Published online Oct 28, 2008. doi: 10.3748/wjg.14.6208
Revised: July 26, 2008
Accepted: August 3, 2008
Published online: October 28, 2008
AIM: To investigate if sildenafil increases splanchnic blood flow and changes the hepatic venous pressure gradient (HVPG) in patients with cirrhosis. Phosphodiesterase type-5 inhibitors are valuable in the treatment of erectile dysfunction and pulmonary hypertension in patients with end-stage liver disease. However, the effect of phosphodiesterase type-5 inhibitors on splanchnic blood flow and portal hypertension remains essentially unknown.
METHODS: Ten patients with biopsy proven cirrhosis (five females/five males, mean age 54 ± 8 years) and an HVPG above 12 mmHg were studied after informed consent. Measurement of splanchnic blood flow and the HVPG during liver vein catheterization were done before and 80 min after oral administration of 50 mg sildenafil. Blood flow was estimated by use of indocyanine green clearance technique and Fick's principle, with correction for non-steady state.
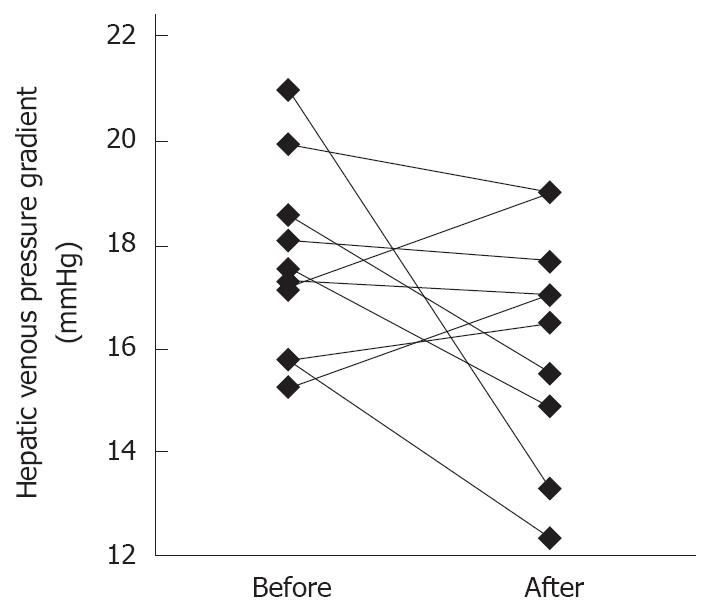
RESULTS: The plasma concentration of sildenafil was 222 ± 136 ng/mL 80 min after administration. Mean arterial blood pressure decreased from 77 ± 7 mmHg to 66 ± 12 mmHg, P = 0.003, while the splanchnic blood flow and oxygen consumption remained unchanged at 1.14 ± 0.71 L/min and 2.3 ± 0.6 mmol/min, respectively. Also the HVPG remained unchanged (18 ± 2 mmHg vs 16 ± 2 mmHg) with individual changes ranging from -8 mmHg to +2 mmHg. In seven patients, HVPG decreased and in three it increased.
CONCLUSION: In spite of arterial blood pressure decreases 80 min after administration of the phosphodiesterase type-5 inhibitor sildenafil, the present study could not demonstrate any clinical relevant influence on splanchnic blood flow, oxygen consumption or the HVPG.
- Citation: Clemmesen JO, Giraldi A, Ott P, Dalhoff K, Hansen BA, Larsen FS. Sildenafil does not influence hepatic venous pressure gradient in patients with cirrhosis. World J Gastroenterol 2008; 14(40): 6208-6212
- URL: https://www.wjgnet.com/1007-9327/full/v14/i40/6208.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6208
| Characteristics | Data |
| Age (yr) | 54 ± 8 |
| Weight (kg) | 75 ± 16 |
| Height (cm) | 175 ± 7 |
| Female/Male | 5/5 |
| Aetiology (ALC/AIH/PBC) | 8/1/1 |
| Varices, present | 9 |
| Bleeding, earlier | 5 |
| Ascites, present | 8 |
| Child Pugh (A/B/C) | 1/2/7 |
| GEC (µmol/kg per min) | 20 ± 4 |
| INR | 1.7 ± 0.5 |
| Bilirubin (mmol/L) | 64 ± 50 |
| Albumin (g/L) | 24 ± 5 |
| Baseline | 80 min after | |
| MAP (mmHg) | 77 ± 7 | 66 ± 121 |
| HF (beats/min) | 83 ± 13 | 85 ± 11 |
| RA (mmHg) | 5 ± 1 | 6 ± 2 |
| Hepatic blood flow (L/min) | 1.14 ± 0.71 | 1.14 ± 0.94 |
| VO2 (mmol/min) | 2.3 ± 0.6 | 2.5 ± 1.2 |
| Wedged pressure (mmHg) | 29 ± 6 | 27 ± 6 |
| Free pressure (mmHg) | 12 ± 6 | 11 ± 5 |
| Gradient (mmHg) | 18 ± 2 | 16 ± 2 |
Erectile dysfunction is a common problem affecting about half of all patients with end-stage liver disease[1,2]. The systematic use of beta-adrenergic blockade[3,4], initiated in order to reduce the hepatic venous pressure gradient (HVPG), may also per se induce impotence[5]. Selective phosphodiesterase type-5 inhibitors, such as sildenafil, represent an important advance in management of erectile dysfunction[6,7]. Inhibition of phosphodiesterase type-5, the prominent isoform in corpora cavernosa, leads to diminished degradation of cyclic guanosine monophosphate, relaxation of smooth muscle and blood filling of corpora cavernosa[8].
In rats, phosphodiesterase type-5 is also present in the superior mesenteric artery[9]. Administration of sildenafil results in a dose-dependent increase in mesenteric blood flow and a minor increase in portal venous pressure, in both the bile-duct-ligated rat, as well as in control rats[10]. It has been suggested that phosphodiesterase type-5 is also present in human mesenteric arteries[11]. The use of sildenafil could, therefore, be hazardous in patients with cirrhosis and portal hypertension. Indeed, acute variceal bleeding has been described after intake of 25 mg sildenafil[12,13]. On the other hand, a more recent study in patients with Child A liver cirrhosis has shown a decrease in portal and sinusoidal resistance after inhibition of phosphodiesterase-5[14], which was introduced as a new potential treatment modality of portal hypertension[14].
Since sildenafil seems to be valuable in the treatment erectile dysfunction[14] and portopulmonary hypertension[15] in patients with cirrhosis, the aim of the present study was to determine if splanchnic blood flow and HVPG are influenced by sildenafil in patients with cirrhosis.
Twelve patients with biopsy-proven cirrhosis were included in the study during diagnostic work-up and/or evaluation for liver transplantation. None of the patients were treated with nitrates or beta-adrenergic drugs at the time of the study. Furthermore, only patients with an HVPG above 12 mmHg were considered for inclusion in this study. Two patients were excluded due to this last criterion. Thus, 10 patients participated (five females/five males, mean age 54 ± 8 years). The reason for referral to our tertiary liver failure unit was chronic hepatic insufficiency in five, recurrent bleeding from esophageal varices in four, and therapy-resistant ascites in one patient. None of the patients had suffered from variceal bleeding within 14 d of the study. Participation in the study included measurement of the HVPG and the estimation of splanchnic blood flow before and 80 min after oral administration of 50 mg of sildenafil. All patients were included after written informed consent, and after the local scientific-ethical committee had approved the study.
Hepatic venous catheterization (Cordis, MP-A1, open end catheter, Miami, USA) was performed through the right or left intermedian cubital vein. During the advance of the catheter, blood pressure in the right atrium was registered. After location of a hepatic vein, the catheter was advanced to the wedge position. Pressure was measured via a pressure monitoring set and was continuously recorded (Hewlett Packard, 78354C) and could be printed (Hewlett Packard, M1125A). The pressure transducer was calibrated to zero pressure at the level of the right atrium. The wedge pressure was only accepted if the wedge position afterwards could be confirmed by visualization of a characteristic wedge pattern on the fluoroscope by use of X-ray contrast media (Omnipaque 240 mg/mL, Amersham Health). Free hepatic venous pressure was measured as close as possible to the inferior caval vein. Pressures, free and wedged, were measured in three different hepatic veins and the mean was used. The catheter was then positioned in a hepatic vein half way between wedge position and the caval vein and used for blood sampling.
Splanchnic blood flow was estimated by use of indocyanine green as previously described[16]. In short, indocyanine green was continuously infused and simultaneously, five paired samples of arterial and hepatic venous blood were drawn at intervals of 5 min. Calculation of hepatic blood flow was based on Fick’s principle with correction for non-steady state[16]. Splanchnic oxygen consumption was calculated as the arterio-venous oxygen content difference times splanchnic blood flow.
Patients were given 50 mg sildenafil with 100 mL of tap water. From 60 to 80 min thereafter, blood was again sampled for estimation of hepatic blood flow. HVPG was measured again, as described above, in three different veins. Pressure in the right atrium was recorded during withdrawal of the catheter.
Indocyanine green was determined by use of HPLC as earlier described[17]. To ensure absorption of sildenafil, blood was sampled 80 min after administration and plasma sildenafil concentration was later analyzed using automated sequential trace enrichment of dialyzates and HPLC[18].
Data are shown as mean ± SD. Paired t test was used for comparison, P < 0.05 was considered statistically significant.
Characteristics and clinical data from the 10 participating patients showed that the majority had advanced cirrhosis (Table 1). None of the patients had allergy to sildenafil. The concentration of sildenafil in plasma was 222 ± 136 ng/mL, 80 min after administration of the drug.
There was a statistically significant decrease in mean arterial pressure from 77 ± 7 mmHg to 66 ± 12 mmHg, P = 0.003, after sildenafil administration (Table 2). No statistically significant changes were observed in other hemodynamic variables or in splanchnic oxygen consumption (Table 2). In particular, the HVPG remained statistically unchanged, i.e. 18 ± 2 mmHg before vs 16 ± 2 mmHg, after administration of sildenafil.
The plasma concentration of sildenafil at 80 min was not statistically significantly correlated to the changes in HVPG, splanchnic blood flow, mean arterial pressure, or right atrial pressure.
Four patients had a decrease in HVPG i.e. 3, 3, 3 and, 8 mmHg, respectively. Two of these where Child class A/B and all four had alcoholic cirrhosis.
This study reports the effects of sildenafil on the splanchnic hemodynamics in patients with biopsy proven cirrhosis and manifest portal hypertension. Despite a small decrease in mean arterial pressure, the main finding in this study was that the splanchnic blood flow, oxygen consumption and the mean HVPG did not change 80 min after administration of sildenafil, i.e. at a time-point when a therapeutic plasma concentration of sildenafil[19] could be documented. These data appear to be in accordance with preliminary results testing the effect of an oral dose of 25 mg of sildenafil with which no effect on portal pressure was reported, in spite a decrease in arterial pressure[20]. However, our results appear to be in contrast to an earlier study reported by Deibert et al[14], in which vardenafil (another phosphodiesterase type-5 inhibitor) was found to lower portal pressure in four of five patients with Child A cirrhosis. The reason for this discrepancy is not clear, but three of the five patients in that latter study[14] had HVPG < 12 mmHg before administration of vardenafil.
As illustrated in Figure 1, the individual HVPG changes ranged from -8 to +2 mmHg. In an animal study with bile-duct-ligated rats, a statistically significant increase in the HVPG of 3% ± 1% after intramesenteric (10 mg/kg) administration of sildenafil has been reported[10]. Thus, our finding suggests that the effect of sildenafil on splanchnic hemodynamics in humans with cirrhosis is different from that in rats. This could be due to the uncertainty concerning which phosphodiesterase isoform, PDE5 and/or PDE1 is present in the human mesenteric artery[11]. It can be argued that even a 10%-15% increase in HVPG, as seen in one out of 10 patients in our study, might be problematic in the individual. However, small changes in the gradient probably take place during everyday life. For example, digestion of food increases hepatic blood flow by almost 100%. In particular, a major increase is seen in the superior mesenteric artery and thus portal blood flow[21]. Moreover, it has been demonstrated in patients with cirrhosis that a meal increases the mean HVPG from 16 to 20 mmHg, corresponding to 25%[22]. This could be even higher in the individual. The risk of experiencing a bleeding episode after intake of sildenafil should, therefore, be interpreted in the light of such everyday events.
The splanchnic hemodynamic data were collected during rest in the present study. However, supposedly the user of sildenafil is rarely in a resting position, but is more likely to increase the level of physical activity, which is known to influence the splanchnic hemodynamics[23]. In fact, physical activity, with an exercise level of 30% of peak workload, appears to increase HVPG from 16.7 to 19.2 mmHg[23]. Working at 50% of peak workload will not increase this HVPG gradient any further. Thus, the physical activity, which often is required to engage in sexual activity, may itself slightly increase the gradient. However, and of importance, the opposite has been observed in patients with cirrhosis during exercise and beta-adrenergic blockade[24]. In these patients, exercise at 30% of peak workload was associated with a decrease in HVPG from 16.3 to 12.9 mmHg[19]. This was explained by a lesser increase in cardiac output and a larger decrease in hepatic blood flow in the propranolol group compared to the non-beta-blocker-treated group of patients.
The possible effect on splanchninc hemodynamics after longer use of sildenafil is elusive and has not been examined. One concern about chronic use may be the possible renal effects. In patients with cirrhosis, administration of a single dose of sildenafil was followed by a decrease in sodium excretion[25]. However, the long-term renal effects may be insignificant as chronic administration of sildenafil prevented the decrease in sodium excretion seen in bile-duct-ligated rats[26].
The present study shows that sildenafil does not induce any profound clinically relevant changes in splanchnic blood flow, oxygen consumption and HVPG. This indicates that phosphodiesterase type-5 inhibition is of no use as a therapeutic agent for alleviating portal hypertension in patients with chronic end-stage liver disease. On the other hand, the use of sildenafil in such patients, initiated because of erectile dysfunction, appears to be safe per se. However,, clearly more studies on safety are needed, as the use of sildenafil is usually associated with physical activity and often also the use of beta blockers.
Erectile dysfunction is a common problem affecting about half of all patients with end-stage liver disease. Selective phosphodiesterase type-5 inhibitors, such as sildenafil, represent an important advance in management of erectile dysfunction. In rats, administration of sildenafil results in a dose-dependent increase in mesenteric blood flow and a minor increase in portal venous pressure. The use of sildenafil could, therefore, be hazardous in patients with cirrhosis and portal hypertension and acute variceal bleeding has been described after intake of 25 mg sildenafil.
Bleeding from esophageal varices is a major contributor to death in patients with end-stage liver disease and it could be hazardous to recommend treatment of erectile dysfunction with sildenafil if this treatment, in turn, leads to an increase in hepatic venous pressure gradient (HVPG).
Another human study addressing the presented problem has been published in abstract form, but the patients investigated all had Child class A cirrhosis whereas, erectile dysfunction as a “quality of life problem” tends to increase with increasing severity of liver disease i.e. Child class B and C, and such patients where investigated in the present study.
The present study does not support a restrictive use of sildenafil in patients with cirrhosis. Future research should be done with larger patient groups in order to determine the long-term risk of bleeding (if any) during treatment with sildenafil.
Liver disease leads to accumulation of fibrous tissue in the liver, and in turn, this leads to increased resistance to the blood flow through the portal vein. The resistance is estimated by the HVPG and the risk of bleeding from esophageal varices in cirrhosis increases with this gradient.
This is an interesting and informative study. The authors investigated if sildenafil increases splanchnic blood flow and changes the HVPG in patients with cirrhosis. Phosphodiesterase type-5 inhibitors are valuable in the treatment of erectile dysfunction and pulmonary hypertension in patients with end-stage liver disease.
| 1. | Cornely CM, Schade RR, Van Thiel DH, Gavaler JS. Chronic advanced liver disease and impotence: cause and effect? Hepatology. 1984;4:1227-1230. |
| 2. | Jensen SB, Gluud C. Sexual dysfunction in men with alcoholic liver cirrhosis. A comparative study. Liver. 1985;5:94-100. |
| 3. | Lebrec D, Nouel O, Corbic M, Benhamou JP. Propranolol--a medical treatment for portal hypertension? Lancet. 1980;2:180-182. |
| 4. | Groszmann RJ, Bosch J, Grace ND, Conn HO, Garcia-Tsao G, Navasa M, Alberts J, Rodes J, Fischer R, Bermann M. Hemodynamic events in a prospective randomized trial of propranolol versus placebo in the prevention of a first variceal hemorrhage. Gastroenterology. 1990;99:1401-1407. |
| 5. | Burris JF, Goldstein J, Zager PG, Sutton JM, Sirgo MA, Plachetka JR. Comparative tolerability of labetalol versus propranolol, atenolol, pindolol, metoprolol, and nadolol. J Clin Hypertens. 1986;2:285-293. |
| 6. | Boolell M, Gepi-Attee S, Gingell JC, Allen MJ. Sildenafil, a novel effective oral therapy for male erectile dysfunction. Br J Urol. 1996;78:257-261. |
| 7. | Goldstein I, Lue TF, Padma-Nathan H, Rosen RC, Steers WD, Wicker PA. Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med. 1998;338:1397-1404. |
| 8. | Corbin JD, Francis SH. Cyclic GMP phosphodiesterase-5: target of sildenafil. J Biol Chem. 1999;274:13729-13732. |
| 9. | Sampson LJ, Hinton JM, Garland CJ. Evidence for expression and function of phosphodiesterase type 5 (PDE-V) in rat resistance arteries. Br J Pharmacol. 2001;132:13-17. |
| 10. | Colle I, De Vriese AS, Van Vlierberghe H, Lameire NH, DeVos M. Systemic and splanchnic haemodynamic effects of sildenafil in an in vivo animal model of cirrhosis support for a risk in cirrhotic patients. Liver Int. 2004;24:63-68. |
| 11. | Wallis RM, Corbin JD, Francis SH, Ellis P. Tissue distribution of phosphodiesterase families and the effects of sildenafil on tissue cyclic nucleotides, platelet function, and the contractile responses of trabeculae carneae and aortic rings in vitro. Am J Cardiol. 1999;83:3C-12C. |
| 12. | Tzathas C, Christidou A, Ladas SD. Sildenafil (viagra) is a risk factor for acute variceal bleeding. Am J Gastroenterol. 2002;97:1856. |
| 13. | Finley DS, Lugo B, Ridgway J, Teng W, Imagawa DK. Fatal variceal rupture after sildenafil use: report of a case. Curr Surg. 2005;62:55-56. |
| 14. | Deibert P, Schumacher YO, Ruecker G, Opitz OG, Blum HE, Rossle M, Kreisel W. Effect of vardenafil, an inhibitor of phosphodiesterase-5, on portal haemodynamics in normal and cirrhotic liver -- results of a pilot study. Aliment Pharmacol Ther. 2006;23:121-128. |
| 15. | Callejas Rubio JL, Salmerón Escobar J, González-Calvín J, Ortego Centeno N. Successful treatment of severe portopulmonary hypertension in a patient with Child C cirrhosis by sildenafil. Liver Transpl. 2006;12:690-691. |
| 16. | Skak C, Keiding S. Methodological problems in the use of indocyanine green to estimate hepatic blood flow and ICG clearance in man. Liver. 1987;7:155-162. |
| 17. | Ott P, Keiding S, Bass L. Plasma elimination of indocyanine green in the intact pig after bolus injection and during constant infusion: comparison of spectrophotometry and high-pressure liquid chromatography for concentration analysis. Hepatology. 1993;18:1504-1515. |
| 18. | Cooper JD, Muirhead DC, Taylor JE, Baker PR. Development of an assay for the simultaneous determination of sildenafil (Viagra) and its metabolite (UK-103,320) using automated sequential trace enrichment of dialysates and high-performance liquid chromatography. J Chromatogr B Biomed Sci Appl. 1997;701:87-95. |
| 19. | Muirhead GJ, Wilner K, Colburn W, Haug-Pihale G, Rouviex B. The effects of age and renal and hepatic impairment on the pharmacokinetics of sildenafil. Br J Clin Pharmacol. 2002;53 Suppl 1:21S-30S. |
| 20. | Inayat I, Tandon P, Tal MG, Spector M, Bari K, Groszmann RJ, Garcia-Tsao G. Sildenafil has no effect on portal pressure but lowers arterial pressure. Hepatology. 2007;53 Suppl 1:46; 569A. |
| 21. | Perko MJ, Nielsen HB, Skak C, Clemmesen JO, Schroeder TV, Secher NH. Mesenteric, coeliac and splanchnic blood flow in humans during exercise. J Physiol. 1998;513:907-913. |
| 22. | Bellis L, Berzigotti A, Abraldes JG, Moitinho E, Garcia-Pagan JC, Bosch J, Rodes J. Low doses of isosorbide mononitrate attenuate the postprandial increase in portal pressure in patients with cirrhosis. Hepatology. 2003;37:378-384. |
| 23. | Garcia-Pagan JC, Santos C, Barbera JA, Luca A, Roca J, Rodriguez-Roisin R, Bosch J, Rodes J. Physical exercise increases portal pressure in patients with cirrhosis and portal hypertension. Gastroenterology. 1996;111:1300-1306. |
| 24. | Bandi JC, Garcia-Pagan JC, Escorsell A, Francois E, Moitinho E, Rodes J, Bosch J. Effects of propranolol on the hepatic hemodynamic response to physical exercise in patients with cirrhosis. Hepatology. 1998;28:677-682. |
| 25. | Thiesson HC, Jensen BL, Jespersen B, Schaffalitzky de Muckadell OB, Bistrup C, Walter S, Ottosen PD, Veje A, Skott O. Inhibition of cGMP-specific phosphodiesterase type 5 reduces sodium excretion and arterial blood pressure in patients with NaCl retention and ascites. Am J Physiol Renal Physiol. 2005;288:F1044-F1052. |
| 26. | Ghali-Ghoul R, Tahseldar-Roumieh R, Sabra R. Effect of chronic administration of sildenafil on sodium retention and on the hemodynamic complications associated with liver cirrhosis in the rat. Eur J Pharmacol. 2007;572:49-56. |
Peer reviewer: Philip Abraham, PhD, Professor, Consultant Gastroenterologist & Hepatologist, P. D. Hinduja National Hospital & Medical Research Centre, Veer Savarkar Marg, Mahim, Mumbai 400016, India
S- Editor Li DL L- Editor Rippe RA E- Editor Lin YP