Published online Nov 28, 2008. doi: 10.3748/wjg.14.6867
Revised: November 12, 2008
Accepted: November 19, 2008
Published online: November 28, 2008
Percutaneous aspiration and drainage of post-operative abdominal fluid collections is a well established standard technique. However, some fluid collections are not amenable to percutaneous drainage either due to location or the presence of surrounding visceral structures. Endoscopic Ultrasound (EUS) has been widely used for the drainage of pancreatitis-related abdominal fluid collections. However, there are no reports on the use of this technique in the post-operative setting. We report a case where the EUS-guided technique was used to drain a percutaneously inaccessible post-operative collection which had developed after Whipple’s resection.
- Citation: Jah A, Jamieson N, Huguet E, Griffiths W, Carroll N, Praseedom R. Endoscopic Ultrasound-guided drainage of an abdominal fluid collection following Whipple’s resection. World J Gastroenterol 2008; 14(44): 6867-6868
- URL: https://www.wjgnet.com/1007-9327/full/v14/i44/6867.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6867
Drainage of post-operative abdominal fluid collections is generally carried out percutaneously under radiological guidance. However, some of these collections may be inaccessible to percutaneous drainage because of their location and surrounding vital structures.
We report a case where a post-operative fluid collection which developed after a Whipple’s resection was successfully drained endoscopically under endoscopic ultrasound (EUS) guidance. Although widely used in pancreatitis, this is the first report of the use of this technique in a post-operative setting.
A 45 year old lady underwent Whipple’s resection for cholangiocarcinoma of the distal common bile duct. Pancreatico-jejunostomy and hepatico-jejunostomy were performed on to a 70 cm Roux-en-Y jejunal loop and a gastrojejunostomy was fashioned using the end of the main jejunal segment continuous with the rest of the intestine.
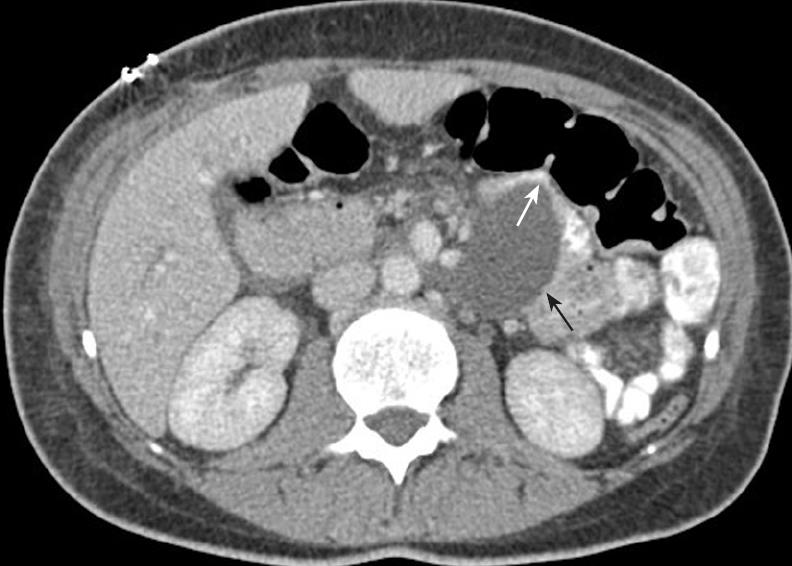
Her initial recovery was uneventful but on the 9th post-operative day she developed pyrexia and vomiting suggestive of gastric outlet obstruction. A contrast-enhanced computerized tomogram (CT) showed a deep-seated fluid collection measuring 5.1 × 3.3 cm which was compressing and stretching the efferent jejunal loop distal to the gastrojejunostomy (Figure 1). Percutaneous drainage was deemed unsafe due to the surrounding bowel loops and blood vessels. However, its proximity to the gastrojejunostomy made it accessible endoscopically.
An EUS-endoscope (GF-UCT240, Olympus, UK) was passed through the gastrojejunostomy and the sero-sanguinous collection was aspirated to dryness under EUS guidance using a 19-gauge Echotip-Ultra needle (Wilson-Cook, Ireland) (Figure 2). The amylase level in the aspirate was normal and all the cultures were sterile. Following aspiration of the fluid collection the vomiting and pyrexia settled, and the patient was able to recommence oral intake. There were no complications related to this procedure and she was discharged from hospital after three days. She was asymptomatic at her routine surgical outpatient review 6 wk later.
Abdominal fluid collections are common after Whipple’s resection and are frequently situated in the pancreatic bed. They may be related to an anastomotic leak (generally pancreatic) and often cause mechanical and/or infective complications. These collections are generally deep-seated and are surrounded by major blood vessels. This combined with altered post-surgical anatomy (presence of Roux loops etc) often makes a direct percutaneous route for drainage impossible to find. In this patient, it was important to exclude a pancreatic leak and to resolve the gastric outlet obstruction. In such cases, a laparotomy would normally be necessary in the absence of a safe percutaneous option.
In contrast, endoscopic transmural drainage or aspiration with EUS guidance has greatly reduced the need for surgery in pancreatitis-related fluid collections and has now become a standard procedure for this condition in our unit. The safety of this technique and high success rates have been widely reported[1-3]. This experience prompted us to use the EUS-guided technique as an alternative route for drainage of this post-operative fluid collection where percutaneous approach was deemed unsafe.
In a patient with a visceral fluid collection, the feasibility of EUS-guided drainage should first be assessed with dual contrast-enhanced CT. Close proximity to the stomach or jejunum provides an easy endoscopic access to these collections. The technique of EUS-guided aspiration is well established[1-3].
We anticipate that the main role of EUS-guided aspiration of collections in the post-operative situation would be to allow much-needed sampling of fluid for microbiological and biochemical analysis. In patients with sepsis or mechanical complications such as obstruction secondary to collections, this technique would also be therapeutic. In stable patients this could eliminate the need for a laparotomy which would otherwise carry a much higher risk of morbidity and mortality. Thus, we conclude that EUS-guided aspiration/drainage should be considered in patients with otherwise inaccessible post-operative fluid collections.
| 1. | Baron TH. Endoscopic drainage of pancreatic fluid collections and pancreatic necrosis. Gastrointest Endosc Clin N Am. 2003;13:743-764. |
| 2. | Hookey LC, Debroux S, Delhaye M, Arvanitakis M, Le Moine O, Devière J. Endoscopic drainage of pancreatic-fluid collections in 116 patients: a comparison of etiologies, drainage techniques, and outcomes. Gastrointest Endosc. 2006;63:635-643. |
| 3. | Lopes CV, Pesenti C, Bories E, Caillol F, Giovannini M. Endoscopic-ultrasound-guided endoscopic transmural drainage of pancreatic pseudocysts and abscesses. Scand J Gastroenterol. 2007;42:524-529. |
Peer reviewer: Dr. Massimo Raimondo, Division of Gastroenterology and Hepatology, Mayo Clinic, 4500 San Pablo Road, Jacksonville, FL 32224, United States
S- Editor Tian L L- Editor Webster JR E- Editor Yin DH