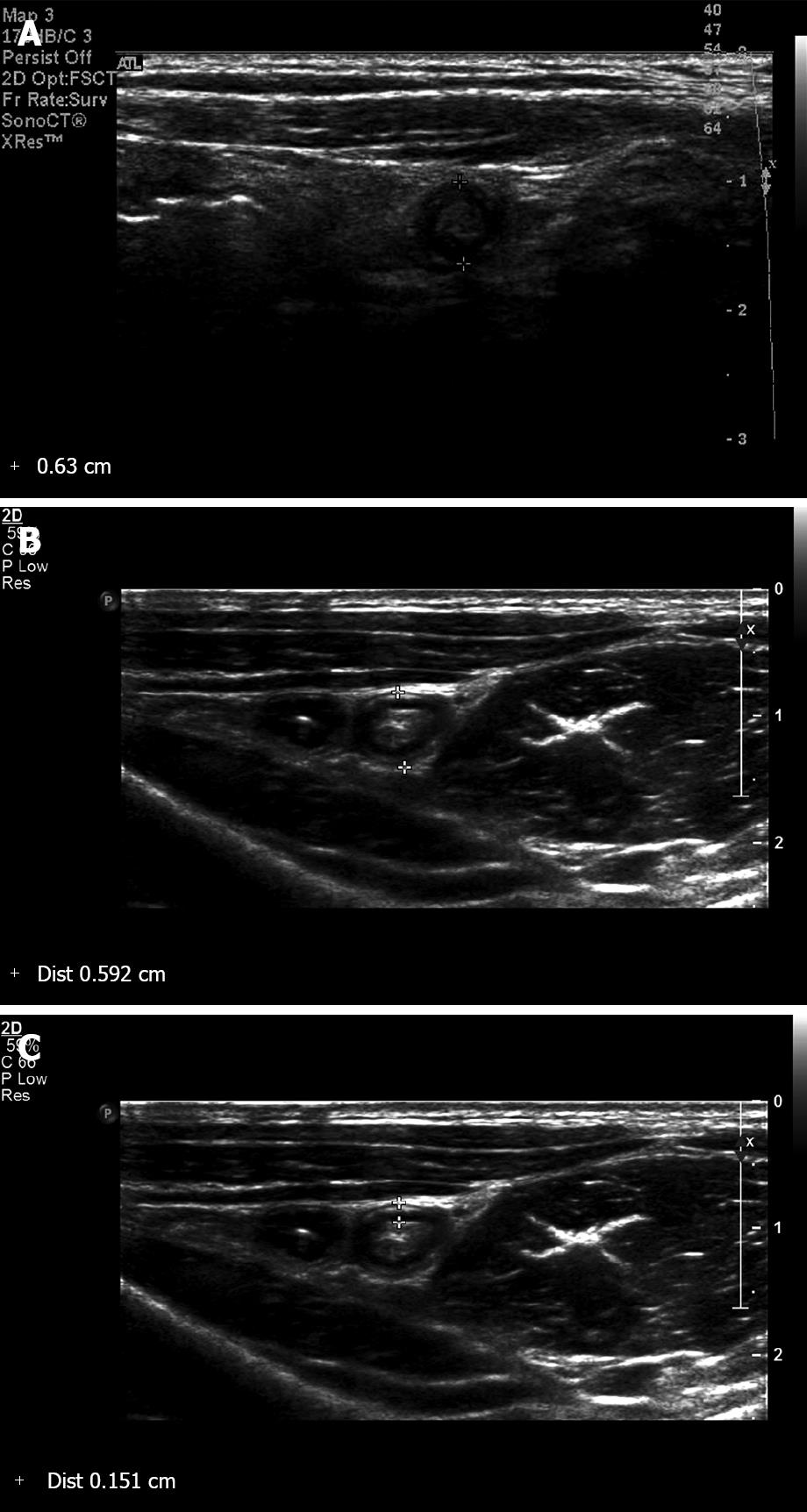
After receiving informed consent, the children were examined by experienced radiologists with three different US units (iU22, Philips Medical Systems, Andover, MA, USA; HDI 5000 SonoCT, Philips Medical Systems, Best, The Netherlands; ATL HDI 5000, Philips Medical Systems, Andover, MA, USA). The appendix was scanned from the base to the tip under graded compression using a high resolution transducer (9-12 MHz linear transducer or a 5-8 MHz sector transducer). Then the MOD and the MMT were measured at the thickest point in the cross-sectional image (Figure 1). The MOD was defined as the distance between the outer hyperechoic borders of the the appendix, and the MMT was defined as the distance from the hyperechoic luminal interface to the outer hyperechoic border. Intra-luminal contents including fluid, gas, feces, stones or nothing were recorded.
The medical records of the patients were traced till the symptoms were resolved. We categorized the patients into two groups: patients who had surgery (surgical appendix group) and patients who recovered without surgery (non-surgical appendix group). Data were analyzed by MedCalc v.9.3 software (MedCalc, Mariakerke, Belgium). We used the rank sum test (Mann-Whitney test) to evaluate the difference in the MOD and the MMT between the two groups and used ROC curve analysis to determine the optimal cut-off values of the MOD and the MMT for diagnosing acute appendicitis.
The MOD and the MMT of 164 appendixes in 160 children were included in this study. Forty-four children underwent an appendectomy. The pathological diagnoses were 15 cases of acute appendicitis (without any comment), six cases of acute early appendicitis, 13 cases of acute suppurative appendicitis, six cases of acute gangrenous appendicitis, two cases of acute gangrenous appendicitis with perforation, one case of acute necrotizing appendicitis and one case of congestion. As congestion did not contain any inflammatory cells, the case of congestion was re-classified in the non-surgical appendix group. The case of congestion was finally diagnosed with Crohn’s disease in the ileum and cecum. As a result, there were 121 appendixes (73.8%) in the non-surgical appendix group and 43 appendixes (26.2%) in the surgical appendix group.
Because each reference interval of the MOD and the MMT rejected normality (P < 0.0001 in each case), the Mann-Whitney test was used for the statistical analysis.
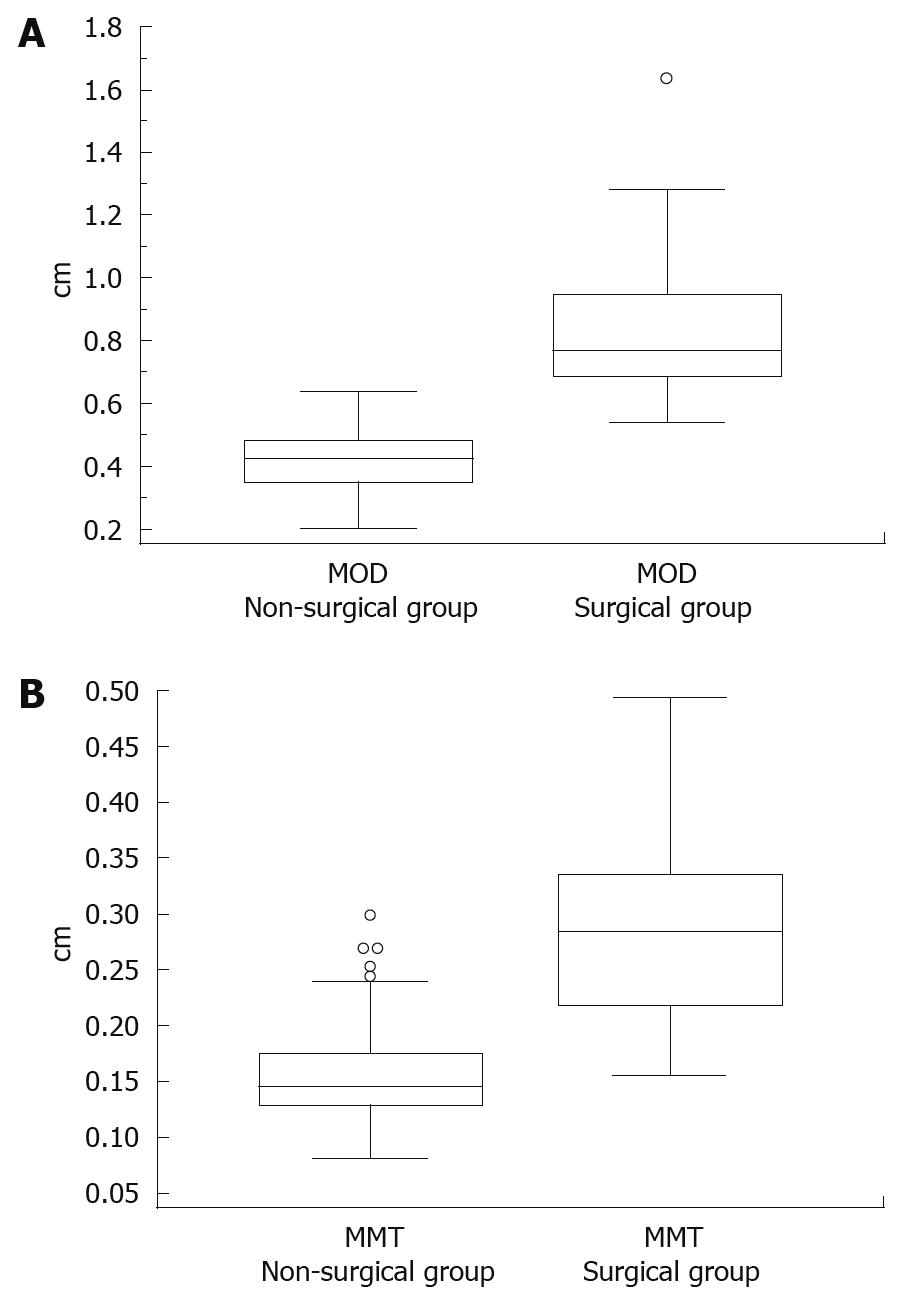
The range of the MOD was 0.20-1.45 cm in all patients, 0.20-0.69 cm in the non-surgical appendix group and 0.42-1.45 cm in the surgical appendix group. The median MOD of 0.37 cm (95% CI: 0.29-0.45 cm) in the non-surgical appendix group was significantly different (P < 0.0001) from the median MOD of 0.76 cm (95% CI: 0.69-0.90 cm) in the surgical appendix group. The data comparison graphs between the two groups were presented in Figure 2A.
The range of the MMT was 0.08-0.58 cm in all patients, 0.08-0.49 cm in the non-surgical appendix group and 0.10-0.58 cm in the surgical appendix group. The median MMT of 0.15 cm (95% CI: 0.13-0.17 cm) in the non-surgical appendix group was significantly different (P < 0.0001) from the median MMT of 0.33 cm (95% CI: 0.30-0.38 cm) in the surgical appendix group. The data comparison graphs between the two groups were presented in Figure 2B.
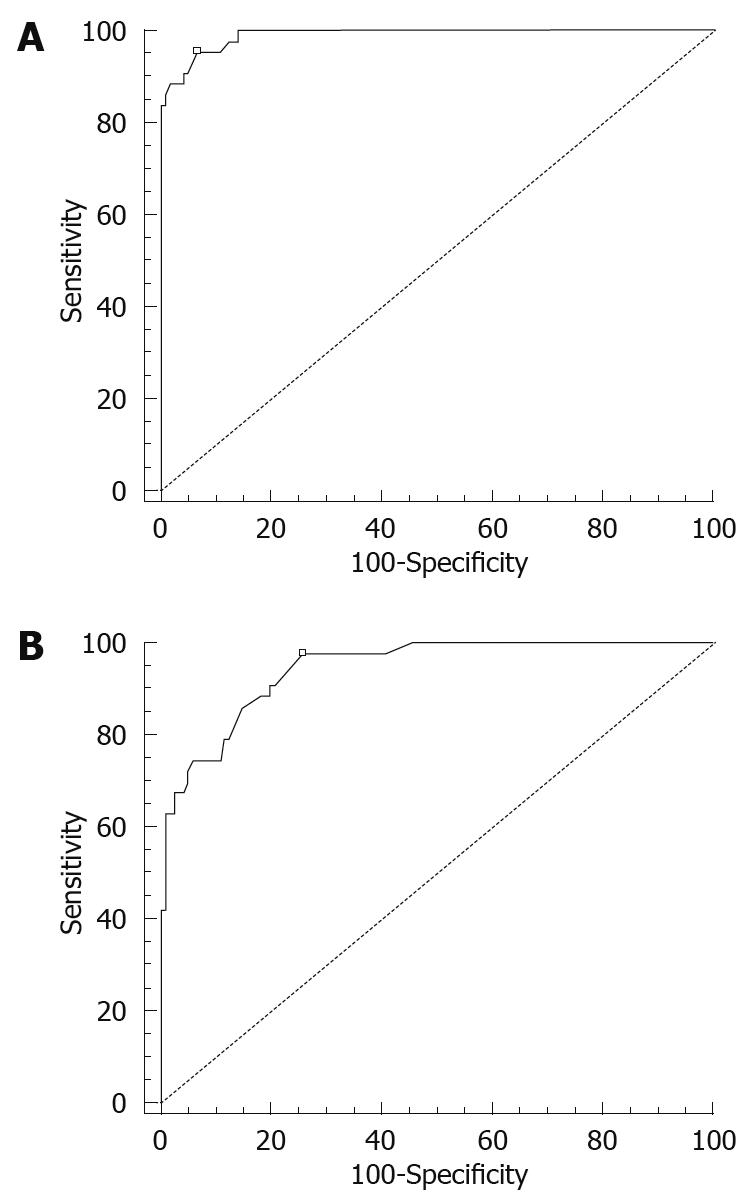
By ROC curve analysis, the optimal cut-off MOD was 0.57 cm with 89.6% sensitivity, 93.2% specificity and a 13.1 positive likelihood ratio (Figure 3A). The optimal cut-off MMT was 0.22 cm with 84.6% sensitivity, 95.8% specificity and a 20.1 positive likelihood ratio (Figure 3B).
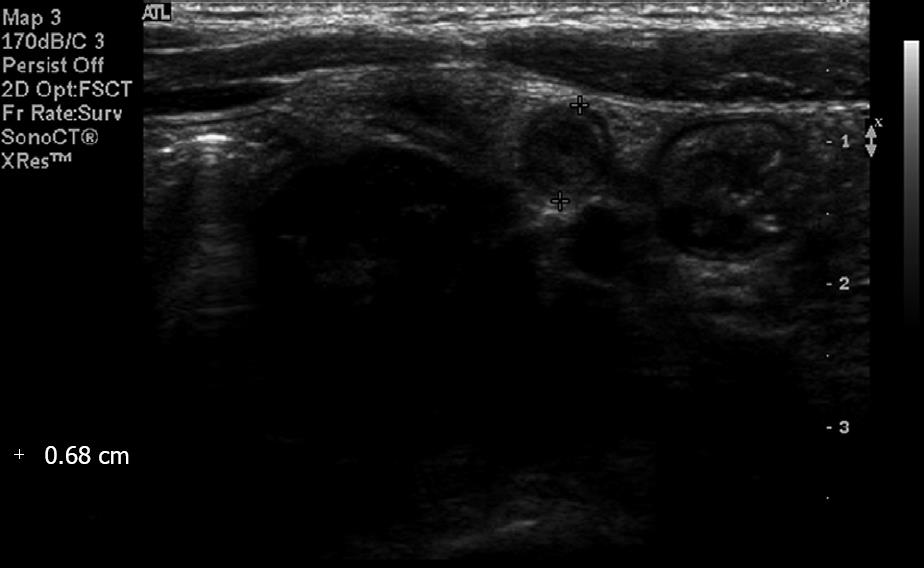
According to previous reports[1–411], the diagnosis of acute appendicitis by US is based on the following findings; the MOD of the appendix > 0.6 cm; the appendix cannot be compressed with manual pressure by the examiner; the cross-sectional shape of the appendix is round rather than oval; there is an absence of gas in the appendiceal lumen; and there is hyperperfusion of the appendiceal wall on a Doppler study. However, the most credible criterion, the MOD, may be exaggerated and inaccurate in certain conditions (Figure 4)[5–7].
Earlier, Park et al[10] suggested that the MMT may have a role as a useful adjunctive measurement, especially for patients with fecal-impacted, non-inflammatory appendixes. As well as this study, there have been several research studies measuring the MMT in children. Simonovský[8] reported that the difference in the normal appendiceal MMT between a group of young children and adolescents and an adult group was marginally significant (P = 0.042). In addition, the investigator stated that an MMT < 3 mm should be regarded as normal in children aged six years or younger. Wiersma et al[9] also reported the sizes of the MOD and the MMT of a normal appendix in children as 0.21-0.64 cm and 0.11-0.27 cm, respectively. However, they studied only normal appendixes.
In our study, we examined data for both diseased and disease-free appendixes on a large scale, and we compared the MOD and MMT between the surgical appendix and the non-surgical appendix. In a statistical analysis, both the MMT and the MOD had diagnostic value for acute appendicitis in children.
In addition, we were able to obtain the optimal cut-off MOD and MMT values for diagnosing acute appendicitis in pediatric patients. By ROC curve analysis, the optimal cut-off MOD was 0.57 cm with 89.6% sensitivity, 93.2% specificity and a 13.1 positive likelihood ratio. The optimal cut-off MMT was 0.22 cm with 84.6% sensitivity, 95.8% specificity and a 20.1 positive likelihood ratio. Considering that literature during the last three years has reported that the sensitivity and the specificity for diagnosis of acute appendicitis with US were 80%-100% and 86.5%-100%[1012–19], our study showed acceptable sensitivity and specificity. While we expected that the MMT would be more sensitive than the MOD, the MMT was less sensitive but more specific than the MOD. We presumed that the MMT could only decrease the false positive ratio of the MOD and could not affect the false negative ratio as the MOD was more sensitive. Therefore, in children, an MOD > 0.57 cm suggests the presence of acute appendicitis and an MMT > 0.22 cm enhances the possibility of having acute appendicitis.
There were several limitations to this study. At first, because our data were obtained only from visible appendixes on US, cases of perforated appendicitis were excluded. Secondly, we categorized patients according to the results of surgery, and therefore cases of chronic or abortive appendicitis may be categorized in the non-surgical appendix group. Thirdly, because the examiner was not one radiologist, inter-observer variance still exists.
In conclusion, the MOD and the MMT are reliable criteria for diagnosis of acute appendicitis in children. An MOD > 0.57 cm and an MMT > 0.22 cm are the optimal criteria.
US became a reliable modality for diagnosing acute appendicitis, especially in doubtful cases for clinicians. When the maximal outer diameter (MOD) of the appendix is larger than 0.6 cm, radiologists suggest the presence of acute appendicitis. However, because the MOD may be larger than 0.6 cm without acute inflammation, the maximal mural thickness (MMT) of the appendix has been evaluated as another size criterion.
Dr. Wiersma and colleagues in Juliana Children’s hospital in The Netherlands reported the sizes of the MOD and the MMT in the normal appendix. Dr. Park and colleagues in Kwandong University Myongji Hospital in South Korea suggested that the MMT may play a role as a useful measurement for the fecal-impacted, non-inflammatory appendix. However, they included only normal appendixes. The authors examined data from both diseased and disease-free appendixes on a large scale to evaluate the MMT and the MOD and to determine the optimal cut-off values of these measurements in the diagnosis of acute appendicitis in children.
The MOD and the MMT are reliable criteria for diagnosing acute appendicitis in children. An MOD > 0.57 cm and an MMT > 0.22 cm are the optimal criteria.
The authors demonstrated the usefulness of measurements of MOD and MMT in diagnosing pediatric acute appendicitis. They compared the MOD and MMT between surgical and non-surgical appendix groups and showed significant differences between the two groups. They also determined optimal cut-off value of MOD and MMT for diagnosis of acute appendicitis. The manuscript was well organized and well written.
| 1. | Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology. 1986;158:355-360. |
| 2. | Jeffrey RB Jr, Laing FC, Townsend RR. Acute appendicitis: sonographic criteria based on 250 cases. Radiology. 1988;167:327-329. |
| 3. | Rettenbacher T, Hollerweger A, Macheiner P, Gritzmann N, Daniaux M, Schwamberger K, Ulmer H, zur Nedden D. Ovoid shape of the vermiform appendix: a criterion to exclude acute appendicitis--evaluation with US. Radiology. 2003;226:95-100. |
| 4. | Rettenbacher T, Hollerweger A, Macheiner P, Rettenbacher L, Tomaselli F, Schneider B, Gritzmann N. Outer diameter of the vermiform appendix as a sign of acute appendicitis: evaluation at US. Radiology. 2001;218:757-762. |
| 5. | Hahn HB, Hoepner FU, Kalle T, Macdonald EB, Prantl F, Spitzer IM, Faerber DR. Sonography of acute appendicitis in children: 7 years experience. Pediatr Radiol. 1998;28:147-151. |
| 6. | Rioux M. Sonographic detection of the normal and abnormal appendix. AJR Am J Roentgenol. 1992;158:773-778. |
| 7. | Simonovský V. Sonographic detection of normal and abnormal appendix. Clin Radiol. 1999;54:533-539. |
| 8. | Simonovský V. Normal appendix: is there any significant difference in the maximal mural thickness at US between pediatric and adult populations? Radiology. 2002;224:333-337. |
| 9. | Wiersma F, Srámek A, Holscher HC. US features of the normal appendix and surrounding area in children. Radiology. 2005;235:1018-1022. |
| 10. | Park NH, Park CS, Lee EJ, Kim MS, Ryu JA, Bae JM, Song JS. Ultrasonographic findings identifying the faecal-impacted appendix: differential findings with acute appendicitis. Br J Radiol. 2007;80:872-877. |
| 11. | Rettenbacher T, Hollerweger A, Macheiner P, Rettenbacher L, Frass R, Schneider B, Gritzmann N. Presence or absence of gas in the appendix: additional criteria to rule out or confirm acute appendicitis--evaluation with US. Radiology. 2000;214:183-187. |
| 12. | Yu SH, Kim CB, Park JW, Kim MS, Radosevich DM. Ultrasonography in the diagnosis of appendicitis: evaluation by meta-analysis. Korean J Radiol. 2005;6:267-277. |
| 13. | Assefa G, Meseret S, Nigussie Y. The role of ultrasound in diagnosing acute appendicictis. Ethiop Med J. 2006;44:67-74. |
| 14. | Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, Babyn PS, Dick PT. US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis. Radiology. 2006;241:83-94. |
| 15. | Peletti AB, Baldisserotto M. Optimizing US examination to detect the normal and abnormal appendix in children. Pediatr Radiol. 2006;36:1171-1176. |
| 16. | Chang YJ, Kong MS, Hsia SH, Wu CT, Lai MW, Yan DC, Chao HC, Chen CC, Chen SY. Usefulness of ultrasonography in acute appendicitis in early childhood. J Pediatr Gastroenterol Nutr. 2007;44:592-595. |
| 17. | Johansson EP, Rydh A, Riklund KA. Ultrasound, computed tomography, and laboratory findings in the diagnosis of appendicitis. Acta Radiol. 2007;48:267-273. |
| 18. | Mardan MA, Mufti TS, Khattak IU, Chilkunda N, Alshayeb AA, Mohammad AM, ur Rehman Z. Role of ultrasound in acute appendicitis. J Ayub Med Coll Abbottabad. 2007;19:72-79. |
| 19. | Khanal BR, Ansari MA, Pradhan S. Accuracy of ultrasonography in the diagnosis of acute appendicitis. Kathmandu Univ Med J (KUMJ). 2008;6:70-74. |