Published online Feb 28, 2008. doi: 10.3748/wjg.14.1286
Revised: December 9, 2007
Published online: February 28, 2008
AIM: To study the relationship between the cytotoxin-associated gene-A (CagA) status of H pylori strains and cerebral infarction among European Caucasians and Chinese Han by conducting a meta-analysis.
METHODS: Ten case-control studies, with data on a total of 907 cases and 966 controls, were retrieved and considered; disqualified studies were excluded. The included studies were then tested for heterogeneity, and a meta-analysis was performed.
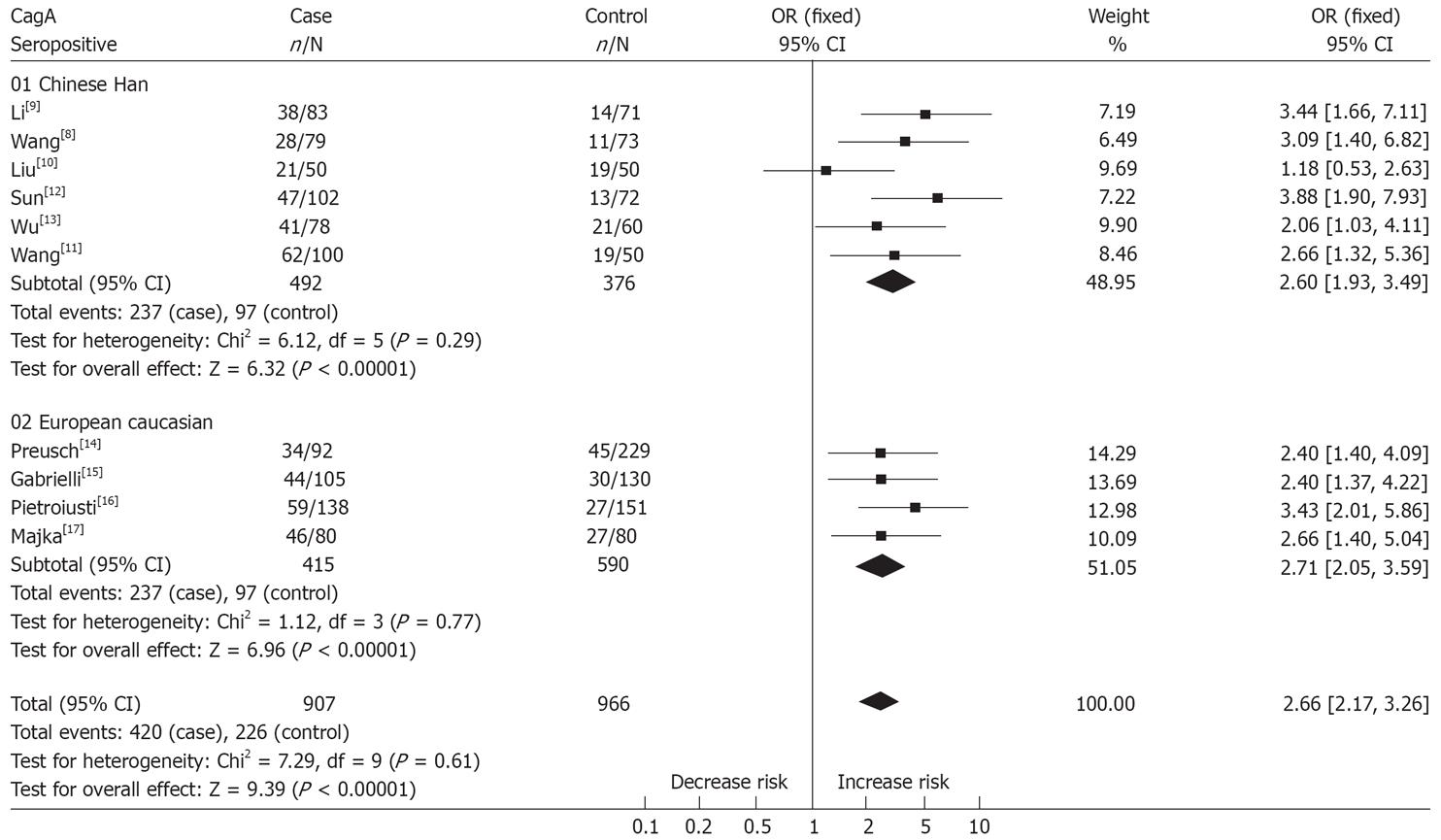
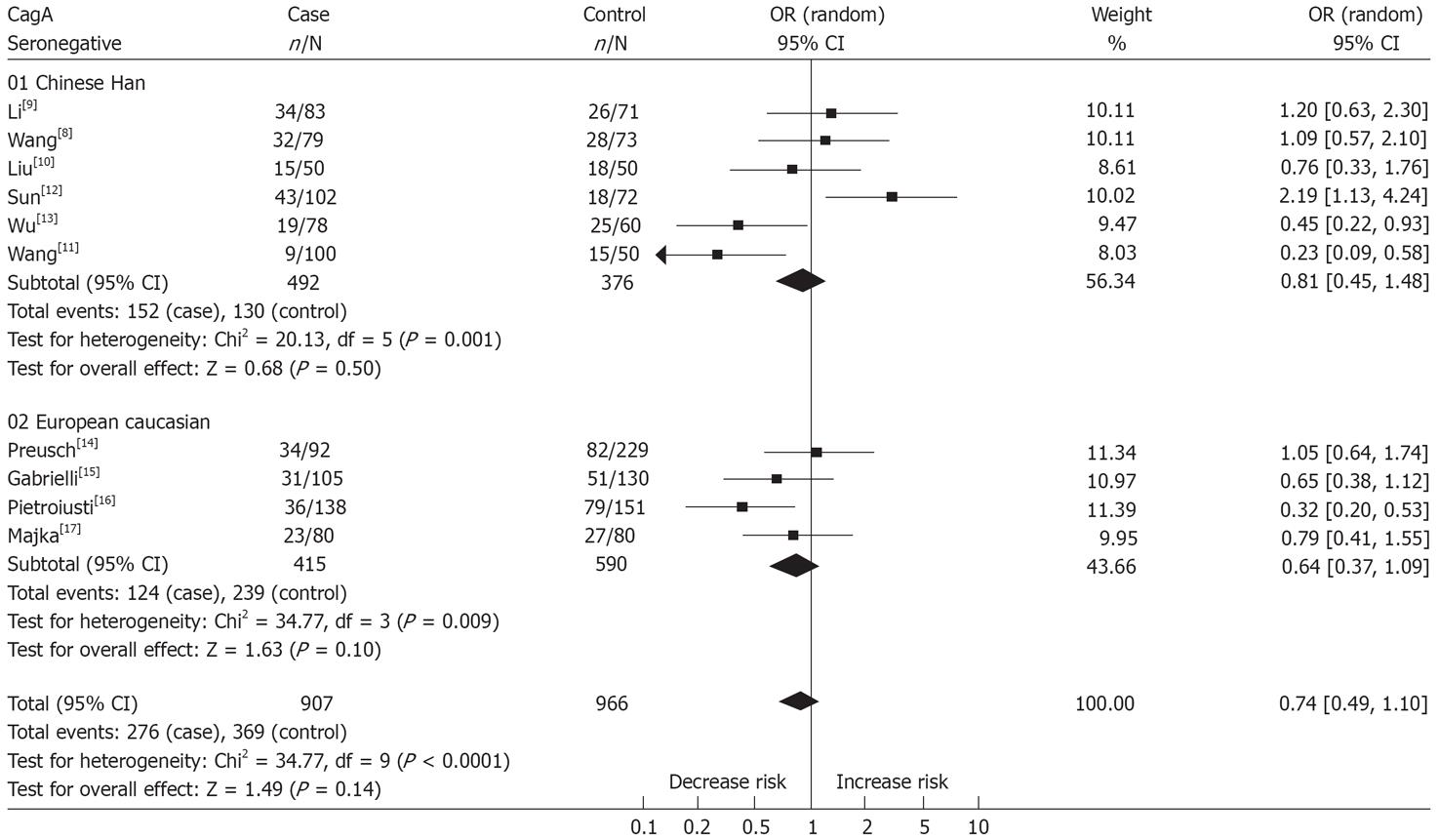
RESULTS: The combined data revealed CagA-bearing strains of H pylori which cause chronic infection are associated with an increased risk of cerebral infarction (OR = 2.66, 95% CI: 2.17-3.26), but no such relationship was found with CagA-negative strains (OR = 0.74, 95% CI: 0.49-1.10) in the overall population. We performed subgroup analyses, dividing the overall population into European Caucasians and Chinese Han subgroups, and analyzed the studies according to their subgroup classification. Through the subgroup analysis, an association between cerebral infarction and CagA-bearing strains was found in both subgroups (OR = 2.60, 95% CI: 1.93-3.49 in Chinese Han; OR = 2.71, 95% CI: 2.05-3.59 in European Caucasians), but no significant association was found between cerebral infarction and CagA-negative strains (OR = 0.81, 95% CI: 0.45-1.48 in Chinese Han; OR = 0.64, 95% CI: 0.37-1.09 in European Caucasians).
CONCLUSION: These results suggest CagA-bearing strains of H pylori are significantly associated with susceptibility to cerebral infarction in Chinese Han and European Caucasians, but that CagA-negative strains are not a definite predisposing factor in either subgroup. The magnitude of this association with cerebral infarction needs to be confirmed by prospective studies and combined studies of H pylori eradication.
-
Citation: Zhang S, Guo Y, Ma Y, Teng Y. Relationship between the cytotoxin-associated gene-A status of
H pylori strains and cerebral infarction in European Caucasians and Chinese Han: A meta-analysis. World J Gastroenterol 2008; 14(8): 1286-1292 - URL: https://www.wjgnet.com/1007-9327/full/v14/i8/1286.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.1286
There is increasing evidence, from both clinical and experimental observations, that chronic inflammation (including that caused by Chlamydia pneumoniae, Cytomegalovirus and H pylori) plays an important role in the development of atherosclerotic lesions in patients with coronary artery disease and ischemic stroke. The role of chronic inflammation in atherogenesis has been studied extensively over the past decade. Conceiving atherosclerosis as an inflammatory condition has given rise to a series of hypotheses aimed at finding determinants for the occurrence of cardiovascular and cerebrovascular diseases beyond the traditional risk factors[1]. Among these hypotheses, the contributions of chronic infections to the development of atherothrombosis have been investigated in many cross-sectional and prospective studies, and are currently regarded as co-operating factors in maintaining a chronic inflammatory status[2]. Clinical trials have also addressed the question of a possible positive impact of antibiotic therapy on the clinical burden from cardiovascular disease[3]. H pylori is the most common gastrointestinal agent worldwide. H pylori infection has been linked to other non-classical markers of atherosclerotic diseases, such as heat shock proteins[4], and the relationships between infection and these markers have been largely unexplored.
There is now clear evidence that cytotoxic strains of H pylori bearing the cytotoxin-associated gene A (CagA) have greater potential for eliciting systemic immune responses. Several subsequent case-control and cohort studies have assessed the association between CagA status and atherosclerotic diseases. Patients with atherothrombotic disease seem more likely to be infected by CagA-bearing strains of H pylori than healthy subjects[5]. As a consequence, these studies have assessed a wide variety of H pylori CagA-bearing strains, with inconsistent results worldwide, possibly because of the lack of adequate statistical power, selection bias or population diversity. A meta-analysis may avoid some of these methodological difficulties. In this article, we have performed for the first time a meta-analysis of population-based studies, and examined the evidence on the relationship between CagA status of H pylori strains and the risk of cerebral infarction (not including cerebral embolism) in European Caucasian and Chinese Han populations.
The aims of the present meta-analysis were: (1) To examine if there is an association between cerebral infarction and more virulent, CagA-bearing strains H pylori; (2) to confirm if there is an association between cerebral infarction and CagA-negative strains of H pylori; and (3) to confirm if there exists a difference between European Caucasians and Chinese Han.
The present meta-analysis follows the MOOSE statement guidelines[6]. We performed an electronic search of the MEDLINE (1966 to May 2007), Cochrane library (issue 2, 2007) EMBASE (1966 to May 2007), CBMdisc (Chinese Biomedical Literature analysis and retrieval system for compact disc, 1978 to May 2007) and CNKI (China National Knowledge Infrastructure, 1994 to May 2007) databases. In order to reduce publication bias, we collected data by contacting investigators to request unpublished data. Although it was virtually impossible to obtain all unpublished data, we conducted a manual search from the references of the papers retrieved, important academic conference articles and important Masters and Doctoral dissertations. We searched for the following key words from the MeSH index: “Helicobacter Pylori”, “cytotoxin-associated gene-A”, “atherosclerosis”, “cerebral infarction”, “cerebral ischemia”, “stroke”, “vascular”, “ischemic cerebrovascular disease” and “atherosclerotic cerebral infarction”. The languages were restricted to Chinese and English.
We restricted our review to case-control studies and prospective studies on CagA-bearing strains of H pylori and the risk of cerebral infarction; the individuals in case and control groups were all European Caucasians or Chinese Han. We excluded abstracts, review articles, editorials, commentaries and book chapters. Thus, inclusion criteria for the studies were: (1) The demographic characteristics of cases and controls are similar; (2) a confirmed diagnosis of cerebral infarction, and the diagnosis was valid and specified (that is, CT or MRI scan, or a diagnosis of carotid atherosclerosis according to transcranial Doppler ultrasound); (3) cases and controls are similar in terms of all important features except for the disease in question, or they are matched, or adjustment is performed in the calculation of odds ratios; (4) information about exposure was gathered in the same way from cases and controls; (5) validated testing tool(s) for detecting the CagA status of H pylori and H pylori strains were used; and (6) detection of CagA status was performed blindly.
Studies were excluded when raw data had been duplicately published or the principal investigator was not contacted and couldn’t provide the raw data. All identified publications were independently evaluated and selected by two investigators (Zhang S. and Guo Y.) based on their compliance with these criteria. The results were compared and disagreements were resolved by consensus.
The aim of this meta-analysis was to assess the relationship between the CagA-bearing strains of H pylori and cerebral infarction. To have an internal control, valid in all studies, for this association, valid in all studies, we also assessed the relationship between CagA-negative strains of H pylori and cerebral infarction. Because there are no specific tests for detecting CagA-negative strains, for the purposes of the present analysis, we calculated the prevalence of CagA-negative strains of H pylori by subtracting the number of CagA-seropositive subjects from the total number of individuals with H pylori infection reported in each study.
Data analysis was performed using Review Manager 4.2.10 software (available from the Cochrane Collaboration at http://www.cochrane.org, accessed on June 12, 2007). The studies were pooled by averaging the ORs and 95% CIs with 2-tailed P values through a fixed-effects model, using the Mantel-Haenszel approach when no heterogeneity was observed among studies. When evidence of heterogeneity among studies was detected, a random-effects model was adopted for a combination of all studies. Heterogeneity among studies was tested by the Chi-square statistic, obtained by summing up the weighted squares of the deviations of each estimate from the pooled estimate (P < 0.05 was considered evidence of heterogeneity).
Lack of adjustment for potential confounders and classic cardiovascular risk factors may inflate estimates of any association of novel candidate risk factors with atherosclerotic cerebral infarction. We performed a sensitivity analysis, with the same statistical methods used for the main analysis, excluding studies that did not provide an adjusted odds ratio.
Publication bias was examined by plotting a funnel plot of the reported effect and fail-safe number (Nfs) methods[7]. We plotted the studies’ log odds ratio versus the sample sizes to detect asymmetry in the distribution of trials. A gap in the funnel plot indicates potential for publication bias.
We found a total of 10 retrospective case-control studies on CagA-bearing strains of H pylori and cerebral infarction that were eligible for inclusion; these included 6 studies[8–13] of Chinese Han and 4 studies[14–17] of European Caucasians. We performed a meta-analysis of these studies, dividing the overall population into Chinese Han and European Caucasian subgroups, yielding a total of 907 “cases” and 966 “controls”. The study parameters are summarized in Table 1.
| Author | CagA-bearing strains | CagA-negative strains | Detection method | Race | Multivariate adjustment | Publication year | ||
| In case | In control | In case | In control | |||||
| Li[9] | 38/83 | 14/71 | 34/83 | 26/71 | ELISA | Chinese Han | Age, sex, main risk factors1, cardiogenic factors, occupation | 2001 |
| Wang[8] | 28/79 | 11/73 | 32/79 | 28/73 | ELISA | Chinese Han | Age, sex, main risk factors1, cardiogenic factors, hypercoagulable states | 2004 |
| Liu[10] | 21/50 | 19/50 | 15/50 | 18/50 | ELISA | Chinese Han | Age, sex, main risk factors1, occupation | 2003 |
| Sun[12] | 47/102 | 13/72 | 43/102 | 18/72 | ELISA | Chinese Han | Age, sex, main risk factors1, cardiogenic factors, family history, education | 2006 |
| Wu[13] | 41/78 | 21/60 | 19/78 | 25/60 | ELISA | Chinese Han | Age, sex, main risk factors1, drinking | 2003 |
| Wang[11] | 62/100 | 19/50 | 9/100 | 15/50 | ELISA | Chinese Han | Age, sex, main risk | 2006 |
| Preusch[14] | 34/92 | 45/229 | 34/92 | 82/229 | ELISA | German Caucasian | Age, sex, main risk factors, occupation, family and past history, cardiogenic factors, social class | 2004 |
| Gabrielli[15] | 44/105 | 30/130 | 31/105 | 51/130 | ELISA | Italian Caucasian | Age, sex, main risk factors1, BMI, family history, occupation, peptic ulcer, | 2004 |
| Pietroiusti[16] | 59/138 | 27/151 | 36/138 | 79/151 | ELISA | Italian Caucasian | Age, sex, main risk factors1, BMI, social class, peptic diseases, occupation | 2002 |
| Majka[17] | 46/80 | 27/80 | 23/80 | 27/80 | ELISA | Polish Caucasian | Age, sex, diabetes, hypertension, social class | 2002 |
All of the included studies adjusted data for important confounding factors, the important confounding factors (for example, age, gender, diabetes, hypertension, smoking, social class, BMI, hyperlipidemia, peptic diseases and other pathogenic micro-organism infection) between groups were comparable, and 6 studies[8111214–16] performed multivariate analysis. All studies used enzyme-linked immunosorbent assay (ELISA) to detect seropositivity for the CagA antigen.
The results of tests for heterogeneity in the overall population and its subgroups revealed homogeneity in these studies (P = 0.29 in Chinese Han; P = 0.77 in European Caucasian and P = 0.61 in overall population); therefore, we adopted a fixed effect model to perform combined analysis. The results of combined analysis were statistically significant (OR = 2.60, 95% CI: 1.93-3.49, P < 0.00001 in Chinese Han; OR = 2.71, 95% CI: 2.05-3.59, P < 0.00001 in European Caucasians; OR = 2.66, 95% CI: 2.17-3.26, P < 0.00001 in the overall population), suggesting CagA-bearing strains may be a determinate predisposing factor for the risk of cerebral infarction in the overall population. Moreover, it is also suggested there is no significant difference between Chinese Han and European Caucasians. The results of meta-analysis are shown in Figure 1.
The test for heterogeneity suggested there was significant in these studies (P = 0.001 in Chinese Han; P = 0.009 in European Caucasian and P < 0.0001 in overall population). We performed combined analysis with a random effect model, yielding ORs of 0.81 (95% CI: 0.45-1.48, P = 0.50) in Chinese Han; 0.64 (95% CI: 0.37-1.09, P = 0.10) in European Caucasians and 0.74 (95% CI: 0.49-1.10, P = 0.14) in the overall population, indicating there was no apparent association between CagA-negative strains of H pylori and cerebral infarction. The results were similar in both the Chinese Han and European Caucasian cohorts. The results of meta-analysis are shown in Figure 2.
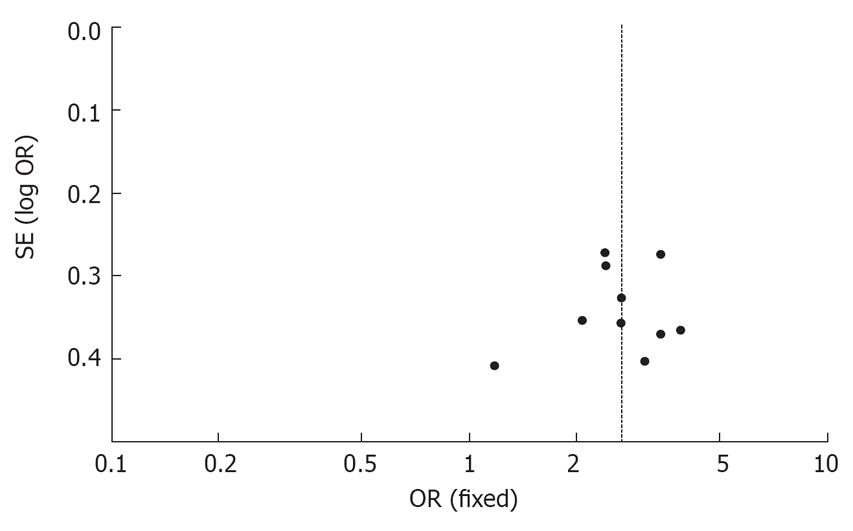
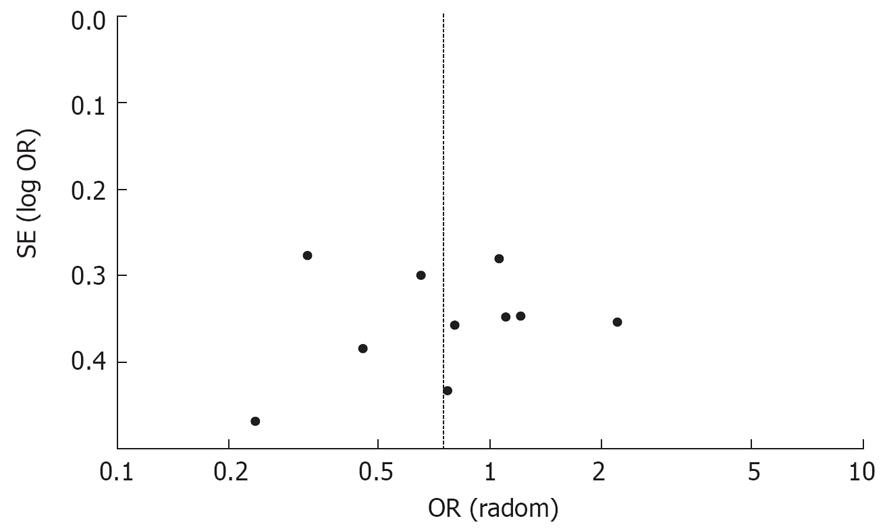
The publication bias of the meta-analysis on the relationship between the CagA status of H pylori strains and cerebral infarction was detected by the Funnel Plot and fail-safe number methods. Although no major asymmetries were detectable in the plot (see Figures 3 and 4), the small number of studies retrieved did not allow publication bias to be excluded. Applying fail-safe number methods (with P = 0.05 and P = 0.01) to evaluate publication bias suggested there was no potential for lack of published data for the negative outcomes. (Nfs0.05 = 81.70, Nfs0.01 = 37.45 in Chinese Han; Nfs0.05 = 169.96, Nfs0.01 = 82.18 in European Caucasians and Nfs0.05 = 498.68, Nfs0.01 = 242.01 in the overall population).
All of the studies retrieved considered important and potential confounders and classical cardiovascular disease risk factors. However, there were four studies, three[91013] in the Chinese Han subgroup and one[17] in the European Caucasian subgroup that did not provide adjusted odds ratios for the relationship between cerebral infarction and CagA-bearing strains. The sensitivity analysis performed after excluding studies without adjusted odds ratios gave a pooled odds ratio of 2.89 (95% CI: 2.25, 3.71, P < 0.0001) in the overall population. These results were similar to the results of the meta-analysis before the sensitivity analysis, suggesting the combined results of meta-analysis were reliable.
Infection by H pylori is one of the most common chronic infections, occurring in approximately half of the world’s population. It commonly affects the gastric mucosa[1819]. Recent studies have found evidence that has resulted in H pylori strains being approximately classified into three types; typeI includes highly virulent strains expressing CagA toxin and VacA toxin, which is strongly related to CagA. Recent studies have found evidence of H pylori, especially CagA-bearing strains, in atherosclerotic plaques[2021] and an association with atherosclerotic diseases.
Using meta-analysis, we found a significant association between cerebral infarction, particularly that caused by atherothrombosis of large vessels, and CagA-bearing strains of H pylori, but not CagA-negative strains. In addition, no difference was found between Chinese Han and European Caucasian populations. By applying sensitivity analysis, we excluded articles that did not provide an adjusted odds ratio, and no difference was found in the conclusion. This indicated the conclusion was reliable and credible. Conducting chronic infected by CagA seronegative strain as the risk factor to combine analysis, we found no statistical significance between CagA-negative strains of H pylori and cerebral infarction in both subgroups and the overall population. Thus, it was uncertain whether CagA-negative strains of H pylori increase the risk of cerebral infarction.
Several mechanistic models may be invoked to explain the association we identified in our meta-analysis. First, it is well known CagA-bearing strains are able to induce enhanced inflammation in the gastric mucosa[22]. Since inflammation plays a major role in atherosclerosis and complicated lesions are associated with an increased inflammatory response[23], the strong inflammatory response related to infection by CagA-bearing strains may influence process of atherosclerosis through an immune-mediated release of cytokines and other substances endowed with pro-inflammatory properties[1617]. Second, it has been suggested H pylori, as well as Chlamydia pneumoniae, could directly provoke inflammation within atherosclerotic plaques. H pylori DNA has been found in carotid atherosclerotic lesions and is associated with features of inflammatory responses[20]. Third, an auto-immune reaction could be postulated. Cross-reactivity between anti-CagA antibodies and vascular wall antigens has been recently demonstrated, suggesting these antibodies may contribute to the activation of inflammatory cells within atherosclerotic lesions[24]. This activation might eventually lead to plaque destabilization.
Although the results of the meta-analysis were positive, it is important to note there were no prospective studies on CagA status and risk of ischemic cerebral diseases. The prospective data available on the topic come from four studies that gave contrasting results on the association between H pylori infection and stroke[25–28]. Regrettably, these studies were heterogeneous in design and provided no raw data to calculate a pooled odds ratio. Only one of these studies[25] reported a large prospective study that compared CagA-seropositive and H pylori-seronegative subjects with regard to the relationship between CagA status and progression of carotid atherosclerosis, during a 5-year follow-up; and the authors showed that infection by CagA-bearing strains of Helicobacter is associated with a larger increase in carotid intimal-medial thickness (IMT) and concluded that infection with CagA-bearing strains could contribute to the pathogenesis of early atherosclerosis. However, no data are available for clinical end points. One study[28] also found that CagA-positive atherosclerotic stroke patients had poorer initial outcomes based on serial measurements of NIHSS scores. No significant differences in IMTs and NIHSS scores were found between H pylori-positive and H pylori-negative patients. Ischemic cerebrovascular diseases, especially cerebral infarction, is likely to be multifactorial[29], involving both polygenic and environmental influences. This article has provided evidence of an association between CagA status and the risk of cerebral infarction in Chinese Han and European Caucasians. It is important to bear in mind the observation nature of meta-analysis, so the standard of quality control could not be completely identical[30]. However, the majority of studies included performed multivariate adjustment in order to minimize bias. Moreover, the sensitive analysis, funnel plot and fail-safe number analysis performed in this article could avoid and evaluate the bias to some extent. More efforts are still needed to perform an accumulated meta-analysis by conducting a high-quality prospective study with expanded sample size, so as to lay a solid foundation for further combined research. Prospective evidence will also clarify the impact of H pylori eradication on the risk of cerebral infarction, and may clarify the relationship between them.
Accumulated evidence indicates a variety of infections contribute to the pathogenesis of atherosclerosis and cerebral infarction, but conflicting results have emerged from the literature. To assess the association between the cytotoxin-associated gene-A (CagA) status of H pylori strains and the risk of cerebral infarction, we carried out a meta-analysis of all related studies.
There have been many clinical and experimental observations highlighting the important role of chronic CagA-bearing strains of H pylori in the development of cerebral infarction. Our study provides evidence for the possible involvement of CagA-bearing strains in cerebral infarction by enhancing some risk factors of atherogenesis. Moreover, the investigation into two genetically distinct populations is of interest.
The most interesting result of this study is we have performed a systematic meta-analysis of population-based studies investigating CagA-bearing and CagA-negative strains of H pylori and their association with the risk of cerebral infarction. The association between H pylori and acute cerebrovascular disease seems to be due to a higher prevalence of more virulent H pylori strains in patients with atherosclerotic stroke.
The meta-analysis suggests H pylori is associated with other markers of atherosclerosis ischemic stroke. The presence of CagA-bearing strains of H pylori causing chronic inflammation is a statistically significant risk factor for cerebral infarction. this article is valuable for the prevention and prediction of cerebral infarction in high-risk populations.
Meta-analysis is a statistical tool for combining results across studies; it is becoming popular as a method for resolving discrepancies in association studies of risk factors.
This is a well-conducted meta-analysis.
| 1. | Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999;340:115-126. |
| 2. | Lindsberg PJ, Grau AJ. Inflammation and infections as risk factors for ischemic stroke. Stroke. 2003;34:2518-2532. |
| 3. | Stone AF, Mendall MA, Kaski JC, Edger TM, Risley P, Poloniecki J, Camm AJ, Northfield TC. Effect of treatment for Chlamydia pneumoniae and Helicobacter pylori on markers of inflammation and cardiac events in patients with acute coronary syndromes: South Thames Trial of Antibiotics in Myocardial Infarction and Unstable Angina (STAMINA). Circulation. 2002;106:1219-1223. |
| 4. | Kalabay L, Fekete B, Czirják L, Horváth L, Daha MR, Veres A, Fónyad G, Horváth A, Viczián A, Singh M. Helicobacter pylori infection in connective tissue disorders is associated with high levels of antibodies to mycobacterial hsp65 but not to human hsp60. Helicobacter. 2002;7:250-256. |
| 5. | Pasceri V, Patti G, Cammarota G, Pristipino C, Richichi G, Di Sciascio G. Virulent strains of Helicobacter pylori and vascular diseases: a meta-analysis. Am Heart J. 2006;151:1215-1222. |
| 6. | Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008-2012. |
| 7. | Mai JZ, Li H, Fang JQ, Liu XQ, Rao XX. Estimation of Fail-Safe Number in Meta-Analysis. Xunzheng Yixue. 2006;6:297-303. |
| 8. | Wang YM, Bai CQ. Preliminary exploration of the association between chronic Helicobacter pylori infection and ischemic stroke. Shaxi Yixue Zazhi. 2004;33:791-781. |
| 9. | Li YJ, Mao XL, Zhu YQ. Relationship between Helicobacter pylori bearing the cytotoxin-associated gene- A and cerebra l infarction. Naoyu Shenjingjibing Zahi. 2001;9:9-10. |
| 10. | Liu XR, Duan HL, Zhou B, Wang YL, Huang YB, Cui Y, Liu HF. Association between Infection with Helicobacter pylori and risk of cerebral infarction. Zhongguo Zonghe Linchuang. 2003;19:614-616. |
| 11. | Wang Y. Relationship between helicobacter pylori cytotoxin-associated protein A and atherosclerotic cerebral infarction. Linchuang Shenjingbingxue Zazhi. 2006;4:272-274. |
| 12. | Sun YY, Wang YJ, Kang XX. The study of the relationship between helicobacter pylori infection and cerebral ischemia. Zhongguo Shiyan Zhenduanxue. 2006;8:826-828. |
| 13. | Wu XX, Huang ZY, Huang DH. Study on the relationship between helicobacter pylori infection and cerebral infarction. Zhongguo Jiceng Yiyao. 2003;7:599-600. |
| 14. | Preusch MR, Grau AJ, Buggle F, Lichy C, Bartel J, Black C, Rudi J. Association between cerebral ischemia and cytotoxin-associated gene-A-bearing strains of Helicobacter pylori. Stroke. 2004;35:1800-1804. |
| 15. | Gabrielli M, Santoliquido A, Cremonini F, Cicconi V, Candelli M, Serricchio M, Tondi P, Pola R, Gasbarrini G, Pola P. CagA-positive cytotoxic H. pylori strains as a link between plaque instability and atherosclerotic stroke. Eur Heart J. 2004;25:64-68. |
| 16. | Pietroiusti A, Diomedi M, Silvestrini M, Cupini LM, Luzzi I, Gomez-Miguel MJ, Bergamaschi A, Magrini A, Carrabs T, Vellini M. Cytotoxin-associated gene-A--positive Helicobacter pylori strains are associated with atherosclerotic stroke. Circulation. 2002;106:580-584. |
| 17. | Majka J, Rog T, Konturek PC, Konturek SJ, Bielanski W, Kowalsky M, Szczudlik A. Influence of chronic Helicobacter pylori infection on ischemic cerebral stroke risk factors. Med Sci Monit. 2002;8:CR675-CR684. |
| 18. | Xue FB, Xu YY, Wan Y, Pan BR, Ren J, Fan DM. Association of H. pylori infection with gastric carcinoma: a Meta analysis. World J Gastroenterol. 2001;7:801-804. |
| 19. | Plummer M, van Doorn LJ, Franceschi S, Kleter B, Canzian F, Vivas J, Lopez G, Colin D, Munoz N, Kato I. Helicobacter pylori cytotoxin-associated genotype and gastric precancerous lesions. J Natl Cancer Inst. 2007;99:1328-1334. |
| 20. | Ameriso SF, Fridman EA, Leiguarda RC, Sevlever GE. Detection of Helicobacter pylori in human carotid atherosclerotic plaques. Stroke. 2001;32:385-391. |
| 21. | Ghirardi G, Maldonado F, Guzman L, Juaneda J, Zuniga ME. Helicobacter pylori detected in atheroma plaque. Rev Fac Cien Med Univ Nac Cordoba. 2006;63:17-23. |
| 22. | Mach F, Sukhova GK, Michetti M, Libby P, Michetti P. Influence of Helicobacter pylori infection during atherogenesis in vivo in mice. Circ Res. 2002;90:E1-E4. |
| 23. | de Boer OJ, van der Wal AC, Becker AE. Atherosclerosis, inflammation, and infection. J Pathol. 2000;190:237-243. |
| 24. | Franceschi F, Sepulveda AR, Gasbarrini A, Pola P, Silveri NG, Gasbarrini G, Graham DY, Genta RM. Cross-reactivity of anti-CagA antibodies with vascular wall antigens: possible pathogenic link between Helicobacter pylori infection and atherosclerosis. Circulation. 2002;106:430-434. |
| 25. | Mayr M, Kiechl S, Mendall MA, Willeit J, Wick G, Xu Q. Increased risk of atherosclerosis is confined to CagA-positive Helicobacter pylori strains: prospective results from the Bruneck study. Stroke. 2003;34:610-615. |
| 26. | Smieja M, Gnarpe J, Lonn E, Gnarpe H, Olsson G, Yi Q, Dzavik V, McQueen M, Yusuf S. Multiple infections and subsequent cardiovascular events in the Heart Outcomes Prevention Evaluation (HOPE) Study. Circulation. 2003;107:251-257. |
| 27. | Haider AW, Wilson PW, Larson MG, Evans JC, Michelson EL, Wolf PA, O'Donnell CJ, Levy D. The association of seropositivity to Helicobacter pylori, Chlamydia pneumoniae, and cytomegalovirus with risk of cardiovascular disease: a prospective study. J Am Coll Cardiol. 2002;40:1408-1413. |
| 28. | Diomedi M, Pietroiusti A, Silvestrini M, Rizzato B, Cupini LM, Ferrante F, Magrini A, Bergamaschi A, Galante A, Bernardi G. CagA-positive Helicobacter pylori strains may influence the natural history of atherosclerotic stroke. Neurology. 2004;63:800-804. |
| 29. | Zhang Y, Qin Z. The restriction fragment length polymorphism (Xba I, EcoR I) of apolipoprotein B gene in relation to the atherothrombotic cerebral infarction. Linchuang Shenjingbingxue Zazhi. 1998;11:3-6. |
| 30. | Kaizar EE. Metaanalyses are observational studies: how lack of randomization impacts analysis. Am J Gastroenterol. 2005;100:1233-1236. |