Published online Sep 21, 2008. doi: 10.3748/wjg.14.5371
Revised: June 2, 2008
Accepted: June 9, 2008
Published online: September 21, 2008
Drink tests are advocated as an inexpensive, noninvasive technique to assess gastric function in patients with a variety of upper digestive symptoms. Many patients with dyspeptic complaints will achieve satiation or develop symptoms at ingested volumes below those typically required to achieve these endpoints in controls. Substantial variation in test performance exists and a greater degree of standardization is required. Additionally, it remains unclear exactly what drink tests measure as correlations with measures of gastric sensation, accomodation and emptying are modest at best. Finally, results of drink tests do not guide therapy. At present, these tests are best reserved for research studies and are not advocated for use in clinical practice.
- Citation: Jones MP. Satiety testing: Ready for the clinic? World J Gastroenterol 2008; 14(35): 5371-5376
- URL: https://www.wjgnet.com/1007-9327/full/v14/i35/5371.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.5371
Drink tests were originally developed as a noninvasive means to assess upper digestive sensation and, perhaps, gastric accommodation. These tests are most commonly performed in patients with symptoms of functional dyspepsia or gastroparesis and many patients with these conditions will achieve satiation or develop dyspeptic symptoms at ingested volumes below those typically required to achieve these endpoints in controls. Drink tests are well tolerated, inexpensive and easy to perform. They are variously performed using either water or nutrient-containing solutions administered at different rates. This variability in test performance has limited our understanding of the exact physiologic parameters measured by the test. Drink tests are often used in clinical studies evaluating patients with functional dyspepsia or gastroparesis. Although patients often report satiation or develop symptoms at substantially smaller ingested volumes than controls, it remains unclear exactly what physiologic processes are assessed by the drink test. Additionally, results of drink tests do not guide therapy. As such, these tests are probably best reserved for research studies and are not advocated for use in clinical practice.
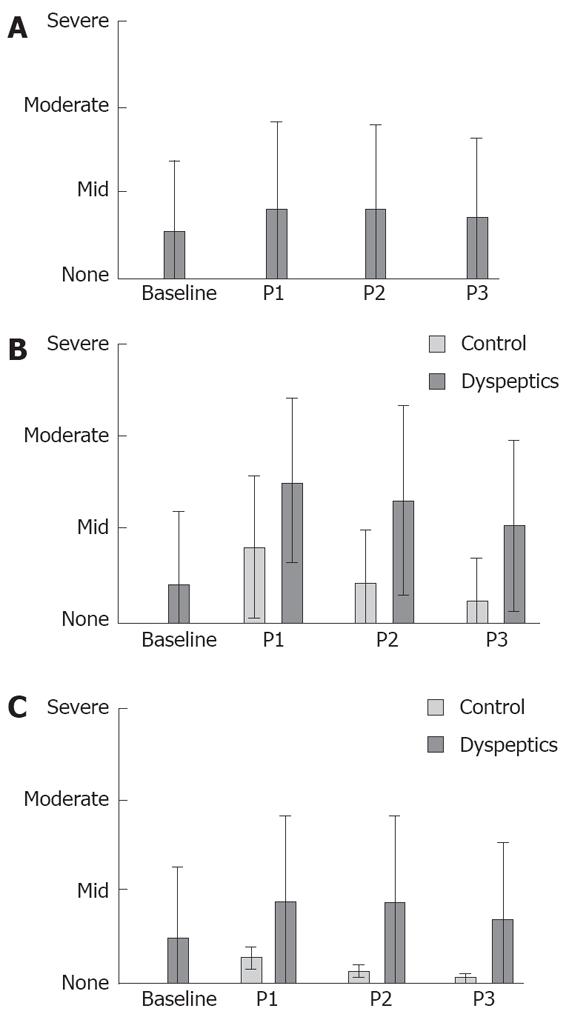
Drink tests were originally developed as a symptom provocative technique for patients with dyspeptic complaints. Patients with dyspepsia will generally drink less and report more symptoms than do healthy subjects. Symptom reporting is influenced to a large degree by the endpoint of the drink test. For example, the 5-min water load test asks subjects to drink room temperature water ad libitum over a 5 min period until they become full[1]. Patients rate symptoms of fullness, nausea and bloating at the end of the drink test and then again 20 min and 30 min after the conclusion of the test. Not surprisingly, scores for the endpoint of fullness do not differ as greatly between patients with functional dyspepsia and controls while patients with functional dyspepsia do report significantly greater scores for symptoms of bloating and nausea (Figure 1)[2]. Compared with controls, symptoms induced by the drink test are more likely to persist in patients with functional dyspepsia compared with controls.
Boeckxstaens et al[3] have evaluated symptom responses to both water and Nutridrink consumed at a rate of 100 mL/min in healthy subjects and patients with functional dyspepsia. After each 100 mL, symptoms of satiety, epigastric bloating, nausea, and pain were scored on a scale from 0 (no sensation) to 5 (discomfort). The test was ended when a score of 5 was reached for at least one of the symptoms and the maximal ingested volume calculated. Subjects also rated these symptoms 1 and 2 h after the end of the drink test. Again, patients with functional dyspepsia reported greater and more persistent symptoms during the drink test than did controls. Nutridrink was more symptom-provoking than water. Importantly, subjects in this study also underwent gastric barostat testing and were classified as having either normal physiology, visceral hypersensitivity or impaired accommodation. Symptom scores during drink tests were not influenced by the results of the barostat study.
While patients with functional dyspepsia will often achieve satiation at lower drink test volumes than controls and will report greater symptoms during the test, specific dyspeptic symptoms are not associated with an abnormal drink test. Jones and Maganti[4] evaluated the relationship between 15 common dyspeptic symptoms and volume to fullness as measured by a 5-min water load test. The only symptom significantly correlated with volume to fullness was nausea which showed a weak inverse correlation with nausea severity (r = -0.3, P = 0.05). Similarly, Boeckxstaens et al[5] reported that while patients with functional dyspepsia were more likely to report more symptoms during drink testing, no specific symptom was more likely to be associated with an abnormal drink test. Finally, Kindt et al[6] recently reported that maximal drink test volume was inversely associated with dyspeptic symptom scores prior to the study. For specific dyspeptic symptoms, only early satiety was significantly associated with the endpoint of the first satiety drinking test (r = 0.25, P = 0.02).
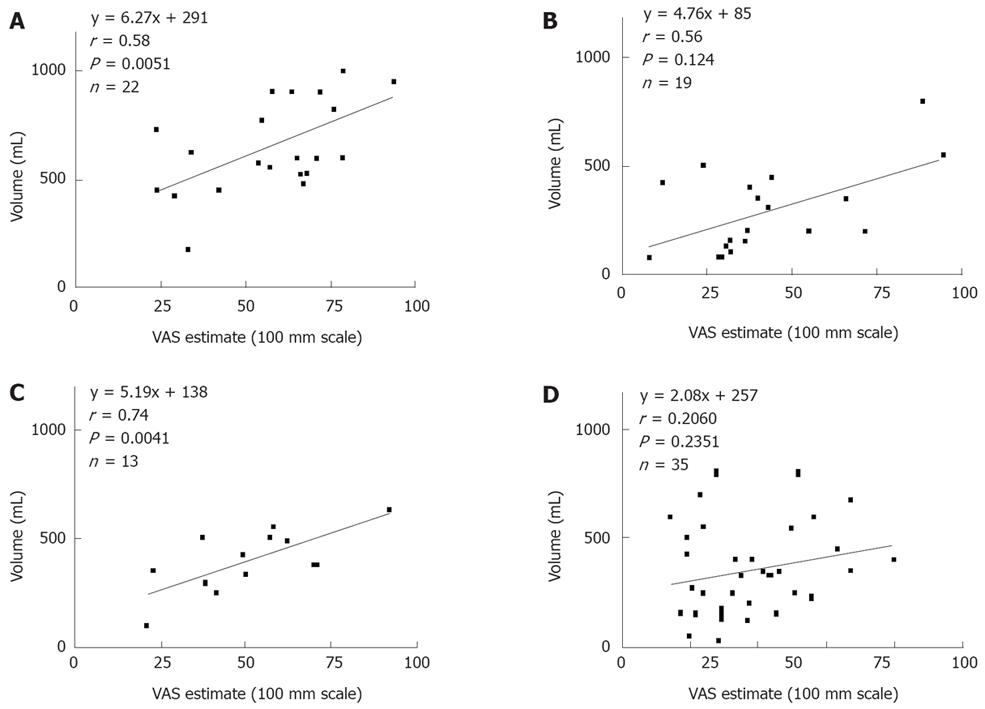
Psychiatric comorbidity is common in functional dyspepsia. In healthy subjects, experimentally induced anxiety is associated with decreased gastric compliance and meal-induced accommodation as well as increased symptom scores during a standard nutrient drink challenge[7]. However, in patients with functional dyspepsia, correlations between drink test volumes and general psychiatric distress (measured using either the SCL-90R or the Psychological General Well Being Scale) have been modest at best[2,4]. We do often encounter patients who report fullness at volumes that clearly defy physiologic parameters (< 50 mL), suggesting that central factors clearly influence test results. Finally, patients with functional dyspepsia, compared with controls, patients with gastroparesis or patients with gastroesophageal reflux often demonstrate poor self-efficacy and are less capable of estimating the volume required to produce fullness (Figure 2)[2].
Assessment of gastric sensation and accommodation is most rigorously measured using a barostat. This is a cumbersome, expensive device that is decidedly patient unfriendly. Logically, it would seem that incrementally distending the stomach by drinking could achieve a result similar to incrementally distending the stomach using a balloon on the end of a catheter. Indeed, Tack et al[8] have reported a good correlation between barostat-measured accommodation and total calories consumed during a nutrient drink test administered at 15 mL/min. For both patients with functional dyspepsia and controls, the correlation was 0.76 (P < 0.001) and the nutrient drink test was calculated to have a sensitivity of 92% and a specificity of 86% in predicting impaired gastric accommodation.
Not all authors have agreed with these findings. Boeckxstaens et al[5] found no correlation between drinking capacity and fundal accommodation to a meal. These authors used both water and nutrient drink tests to evaluate subjects. The sensitivity of the water load test and nutrient drink test to detect impaired accommodation was 73% and 81%, respectively. The discrepant results between these two studies may reflect the methods used. Tack et al[8] had subjects ingest Nutridrink at a rate of 15 mL/min while Boeckxstaens et al[5] had subjects consume Nutridrink or water at 100 mL/min.
Accommodation can also be assessed using single-photon emission computed tomography (SPECT). Using a nutrient drink test administered at a rate of 120 mL/4 min, Gonenne et al[9] found that after controlling for covariates in a convenience sample of controls and patients with functional dyspepsia, the maximal tolerated nutrient drink test volume explained only 13% and 3% of the variations in fasting and postprandial volumes measured by SPECT.
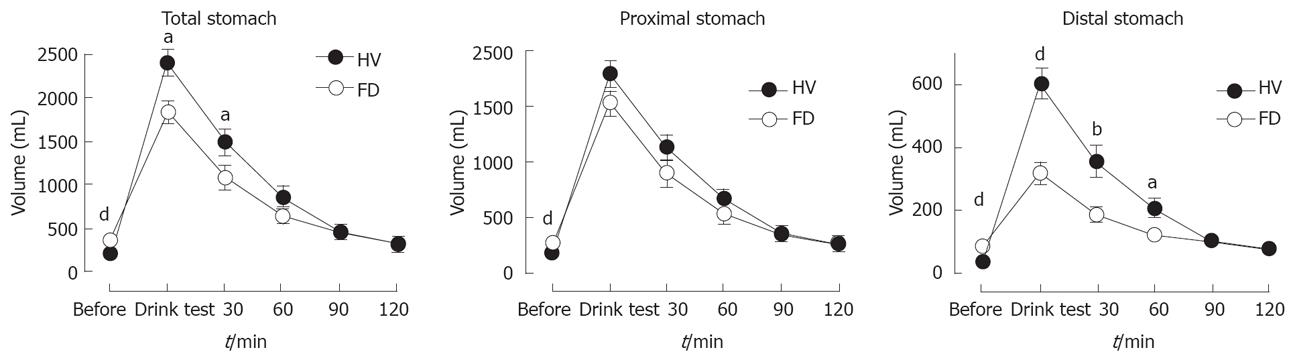
Recently, van den Elzen et al[10] have shown that drinking capacity may be more related to distal rather than proximal stomach function. Compared to controls, patients with functional dyspepsia ingested significantly less water (P < 0.001) and had reduced filling of the distal stomach (P < 0.001) after the drink test (Figure 3).
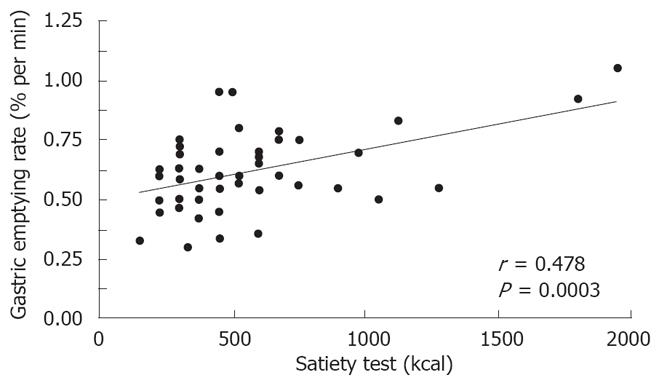
Only a few studies have examined the relationship between gastric emptying and maximal tolerated volume and that relationship appears modest at best. Cuomo et al[11] reported that in females with functional dyspepsia, the correlation between maximal tolerated drink test volume and the fractional rate of gastric emptying was 0.48 (P = 0.0003, Figure 4). Tack et al[8] also reported a weak but significant correlation between maximal tolerated volume for the nutrient drink test and the half time of gastric emptying for a solid meal when pooled controls and patients with functional dyspepsia were studied (r = -0.40, P = 0.001). The correlation was not statistically significant when only evaluating patients with functional dyspepsia. Jones et al[2] did not find a correlation between volume to fullness using a 5-min water load test and Tlag (r = 0.1532, P = 0.4549) or T1⁄2 (r = 0.1489, P = 0.4679) using a stable isotope gastric emptying breath test.
Drink tests are performed using either water or nutrient-containing beverages which are consumed at various rates. No method has proven superior although nutrient drink tests appear to be performed more often in clinical research. Presently, there is a need for a consensus on drink test methodology so that observations made by various investigators will be uniformly interpretable. Limited data exist regarding the performance characteristics of drink tests. Males ingest greater volumes than females but there appears to be less of an influence with respect to age and BMI[2,5,6,8].
Results of drink tests are reproducible at least in the short term. For healthy subjects, the correlations between 5-min water load tests at baseline and repeated 2 wk and 2 mo later were 0.78 (P < 0.0001) and 0.33 (P = 0.16)[2]. Cuomo et al[11] repeated a nutrient drink test between 2 d and 5 d in 10 controls and 5 patients with functional dyspepsia. The resulting inter-day variation of kcal ingested was 4.7% ± 1.5%.
Water loading at different rates produces comparable results in healthy subjects. The correlation between volumes to fullness for the 5-min water load and 100 mL/min water load was 0.79 (P < 0.0001)[2]. For the same subjects, the correlation between the 5-min water load and a 5-min nutrient drink test was 0.20 (P = 0.48). Boeckxstaens et al[5] found a significant correlation between the maximal volume ingested in the water test and the nutrient drink test. The correlation was greatest among controls (r = 0.67, P = 0.0001) and weakest among patients with functional dyspepsia (r = 0.57, P = 0.0001).
Using a 15 mL/min Nutridrink test, Kindt et al[6] demonstrated excellent test-retest reliability for a group that included 34 controls and 78 patients with FD (r = 0.88, P < 0.0001). During repeat testing, controls tended to consume higher volumes while patients with functional dyspepsia showed less variability.
For the 5-min water load test, the mean volume required to produce fullness in a group of 73 controls was 648 ± 204 mL[2]. Males (703 ± 217 mL) drank more than females (611 ± 188 mL), but the difference was not statistically significant (t = 1.907; P = 0.0605). No healthy subject consumed < 300 mL of water and that volume was proposed as a cut-off for an abnormal test. A subsequent study demonstrated that the 300 mL cut-off value for the 5-min water load test discriminated controls from patients with functional dyspepsia with a sensitivity of 98% and a specificity of 46%[12].
For healthy subjects, the mean volume to fullness for the 100 mL/min water load test in controls has been reported as 1128 ± 355 mL[2]. In the same population, the mean volume to fullness for the 5-min nutrient drink test was 688 ± 187 mL. The nutrient drink test was performed using BoostTM (Mead Johnson Nutritionals, Evansville, Indiana) which contains 1.1 kcal/mL and is 70% carbohydrate, 15% fat, and 16% protein. Boost differs somewhat from NutridrinkTM (N.V. Nutricia, Zoetermeer, Netherlands) which contains 1.5 kcal/mL and is 39% fat. BoostTM is comparable to EnsureTM (Abbott Laboratories, Abbott Park, Ill.) which contains 1.06 kcal/mL and is 65% carbohydrate, 20% fat, and 15% protein. These test meals have not been directly compared but Tack et al[8] have shown that with increasing caloric density, maximum satiety occurs at progressively higher caloric intakes while satiety scores according to ingested volumes do not differ significantly. This suggests that volume may be a greater stimulus than caloric density. No study has assessed the influence of caloric composition or palatability.
Boeckxstaens et al[5] have reported normal values for both Nutridrink and water load administered at 100 mL/min. Males consumed significantly more water (2084 ± 181 mL vs 1367 ± 97 mL, P = 0.0001) and Nutridrink (1405 ± 81 mL vs 946 ± 74 mL, P = 0.002) than females. Using the 10th percentile as the lower limit of the normal range, volumes < 1100 mL of water for men and < 800 mL of water for women were considered abnormal. Similarly, volumes < 800 mL of Nutridrink for men and < 600 mL for women were considered abnormal. The difference in results for the 100 mL/min water load tests between these two studies likely reflects the fact that Jones et al[2] had subjects stop drinking when they first experienced fullness while Boeckxstaens et al[5] had patients continue to drink until they developed very severe or uncomfortable sensations of symptoms of satiety, epigastric bloating, nausea or pain.
Using a Nutridrink test administered at a rate of 15 mL/min to healthy volunteers, Tack et al[8] reported that maximum satiety occurred after ingestion of 1005 ± 35 mL (mean ± SE) with a lower limit of normal of 653 mL. This observation was supported by a more recent observation from the same group[2]. In this study, controls reported maximum satiety after ingestion of 937 ± 428 mL. Increasing drink test volumes were associated with male sex and increasing age[6]. Moreover, Chial et al[13] used a nutrient drink test adopted from the methodology of Tack et al[8]. Subjects consumed 120 mL of EnsureTM every 4 min until full, and the average volume of nutrient drink ingested (mean ± SE) was 1181 ± 50 mL. There was a weak but significant correlation (r = 0.29, P = 0.02) between volume to fullness and body mass index.
Given that it is unclear exactly what drink tests measure, and that the test remains poorly standardized, the role of drink tests in clinical practice remains to be established[14,15]. The test has most often been employed in clinical research studies evaluating patients with functional dyspepsia. Water loading is also performed as a provocative maneuver during the performance of electrogastrography[1].
Patients should be studied in the morning after an overnight fast. While certain medications can alter digestive sensation, accommodation or gastric emptying, we do not routinely stop motility or sensory modifying medications for clinical studies.
The 5-min water load test is performed by having subjects drink room temperature tap water ad libitum over a 5-min period until reaching the point of fullness. Water is consumed from an unmarked flask that is taken from the subject and refilled after each drink. The volume required to refill the flask to the initial level is recorded, and the total volume consumed is calculated by summing these volumes. In this way, the flask is “bottomless” and the subject blinded as to the actual volume of water consumed. During the test, patients rate symptoms of fullness, bloating, and nausea using a 4-point Likert scale for each symptom. Scores are recorded at baseline and then every 10 min for a 30-min period after completion of the test. Individual symptoms can therefore receive a total score ranging from 0-12, and the total WL symptom score has a range of 0-36.
Nutrient drink tests can be performed in a several ways. The simplest method is that used by Chial et al[13], in which subjects consume 120 mL of EnsureTM every 4 min until full. Ensure is administered in a paper cup that is refilled every 4 min. At 5 min intervals, participants score fullness using a rating scale that combines verbal descriptors on a scale graded 0-5 [0: no symptoms; 1: first sensation of fullness (threshold); 2: mild; 3: moderate; 4: severe; 5: maximum or unbearable fullness]. Participants are told to stop when a score of 5 is obtained. Postprandial symptoms were measured 30 min after completing the test with participants scoring symptoms of bloating, fullness, nausea and pain using a visual analogue scale (VAS) with 100 mm lines and the words “unnoticeable” and “unbearable” as anchors. The sum of the four 100-mm VAS scales for each symptom provides an aggregate symptom score.
The nutrient drink test used by Boeckxstaens et al[5] had subjects who consumed NutridrinkTM at a rate of 100 mL/min. NutridrinkTM is given in beakers or paper cups filled with 100 mL aliquots. After each 100 mL, symptoms of satiety, epigastric bloating, nausea, and pain are scored on a 5-point Likert scale (0: no sensation; 1: very mild; 2: mild; 3: moderate; 4: severe; 5: very severe or discomfort). When a score of 5 is reached for any symptom, the test ends and the maximal ingested volume is calculated.
Drink test results are reported as the maximal ingested volume. Occasionally, a patient may experience emesis during the test. If emesis occurs, the volume of emesis should be recorded and subtracted from the total ingested volume. Along with the maximal ingested volume, individual and cumulative symptom scores can be reported.
While the utility of drink tests remains to be determined, we find the test most helpful when it is either normal or glaringly abnormal. In the former scenario, the patient can be reassured that gastric function is likely to be intact. The latter scenario is more subjective. Often patients will report maximal fullness after the consumption of physiologically insignificant volumes (< 50 mL). We have not found results from the water load test to be correlated with measures of psychiatric distress or somatization but maximal ingested volumes are positively correlated with quality of life[2,12]. Others have reported that maximal ingested volumes are reduced in patients with depression[16]. While drink tests are not intended as surrogates for assessing psychosocial factors or quality of life, maximal fullness at extremely low volumes may suggest that extra-gastric or central factors are playing an important role in symptom generation, perpetuation or tolerance.
Since the physiologic parameters that determine maximal ingested volumes are not well known at present, drink test results cannot be reasonably used to guide therapy. Few studies have assessed the impact of commonly used treatments for functional dyspepsia on drink test results. A brief, randomized controlled trial found that 14 d of therapy with nortriptyline, mirtazapine or placebo did not alter either maximal ingested volumes or symptom scores[17]. A similar study also found no effect on maximal ingested volume or symptoms in healthy subjects treated with either citalopram, desipramine or placebo for 11 d[18]. In contrast, in healthy subjects, the kappa-opioid agonist asimadoline has been shown to increase maximal tolerated volumes without altering gastric emptying[19].
A small trial randomized patients with functional dyspepsia to biofeedback (breathing exercises using software for vagal biofeedback) or an educational control group[20]. Drinking capacity and quality of life improved significantly more in the biofeedback group than in the control group without any significant change in baseline autonomic activity or intra-gastric volume.
Combining an incomplete understanding of relevant pathophysiologic alterations that might be measured by drink tests with limited data regarding effects of therapy on drink test volumes leads us to conclude that drink tests are of limited utility in guiding clinical management. Until our understanding in this area has evolved, drink tests should not routinely be performed in clinical practice.
Drink tests are often used in clinical studies evaluating patients with functional dyspepsia or gastroparesis. Although patients often report satiation or develop symptoms at substantially smaller ingested volumes than controls, it remains unclear exactly what physiologic processes are assessed by the drink test. Additionally, results of drink tests do not guide therapy. As such, these tests are probably best reserved for research studies and are not advocated for use in clinical practice.
| 1. | Koch KL, Hong SP, Xu L. Reproducibility of gastric myoelectrical activity and the water load test in patients with dysmotility-like dyspepsia symptoms and in control subjects. J Clin Gastroenterol. 2000;31:125-129. |
| 2. | Jones MP, Hoffman S, Shah D, Patel K, Ebert CC. The water load test: observations from healthy controls and patients with functional dyspepsia. Am J Physiol Gastrointest Liver Physiol. 2003;284:G896-G904. |
| 3. | Boeckxstaens GE, Hirsch DP, Kuiken SD, Heisterkamp SH, Tytgat GN. The proximal stomach and postprandial symptoms in functional dyspeptics. Am J Gastroenterol. 2002;97:40-48. |
| 4. | Jones MP, Maganti K. Symptoms, gastric function, and psychosocial factors in functional dyspepsia. J Clin Gastroenterol. 2004;38:866-872. |
| 5. | Boeckxstaens GE, Hirsch DP, van den Elzen BD, Heisterkamp SH, Tytgat GN. Impaired drinking capacity in patients with functional dyspepsia: relationship with proximal stomach function. Gastroenterology. 2001;121:1054-1063. |
| 6. | Kindt S, Coulie B, Wajs E, Janssens J, Tack J. Reproducibility and symptomatic predictors of a slow nutrient drinking test in health and in functional dyspepsia. Neurogastroenterol Motil. 2008;20:320-329. |
| 7. | Geeraerts B, Vandenberghe J, Van Oudenhove L, Gregory LJ, Aziz Q, Dupont P, Demyttenaere K, Janssens J, Tack J. Influence of experimentally induced anxiety on gastric sensorimotor function in humans. Gastroenterology. 2005;129:1437-1444. |
| 8. | Tack J, Caenepeel P, Piessevaux H, Cuomo R, Janssens J. Assessment of meal induced gastric accommodation by a satiety drinking test in health and in severe functional dyspepsia. Gut. 2003;52:1271-1277. |
| 9. | Gonenne J, Castillo EJ, Camilleri M, Burton D, Thomforde GM, Baxter KL, Zinsmeister AR. Does the nutrient drink test accurately predict postprandial gastric volume in health and community dyspepsia? Neurogastroenterol Motil. 2005;17:44-50. |
| 10. | van den Elzen BD, Bennink RJ, Holman R, Tytgat GN, Boeckxstaens GE. Impaired drinking capacity in patients with functional dyspepsia: intragastric distribution and distal stomach volume. Neurogastroenterol Motil. 2007;19:968-976. |
| 11. | Cuomo R, Sarnelli G, Grasso R, Bruzzese D, Pumpo R, Salomone M, Nicolai E, Tack J, Budillon G. Functional dyspepsia symptoms, gastric emptying and satiety provocative test: analysis of relationships. Scand J Gastroenterol. 2001;36:1030-1036. |
| 12. | Jones MP, Roth LM, Crowell MD. Symptom reporting by functional dyspeptics during the water load test. Am J Gastroenterol. 2005;100:1334-1339. |
| 13. | Chial HJ, Camilleri C, Delgado-Aros S, Burton D, Thomforde G, Ferber I, Camilleri M. A nutrient drink test to assess maximum tolerated volume and postprandial symptoms: effects of gender, body mass index and age in health. Neurogastroenterol Motil. 2002;14:249-253. |
| 14. | Bratten J, Jones MP. New directions in the assessment of gastric function: clinical applications of physiologic measurements. Dig Dis. 2006;24:252-259. |
| 15. | Mimidis K. Drinking tests in functional dyspepsia: what do they really measure? Neurogastroenterol Motil. 2007;19:947-950. |
| 16. | Strid H, Norström M, Sjöberg J, Simrén M, Svedlund J, Abrahamsson H, Björnsson ES. Impact of sex and psychological factors on the water loading test in functional dyspepsia. Scand J Gastroenterol. 2001;36:725-730. |
| 17. | Choung RS, Cremonini F, Thapa P, Zinsmeister AR, Talley NJ. The effect of short-term, low-dose tricyclic and tetracyclic antidepressant treatment on satiation, postnutrient load gastrointestinal symptoms and gastric emptying: a double-blind, randomized, placebo-controlled trial. Neurogastroenterol Motil. 2008;20:220-227. |
| 18. | Talley NJ, Camilleri M, Chitkara DK, Bouras E, Locke GR 3rd, Burton D, Rucker MJ, Thapa P, Zinsmeister AR. Effects of desipramine and escitalopram on postprandial symptoms induced by the nutrient drink test in healthy volunteers: a randomized, double-blind, placebo-controlled study. Digestion. 2005;72:97-103. |
| 19. | Delgado-Aros S, Chial HJ, Camilleri M, Szarka LA, Weber FT, Jacob J, Ferber I, McKinzie S, Burton DD, Zinsmeister AR. Effects of a kappa-opioid agonist, asimadoline, on satiation and GI motor and sensory functions in humans. Am J Physiol Gastrointest Liver Physiol. 2003;284:G558-G566. |
| 20. | Hjelland IE, Svebak S, Berstad A, Flatabo G, Hausken T. Breathing exercises with vagal biofeedback may benefit patients with functional dyspepsia. Scand J Gastroenterol. 2007;42:1054-1062. |
Peer reviewer: Benedicte Y De Winter, President, Chief, MD, PhD, Professor, University of Antwerp, Laboratory of Gastroenterology, Campus Drie Eiken, Universiteitsplein 1, 2610 Antwerp, Belgium
S- Editor Zhong XY L- Editor Kumar M E- Editor Yin DH