INTRODUCTION
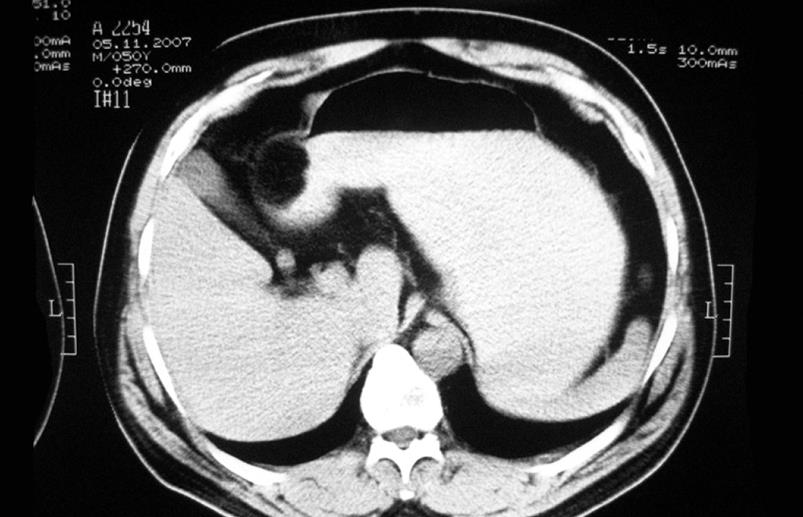
Figure 1 CT scan image showing a well-defined oval mass on the antro-pyloric part of stomach.
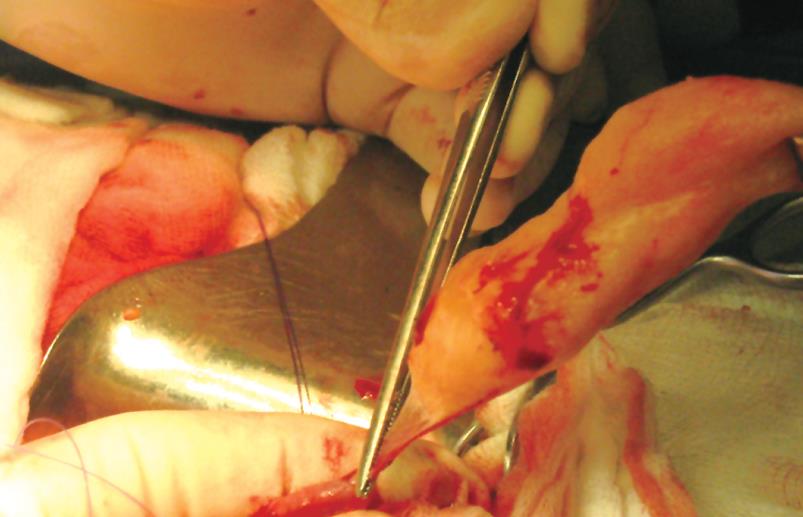
Figure 2 Intraoperative view showing a yellowish subserosal neoplasm on the anterior wall of gastric antrum during extirpation.
Figure 3 Histopathology confirming the diagnosis of lipoma containing mature fat cells with slight variation in size and shape (HE, × 100).
Gastrointestinal lipomas are uncommon, slowly growing benign tumors composed of mature adipose tissue that can occur anywhere along the gut. Mostly are located in the colon, ileum and jejunum[1]. Lipomas found in the stomach are even more unusual, accounting for 2%-3% of all benign gastric tumors[2,3]. They are of submucosal or extremely rare subserosal origin, most frequently localized to the antrum[4-7]. Although it is reported that 5%-10% of gastric lipomas are located at subserosal layer[1], so far, there is no report on treatment of subserosal gastric lipomas in the English medical literature. Karadeniz et al[8] in 2007 described an exceptional case of subserosal lipoma within an inverted Meckel’s diverticulum. In the past, preoperative accurate diagnosis was very difficult even for symptomatic gastric lipomas[9]. The treatment of large symptomatic gastric lipomas has not yet been established[10]. Actual imaging technologies and endoscopy have become new approaches to the management of gastric lipomas[9-12]. We present a case of a large symptomatic subserosal gastric lipoma which was successfully managed with removal, enucleation of lipoma, explorative gastrotomy and edge resection for histology check of gastric wall.
CASE REPORT
A 50 year-old male patient was admitted to the Division of Abdominal Surgery with a 6-mo history of upper abdominal pain, dyspeptic disorders, vomiting mainly after the meal, and tachycardia, without significant weight loss. He was previously medically treated for bronchial asthma and chronic gastritis with pronison, aminophylline, spalmotil, omeprazol, and surgically underwent appendectomy, repair of limb fracture and nose deviation. He stopped smoking twelve years ago.
On admission, physical examination was unremarkable. Abdomen was soft and flat with mild tenderness in epigastrium and no palpable masses. Laboratory examinations including tumor markers, CEA, CA19-9 and AFP, showed no abnormalities. Barium meal study showed a normally shaped stomach without signs of filling defects and motility abnormalities, except for an axial hiatus hernia. Upper gastrointestinal endoscopy which was done two times, revealed a soft submucosal oval-shaped mass with an approximate diameter of 5 cm in gastric antrum. Overlying mucosa had a normal appearance with slight local hyperemia. Multiple gastric mucosa biopsies showed normal epithelium and rare stromal infiltrate with regular mucosa built up by regular tubular glands. Abdominal CT scan showed on the antro-pyloric part of the stomach a homogeneous well-defined oval mass around 6 cm in diameter with negative densitometry values (-50 and -60 Hounsfield units) that corresponds to fatty tissue (Figure 1). The patient underwent midline supraumbilical laparotomy. Intraoperatively, a yellowish, soft surface subserosal, well-defined tumor with a longitudinal diameter of around 5-6 cm, was found in the anterior wall of gastric antrum. The tumor was dissected and totally removed, enucleated, through an incision of gastric serosa without any technical difficulties (Figure 2). Explorative gastrotomy, endoluminal check of mucosa, and edge resection of underlying layers of gastric wall were performed. Gastrotomy was closed with PDS 3.0 using one layer Gambee sutures. Macroscopically, the specimen was capsulated by fatty content in a size of 5.5 cm. Histologicaly, the diagnosis of lipoma containing mature well-differentiated adipocytes (Figure 3), and no pathological lession in resected gastric edges were confirmed. Postoperative course was uneventful and the patient was discharged on the seventh postoperative day. Clinical and endoscopy follow-up 1 and 4 mo later showed that the tumor and clinical symptoms disappeared completely.
DISCUSSION
Lipomas of the stomach are very rare, accounting for less than 3% of all benign tumors of stomach[10,13]. Although generally single, they can be multiple as well[14]. Subserosal gastric lipomas are extremely rarely symptomatic. Probably because of this, there is no report on treatment of subserosal gastric lipomas in the English medical literature. In our case, subserosal lipoma localized in the antrum caused symptoms such as upper abdominal pain, dyspeptic disorders, and vomiting. This location is mainly responsible for dyspeptic and obstructive symptomatology[15,16]. The size of the lesion is correlated with the onset of abdominal disorders[7,10].
Diagnosis of gastric lipoma, in the past, before the era of modern diagnostic technology, was generally made after surgery[9,15]. Usually, on barium studies, extra mucosal tumors including lipomas reveal a smooth filling defect with a “bull’s eye” appearance that is indistinguishable from other mesenchymal tumors[3]. Computerized tomography is a highly specific imaging diagnostic tool for lipoma[1,3,7,17]. In our case, barium studies did not show any filling defect, whereas abdominal CT scan showed a homogeneous well-defined oval mass with negative densitometry values of -50 and -60 Hounsfield units that corresponds to lipoma (Figure 1). However, CT scan is not accurate in determining the layer of location in the gastric wall. Although endoscopic sonography (EUS) provides more accurate findings of submucosal tumors regarding their shape, size and location inside gastric walls[18], because of limited resources in our hospital, this technique is not available. Upper GI tract endoscopy and biopsies were performed twice for our case. However, they played a complementary role in offering a description of a soft submucosal oval-shaped mass in gastric antrum, normal overlying mucosa and histopathology findings. A clear-cut endoscopic differentiation between gastric lipomas and other submucosal neoplasm is not feasible, because routine endoscopic gastric biopsies do not reach the submucosal layer[16]. Furthermore, in the subserosal location, it was impossible to reach the neoplasm endoscopically. Despite the fact that CT scan is highly pathognomonic, there are reports suggesting the necessity of verifying specificity and sensibility of non-radiation based imaging systems, such as high resolution transabdominal ultrasound (TAUS)[19] and abdominal magnetic resonance imaging (MRI)[16].
The treatment modalities for gastric lipomas have been changed in parallel with the advances in endoscopic and imaging techniques. The choice of treatment for gastric lipomas is still controversial[16]. It was reported that different surgical and endoscopic procedures have been used in treatment of submucosal lipomas, but more accurate diagnosis preoperatively enable the replacement of previously used resection methods[6,9] by limited procedures such as tumor enucleation, partial resection or other endoscopic and minimally invasive procedures[4,7,10,11,20]. Although there are no malignant transformations of a gastric lipoma, coincidental separated malignant lesions have been reported[18]. As it was discussed by Yamamoto et al[18] in 2004, submucosal lipomas that have extended into the gastric lumen may provoke repeat erosions or local inflammation of gastric epithelium, which is thought to promote gastric cancer. Therefore, complete pretreatment diagnostic evaluation is needed. In our patient, preoperative evaluation did not find any morphologic and histological pathology in the gastric epithelium. Since his lipoma was symptomatic and its location in the gastric wall was not diagnosed preoperatively, the patient was treated with open laparotomy. Intraoperatively, a subserosal lipoma was found and enucleated through an incision of gastric serosa. To rule out the underlying concomitant pathology, explorative gastrotomy and edge resection of the gastric wall were carried out.
In summary, we report here a very rare case of subserosal symptomatic gastric lipoma successfully treated with enucleation. Subserosal gastric lipoma, although extremely rare, can be the cause of abdominal pain and dyspeptic disorders that need surgical treatment. Accurate diagnosis of gastric lipoma, which can be reached with a combination of endoscopic and imaging diagnostic techniques, is a very useful precondition in choosing the appropriate, less mutilating procedures of treatment.