INTRODUCTION
Hepatocellular carcinoma (HCC) is the sixth most common cancer worldwide[1]. Prognosis has been improved by careful follow-up of the high-risk patient, progress in diagnostic techniques, and combined modality therapy such as surgery, chemotherapy including transarterial chemoembolization (TACE), percutaneous ethanol injection therapy, and radiofrequency ablation. While recurrence of HCC is generally intrahepatic, long-term therapy increases the risk of extrahepatic metastases, and more than 50% of these occur in the lung[23]. While the most effective therapy for lung metastasis is surgical resection[4–7], Kawamura et al[5] reported that only 2.6% of patients with lung metastases can undergo this type of surgery. Most patients are not deemed suitable because of multiple lung metastases, uncontrolled intra-hepatic HCCs, and deterioration in liver function. Since the prognosis of extrahepatic tumors is poor, options are limited to palliation for many people. Most people will be forced to depend on the few available chemotherapy protocols suitable for this situation; there is no standardized effective chemotherapy regime. A recent pilot study found that S-1, a novel oral dihydropyridine dehydrogenase (DPD) inhibitor, and interferon-alpha (IFN-α) were associated with objective response in three of 12 patients with lung metastasis of HCC[8]. Accumulation of such reports may lead to a standard therapy being confirmed in the future. Ishikawa et al[9] previously reported combined chemotherapy with docetaxel, combined docetaxel, cisplatin (CDDP) and enteric-coated tegafur/uracil (UFT-E) for lung metastases of HCC. This chemotherapy regime was effective for lung metastases of HCC but not for the primary hepatic lesion; however, the reasons for this difference remain unknown. We report a case in which multiple lung metastases of HCC were completely resolved by modified combined chemotherapy with docetaxel, CDDP and UFT-E.
CASE REPORT
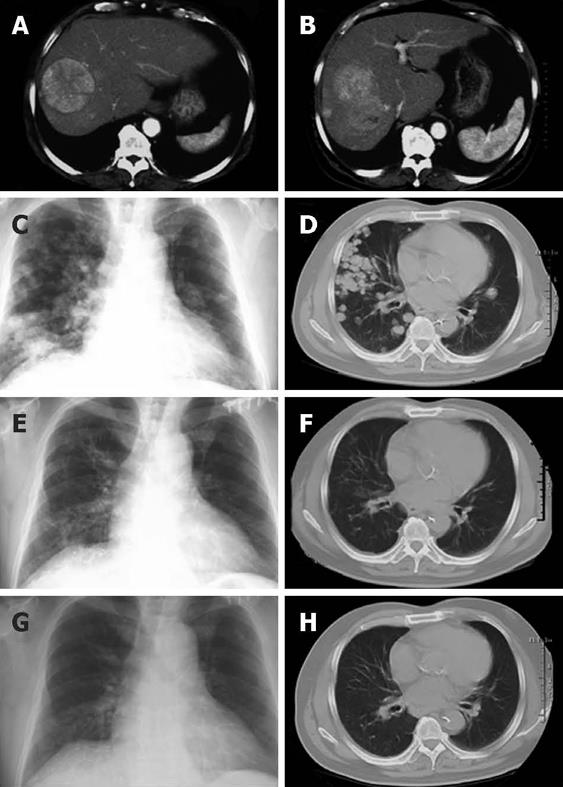
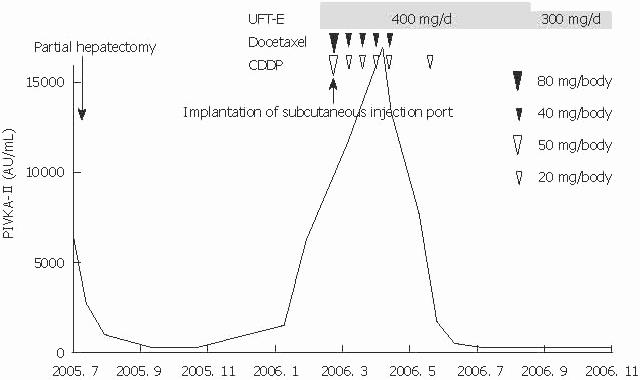
A 68-year-old man diagnosed with multiple lung metastases of HCC was admitted to Saiseikai-Niigata Daini Hospital in February 2006. He had undergone right hepatic lobectomy to remove three hepatocellular carcinomas (6 cm, 5 cm and 4 cm in diameter) 7 mo before the admission. Pathological diagnosis was moderately differentiated HCC, and clinical stage at the time of surgery was stage IVa according to the TNM classification. Tests for hepatitis B and C viral markers were all negative, but examination of the resected liver indicated cirrhosis, possibly caused by alcohol. Liver function test disclosed the following values: alanine aminotransferase 137 IU/L, alkaline phosphatase 503 IU/L, serum albumin 4.4 g/dL, and PT-INR 1.19 (Child-Pugh class A). While there was no elevation of tumor marker alpha-fetoprotein (4.3 ng/mL), protein induced by vitamin K absence II (PIVKA-II) was markedly elevated at 6280 mAU/L. Chest X-ray and computed tomography (CT) showed at least 50 metastases spread diffusely throughout the lungs (Figure 1). Since no treatment guidelines were available, we modified the combined chemotherapy with docetaxel, CDDP and UFT-E reported by Ishikawa et al[9] after obtaining informed consent. First, 400 mg/d of oral UFT-E was started. We then placed an intra-arterial catheter that delivered medication into the aorta just before the bronchial arteries, and docetaxel (80 mg/body initially, followed by 40 mg/body) and CDDP (50 mg/body initially, followed by 20 mg/body) were administered every 2 wk via a subcutaneous injection port (Figure 2). This was performed on an outpatient basis from the third injection. The serum level of PIVKA-II decreased 1 mo after starting chemotherapy and normalized after 4 mo. Two months after starting chemotherapy, chest X-ray and CT showed complete disappearance of the lung metastases (Figure 1). Adverse events during the therapy were grade 3 leukocytopenia (minimum white blood cell count was 2500/&mgr;L), grade 2 fatigue and anorexia, and grade 1 alopecia according to Common Terminology Criteria for Adverse Events v3.0 (CTCAE). Therapy was stopped after the fourth administration and only UFT-E was continued, in accordance with the patient’s wishes. This was also stopped 5 mo after starting chemotherapy, when chest X-ray and CT remained negative. Approximately 2 years after hepatic surgery, HCC reappeared in the liver and was treated with TACE; however, lung metastasis did not recur. The patient remains well and is being followed-up as an outpatient.
Figure 1 Chest X-ray and CT images before and after chemotherapy (A-H).
Seven months before the chemotherapy, huge multiple HCCs were apparent in the right lobe of the liver (A, B). On admission before chemotherapy, multiple lung metastases were seen in the bilateral lung fields (C, D). Two months after starting chemotherapy, the multiple lung metastases had disappeared completely (E, F). Five months after starting chemotherapy, the tumors had not recurred (G, H).
Figure 2 Clinical course of this patient.
First, 400 mg/d of oral UFT-E was started. We then placed an intra-arterial catheter that delivered medication into the aorta just before the bronchial arteries, and docetaxel (80 mg/body initially, followed by 40 mg/body) and CDDP (50 mg/body initially, followed by 20 mg/body) were administered every 2 wk via a subcutaneous injection port. Levels of PIVKA-II, a tumor marker, decreased rapidly 1 mo after starting chemotherapy; levels continued to fall to normal and were maintained.
DISCUSSION
The most effective therapy for lung metastasis of HCC is thought to be pulmonary resection[4–7], and this has been reported to prolong life in some cases[10]. However, the present patient was unsuitable for pulmonary resection because of multiple lung metastases. Reports of chemotherapy for lung metastasis of HCC are rare and most are case reports, indicating the absence of a highly effective standard therapy. Nonetheless, the literature contains reports of successful treatment of lung metastasis of HCC using tegaful/uracil[11], 5-fluorouracil (5-FU) + IFN[12], and 5-FU + CDDP + IFN[13]. Moreover, a pilot study of S-1 and IFN-α in patients with pulmonary metastases of HCC showed that three of 12 patients responded objectively[8]. There is also a report of the complete disappearance of multiple lung metastases with combined chemotherapy with docetaxel, CDDP and UFT-E[9]. In the present case, multiple lung metastases also disappeared in response to modified combined chemotherapy with docetaxel, CDDP, and UFT-E, suggesting that the effects of this combined chemotherapy are reproducible. We chose to modify the original intravenous combined chemotherapy including the docetaxel dose (original recommended dose was 60 mg/m2 of docetaxel, 80 mg/m2 of CDDP on day 1 and 400 mg/m2 per day of tegaful/uracil in consideration of adverse effects[9]. This original dose was determined by modifying the regime for advanced lung cancer[14]) since two patients who received this could not be treated effectively because of adverse events attributed to docetaxel (personal communication).To reduce the adverse events and increase treatment efficacy, we used an intra-arterial catheter that delivered medication to just before the bronchial arteries. In this way, docetaxel and CDDP could be administered in high concentration to the lung.
The precise mechanisms underlying the effectiveness of this therapy for lung metastasis of HCC are not known. It has been reported previously that the growth inhibition of hepatoma cells induced by docetaxel was mediated through G2/M-phase arrest, caspase activation and DNA fragmentation[15]. It is uncertain whether a single drug is sufficient, whether combinations of these agents are necessary, or whether docetaxel is the key drug. Furthermore, we do not know whether repeated doses or administration via the intra-arterial route improved the outcome for this patient. Further study is needed into the tumor characteristics of lung metastasis and immune responses in patients such as this one. While many issues must be resolved, this report is the second to document the effectiveness of combined chemotherapy with docetaxel, CDDP and UFT-E for lung metastasis of HCCs. This suggests that the present regime could be useful in this situation, as no highly effective standard therapy has been reported.
Peer reviewers: Satoshi Osawa, MD, First Department of Medicine, Hamamatsu University School of Medicine, 1-20-1 Handayama, Hamamatsu, 431-3192, Japan; Hitoshi Yoshiji, MD, PhD, Third Department of Internal Medicine, Nara Medical University, 840 Shijo-cho, Kashihara, Nara 634-8522, Japan; Akihito Tsubota, Assistant Professor, Institute of Clinical Medicine and Research, Jikei University School of Medicine, 163-1 Kashiwa-shita, Kashiwa, Chiba 277-8567, Japan
S- Editor Tian L L- Editor Logan S E- Editor Lin YP