Published online May 14, 2009. doi: 10.3748/wjg.15.2265
Revised: March 12, 2009
Accepted: March 19, 2009
Published online: May 14, 2009
AIM: To evaluate the efficacy of cola treatment for gastric phytobezoars, including diospyrobezoars.
METHODS: A total of 17 patients (range: 48 to 78 years) with symptomatic gastric phytobezoars treated with cola and adjuvant endoscopic therapy were reviewed. Three liters of cola lavage (10 cases) or drink (7 cases) were initially used, and then endoscopic fragmentation was done for the remnant bezoars by using a lithotripsy basket or a polypectomy snare. The overall success of dissolving a gastric phytobezoars with using three liters of cola and the clinical and endoscopic findings were compared retrospectively between four cases of complete dissolution by using only cola and 13 cases of partial dissolution with cola.
RESULTS: After 3 L of cola lavage or drinking, a complete dissolution of bezoars was achieved in four patients (23.5%), while 13 cases (76.5%) were only partially dissolved. Phytobezoars (4 of 6 cases) were observed more frequently than diospyrobezoars (0 of 11) in the group that underwent complete dissolution (P = 0.006). Gender, symptom duration, size of bezoar and method of cola administration were not significantly different between the two groups. Twelve of 13 patients with residual bezoars were completely treated with a combination of cola and endoscopic fragmentation.
CONCLUSION: The rate of complete dissolution with three liters of cola was 23.5%, but no case of diospyrobezoar was completely dissolved using this method. However, pretreatment with cola may be helpful and facilitate endoscopic fragmentation of gastric phytobezoars.
- Citation: Lee BJ, Park JJ, Chun HJ, Kim JH, Yeon JE, Jeen YT, Kim JS, Byun KS, Lee SW, Choi JH, Kim CD, Ryu HS, Bak YT. How good is cola for dissolution of gastric phytobezoars? World J Gastroenterol 2009; 15(18): 2265-2269
- URL: https://www.wjgnet.com/1007-9327/full/v15/i18/2265.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.2265
Bezoars are hard masses or concretions of indigestible food, vegetable fiber or hair that are found in the gastrointestinal (GI) tract, usually in the stomach. Although the incidence of bezoars is unknown, the reported incidence is about 0.4%[1]. Bezoars are usually classified into four types according to their composition: phytobezoars, trichobezoars, medication bezoars and lactobezoars. Dissolution therapy with proteolytic or cellulase enzymes[2], endoscopic fragmentation or aspiration and surgery have been proposed as the treatment options for bezoars, and these treatments have a wide range of efficacy[3]. Ingestion of persimmons is considered the most common cause of phytobezoars in some countries[45]. Because of their hard consistency, endoscopic therapy with fragmentation or enzymatic dissolution is challenging and sometimes mechanical fragmentation cannot be accomplished.
Recently, dissolution bezoars with cola has been described to be one of the effective treatment options for the treatment of gastric phytobezoars. However, only commentaries on individual cases or small number of cases have been reported on the cola dissolution of phytobezoars[6–12]. To elucidate the efficacy of cola for dissolving phytobezoars, further evaluations with large number cases are needed. Here, we report the clinical results of 17 consecutive patients with gastric phytobezoars, including diospyrobezoars, who were initially treated by three liters of cola gastric lavage or drink.
The medical records of 17 patients with gastric phytobezoars treated by cola gastric lavage at Korea University Hospital, Seoul, between 2002 and 2008 were retrospectively reviewed. Diagnosis and classification of gastric bezoars were based upon clinical and endoscopic findings. Diospyrobezoar was diagnosed by history of eating persimmons and the endoscopic typical characteristics such as cemented seeds of persimmon or hard consistency or darkish-brown color. The size of each bezoar was grossly estimated as occupied percentage of the lumen of the stomach. The patients’ median age was 63 years (range: 48-78). Seven patients had a long-standing history of diabetes mellitus (DM), four had a history of arterial hypertension (AHT) and the other patients had no significant past or concurrent diseases. On the initial endoscopic evaluation, 11 cases had darkish-brown colored diospyrobezoar and 6 cases had bright brown or yellow colored phytobezoars (Table 1). After diagnosing the bezoar, two nasogastric tubes (16 F) were placed for performing gastric cola lavage. One tube was used for the continuous administration of cola, and the other for natural drainage. A lavage with three liters of cola was performed over 12 h. All the procedures were done after obtaining informed consent from all the patients. Among the 17 patients, 8 patients drank the three liters of cola as they had refused to have the nasogastric tube inserted (Table 2). The nine patients with nasogastric tubes were kept in the recumbent position to prevent aspiration. The patients with DM had blood glucose monitoring by a glucometer. One day after the lavage with three liters of cola (or after drinking the same amount of cola), second-look endoscopic examinations were performed for assessing the bezoar. The status of the bezoars was then described, i.e. whether or not the bezoar remained in place, and whether it had changed its size and consistency. When the bezoar had disappeared, we considered this as complete dissolution. When it had a decreased size and a softened consistency by palpation with the biopsy forcep, then the response was considered as partial dissolution. If no change of the size and consistency was observed, then this was considered as lack of response. As the result of the initial administration of cola, patients were divided into two groups, i.e with either complete dissolution or partial dissolution. The clinical and endoscopic features and the method of cola administration were then retrospectively compared between two groups.
| Case no. | Gender | Age | Symptoms | Duration (d) | Comorbidity | Type of bezoar | Endoscopic findings | Size of bezoar |
| CD group | ||||||||
| 1 | F | 69 | Indigestion | 21 | None | Phytobezoar | GU | Above 50% |
| 2 | F | 62 | Epigastric soreness | 21 | DM | Phytobezoar | GU | Above 50% |
| 3 | F | 49 | Indigestion, epigastric soreness | 14 | DM | Phytobezoar | Pyloric stenosis | Below 50% |
| 4 | F | 51 | Indigestion | 20 | DM | Phytobezoar | GU | Below 50% |
| PD group | ||||||||
| 5 | M | 48 | Epigastric soreness | 8 | None | Phytobezoar | DU scar with stenosis | Below 50% |
| 6 | F | 57 | Indigestion | 21 | None | Diospyrobezoar | Pyloric stenosis | Above 50% |
| 7 | M | 71 | Indigestion | 90 | None | Diospyrobezoar | Pyloric stenosis | Below 50% |
| 8 | F | 65 | Epigastric soreness | 10 | HTN | Diospyrobezoar | Pyloric stenosis | Above 50% |
| 9 | F | 61 | Indigestion | 14 | DM | Diospyrobezoar | Pyloric stenosis | Below 50% |
| 10 | F | 57 | Indigestion | 21 | None | Diospyrobezoar | Pyloric stenosis | Below 50% |
| 11 | F | 67 | Epigastric soreness | 60 | DM | Diospyrobezoar | GU | Below 50% |
| 12 | M | 63 | Epigastric soreness | 21 | HTN | Phytobezoar | Pyloric stenosis | Above 50% |
| 13 | M | 78 | Indigestion | 30 | DM | Diospyrobezoar | GU | Above 50% |
| 14 | F | 75 | Epigastric soreness | 90 | DM | Diospyrobezoar | None | Below 50% |
| 15 | F | 54 | None | 7 | HTN | Diospyrobezoar | GU | Below 50% |
| 16 | F | 61 | Nausea and vomiting | 7 | None | Diospyrobezoar | GU | Below 50% |
| 17 | M | 63 | Epigastric soreness | 30 | None | Diospyrobezoar | Pyloric stenosis | Above 50% |
| Case no. | Initial methodof colaadministration | Methods ofendoscopic treatment | Endoscopicprocedure time (min) | No. ofendoscopicsessions (n) | No. of used instruments(n) | Total amount of administered cola (liters) | Hospitalstay (d) |
| CD group | |||||||
| 1 | 3 L drink | 0 | 0 | 3 | 2 | ||
| 2 | 3 L lavage | 0 | 0 | 3 | 2 | ||
| 3 | 3 L lavage | 0 | 0 | 3 | 3 | ||
| 4 | 3 L lavage | 0 | 0 | 3 | 2 | ||
| PD group | |||||||
| 5 | 3 L drink | Mechanical lithotripsy | 8 | 1 | 1 | 6 | 3 |
| 6 | 3 L lavage | Mechanical lithotripsy | 45 | 1 | 1 | 6 | 3 |
| 7 | 3 L drink | Mechanical lithotripsy | 14 | 1 | 2 | 6 | 2 |
| 8 | 3 L lavage | Mechanical lithotripsy | 44 | 1 | 1 | 6 | 3 |
| 9 | 3 L drink | Mechanical lithotripsy | 62 | 1 | 2 | 6 | 4 |
| 10 | 3 L lavage | Mechanical lithotripsy | 42 | 1 | 1 | 6 | 3 |
| 11 | 3 L lavage | Mechanical lithotripsy | 50 | 1 | 1 | 6 | 7 |
| 12 | 3 L lavage | Mechanical lithotripsy | 30 | 1 | 1 | 6 | 3 |
| 13 | 3 L lavage | Polypectomy snare | 52 | 2 | 2 | 9 | 3 |
| 14 | 3 L drink | Polypectomy snare | 40 | 2 | 3 | 6 | 5 |
| 15 | 3 L drink | Polypectomy snare | 58 | 2 | 3 | 9 | 5 |
| 16 | 3 L drink | Polypectomy snare | 62 | 1 | 4 | 6 | 5 |
| 17 | 3 L drink | Polypectomy snare | 72 | 2 | 5 | 6 | 3 |
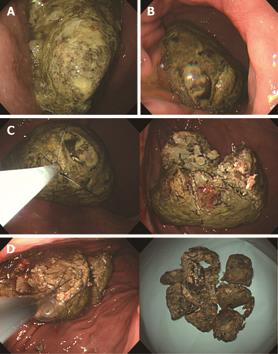
The endoscope we used was an Olympus GIF Q 260 or a H 260 (Olympus, Tokyo, Japan). If a residual bezoar was observed, then endoscopic fragmentation was done using a lithotripsy basket (GML-90-26-180, Medi-Globe, Achenmuhle, Germany) or a polypectomy snare (SD-5L-1, Olympus, Japan) (Figure 1A and B). Finally, fragmented bezoars were crushed and retrieved with a biopsy forcep or a pentagon grasping forcep (Figure 1C and D). After the procedures, all the patients were advised to drink an additional 3 L of cola. Re-examination endoscopy was done one day after the procedures. All the endoscopic procedures were performed by three expert endoscopists.
Fisher exact test and the Mann-whitney U test were used for the comparison of clinical, endoscopic, and method of administration of cola. P < 0.05 were regarded as statistically significant.
After lavage with (or drinking) 3 L of cola, a complete dissolution was observed in four patients (23.5%), whereas 13 cases were partially dissolved with cola, i.e. their size was grossly decreased and their consistency was more softened than that observed before treatment (Figure 1A and B). The clinical characteristics of patients with complete dissolution (CD) and partial dissolution (PD) are compared and summarized in Table 2. The complete dissolution was observed in 4 out of 6 cases of phytobezoars, but no complete dissolution was noted in diospyrobezoars (P = 0.006). Other parameters, including age, gender, size of bezoar, endoscopic findings and the method of cola administration, were not different between the two groups (Table 3). Among the 13 cases with residual bezoars, eleven were completely treated with one endoscopic session and additional drink of three liters of cola. Four patients (case 13, 14, 15, 17) needed two endoscopic sessions to completely disrupt the bezoar.
| CD group (n = 4) | PD group (n = 13) | Pvalue | |
| Age, range (yr) | 51-69 | 48-78 | 0.412 |
| Gender (M:F) | 0:4 | 5:8 | 0.208 |
| Symptom duration, range (d) | 14-21 | 7-90 | 0.624 |
| Median (d) | 20 | 21 | |
| Type of bezoar | 0.006 | ||
| Phytobezoar | 4 | 2 | |
| Diospyrobezoar | 0 | 11 | |
| Size of bezoar | 0.559 | ||
| Over than 50% of stomach | 2 | 5 | |
| Less than 50% of stomach | 2 | 8 | |
| Endoscopic findings | 0.241 | ||
| GU | 3 | 5 | |
| Gastric outlet stenosis | 1 | 8 | |
| Method of administration of cola | 0.441 | ||
| Lavage | 3 | 6 | |
| Oral drink | 1 | 7 |
Thirteen out of 14 (91.6%) patients were completely cured with a combination of cola and endoscopic treatment. The mean endoscopic procedure time was 44.53 ± 18.56 min and the mean number of used accessories was 2.07 ± 1.02. No procedure-related complications developed, such as hemorrhage, perforation and small bowel obstruction. The mean hospital stay of all patients was 3.52 ± 1.32 d.
In another patient (case 17), the decreased size and softened consistency of the bezoar was observed after an initial lavage with three liters of cola lavage, but the endoscopic breakage failed (Figure 2A and B). So, 100 mL of cola were directly injected into the bezoar using an endoscopic needle and six additional liters of cola were administered orally for two days. On the fourth day, the bezoar still remained in place, with only partial resolution (Figure 2C). Because the patient refused an additional endoscopic treatment with cola, the bezoar was removed by surgery.
The treatment modalities for gastric bezoars include endoscopic therapy with fragmentation, medical treatment by enzymatic dissolution and surgery[13]. Various endoscopic methods and instruments for breaking up bezoars have been reported, including lithotripsy with basket[14], endoscopic suction removal with large-channel endoscopy[15], polypectomy snare[16] and biopsy forceps. However, these procedures are time-consuming. Furthermore, procedure-related complications may develop, such as bleeding, overtube-associated complications and intestinal obstruction caused by the fragmented, residual bezoars. In addition, chemical dissolution usually requires a long period of time and complications may develop, such as electrolyte imbalance, gastric ulcer and bleeding. The reported efficacy of chemical dissolution is variable[317].
Recently, Ladas et al[6] reported a five cases of gastric phytobezoars successfully dissolved by lavage with three liters of cola. Since then, there were six reports written in English and describing the treatment of gastric bezoars with cola. However, reports on cola dissolution have been limited to individual case reports. Methods and results are summarized in Table 4.
| Author | Type of bezoars | No. of cases | Methods of administration of Coca-cola | Duration of Coca-cola |
| Ladas et al[6] | Phytobezoar | 5 | 3 L of Coca-cola lavage | 12 h |
| Kato et al[7] | Diospyrobezoars | 1 | 3 L of Coca-cola lavage | 12 h |
| Chung et al[8] | Diospyrobezoars | 1 | Injection of 30 mL of Coca-cola and drinking 4 L of Coca-cola | 2 d |
| Lin et al[9] | Diospyrobezoars | 1 | Injection and irrigation with 1 can of Coca-cola + oral drink of 1 can | |
| Okamoto et al[10] | Diospyrobezoars | 1 | Drinking 500 mL of Coca-cola per day | 7 d |
| Sechopoulos et al[11] | Stump of vegetables | 1 | 2 cans of Coca-cola injection | |
| Whitson et al[12] | Phytobezoar | 1 | Drinking 5 L of Coca-cola per day | 5 d |
In this series, we report the clinical results of 17 gastric phytobezoars treated with cola. To our knowledge, this is largest study ever on this topic. The therapeutic efficacy of a lavage with three liters of cola (or of drinking the same amount), to achieve the complete dissolution of bezoars, was only 23.5%. Compared with previous reports, our success rate is very low. The reason for this low therapeutic efficacy of cola may be due to the fact that most cases of our series were diospyrobezoars (13 out of 17 cases, 76.4%), and in fact we failed to observe the complete dissolution of diospyrobezoars using cola alone.
Diospyrobezoars following ingestion of persimmon are formed by the agglutination of the tannins in the skin of the fruit. Because of their hard consistency, endoscopic therapy with fragmentation or enzymatic dissolution is challenging and sometimes mechanical fragmentation cannot be accomplished. In a previous report, the efficacy of the combination of endoscopic fragmentation and pharmacotherapy was 80%[18]. There are four reports of cases in whom the complete dissolution of diospyrobezoars was carried out with cola (Table 4). The direct injection of small amounts of cola directly into the phytobezoars is also rapidly effective and safe[679]. However, in our experience, this technique was not effective for complete dissolving huge disopyrobezoar (case 17). So, in case of diospyrobezoars, complete dissolution might not be achieved with cola use alone.
Another reason for the low therapeutic efficacy may be the relatively short duration of cola administration. There were two successful dissolution cases with daily cola drinking for longer durations (7 d[10] and 3 mo[18]). A prolonged administration may have changed our clinical results, but it may also have induced metabolic disturbances due to the cola’s high caloric content. Also, a longer administration time may prolong the nil per os time and the length of hospital stay. So, we used the short duration of cola and combined it with the endoscopic fragmentation.
Cola alone could not dissolve completely all gastric phytobezoars. However, in our series, softened-consistency or decreased size was observed in all residual bezoars. So, endoscopic fragmentation and retrieval of the bezoars could be easily performed. Except for four cases, all the procedures were completed in only one session, with relative short procedure time. As the bezoars’ consistency was softened, disruption of accessories was prevented. So, these techniques are cost-effective when considering the length of the hospital stay, the number of endoscopic sessions and the used accessories. Also, using additional cola after endoscopic disruption may be helpful preventing small bowel obstruction due to daughter fragments.
Cola’s mechanism of dissolution of bezoars is not well understood. The suggested mechanisms are: (1) the mucolytic effect of NaHCO3, (2) the digestion of the bezoar by CO2 bubbles and (3) the cola’s acidity, which is similar to that of gastric acid[6].
In conclusion, the complete dissolution rate using three liters of cola was 23.5%, but no case of diospyrobezoars was completely dissolved. However, pretreatment with cola may be helpful and facilitate endoscopic fragmentation of gastric phytobezoars. A combination therapy of gastric phytobezoars with cola and endoscopic fragmentation is cost-effective and decreases the number of endoscopic sessions and accessories that are used as well as the hospital stay.
Ladas et al have first reported a case series of gastric phytobezoars that were successfully dissolved with cola lavage along with oral maintenance. Since then, there were several reports of gastric bezoar cases successfully treated only with cola.
The efficacy of cola for dissolving bezoars was very low compared with previous reports. There was no case of completely dissolved diospyrobezoar with cola. However, the use of cola for dissolving bezoars was cost-effective.
This study may suggest that dissolving gastric bezoars with cola alone is not the best treatment modality, especially for diospyrobezoars.
The study evaluated the efficacy of cola treatment for gastric phytobezoars. The study is well written and perhaps the largest experience todate.
| 1. | McKechnie JC. Gastroscopic removal of a phytobezoar. Gastroenterology. 1972;62:1047-1051. |
| 3. | Walker-Renard P. Update on the medicinal management of phytobezoars. Am J Gastroenterol. 1993;88:1663-1666. |
| 4. | Gayà J, Barranco L, Llompart A, Reyes J, Obrador A. Persimmon bezoars: a successful combined therapy. Gastrointest Endosc. 2002;55:581-583. |
| 5. | Zhang RL, Yang ZL, Fan BG. Huge gastric disopyrobezoar: a case report and review of literatures. World J Gastroenterol. 2008;14:152-154. |
| 6. | Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric Coca-Cola lavage. Eur J Gastroenterol Hepatol. 2002;14:801-803. |
| 7. | Kato H, Nakamura M, Orito E, Ueda R, Mizokami M. The first report of successful nasogastric Coca-Cola lavage treatment for bitter persimmon phytobezoars in Japan. Am J Gastroenterol. 2003;98:1662-1663. |
| 8. | Chung YW, Han DS, Park YK, Son BK, Paik CH, Jeon YC, Sohn JH. Huge gastric diospyrobezoars successfully treated by oral intake and endoscopic injection of Coca-Cola. Dig Liver Dis. 2006;38:515-517. |
| 9. | Lin CS, Tung CF, Peng YC, Chow WK, Chang CS, Hu WH. Successful treatment with a combination of endoscopic injection and irrigation with coca cola for gastric bezoar-induced gastric outlet obstruction. J Chin Med Assoc. 2008;71:49-52. |
| 10. | Okamoto Y, Yamauchi M, Sugihara K, Kato H, Nagao M. Is coca-cola effective for dissolving phytobezoars? Eur J Gastroenterol Hepatol. 2007;19:611-612. |
| 11. | Sechopoulos P, Robotis JF, Rokkas T. Gastric bezoar treated endoscopically with a carbonated beverage: case report. Gastrointest Endosc. 2004;60:662-664. |
| 12. | Whitson BA, Asolati M, Kandaswamy R, Sutherland DE. Diabetic gastroparesis-associated bezoar resolution via "cola-lysis". Clin Transplant. 2008;22:242-244. |
| 13. | Krausz MM, Moriel EZ, Ayalon A, Pode D, Durst AL. Surgical aspects of gastrointestinal persimmon phytobezoar treatment. Am J Surg. 1986;152:526-530. |
| 14. | Manbeck MA, Walter MH, Chen YK. Gastric bezoar formation in a patient with scleroderma: endoscopic removal using the gallstone mechanical lithotripter. Am J Gastroenterol. 1996;91:1285-1286. |
| 15. | Blam ME, Lichtenstein GR. A new endoscopic technique for the removal of gastric phytobezoars. Gastrointest Endosc. 2000;52:404-408. |
| 16. | Leichtmann GA, Novis BH, Freund J. Esophageal bezoar diagnosed and removed endoscopically. Gastrointest Endosc. 1986;32:432. |
| 17. | Zarling EJ, Moeller DD. Bezoar therapy. Complication using Adolph's Meat Tenderizer and alternatives from literature review. Arch Intern Med. 1981;141:1669-1670. |
| 18. | Lee HJ, Kang HG, Park SY, Yi CY, Na GJ, Lee TY, Kim SH, Song CS. [Two cases of phytobezoars treated by adminsitration of Coca-Cola by oral route]. Korean J Gastroenterol. 2006;48:431-433. |