Published online Sep 14, 2008. doi: 10.3748/wjg.14.5353
Revised: August 11, 2008
Accepted: August 18, 2008
Published online: September 14, 2008
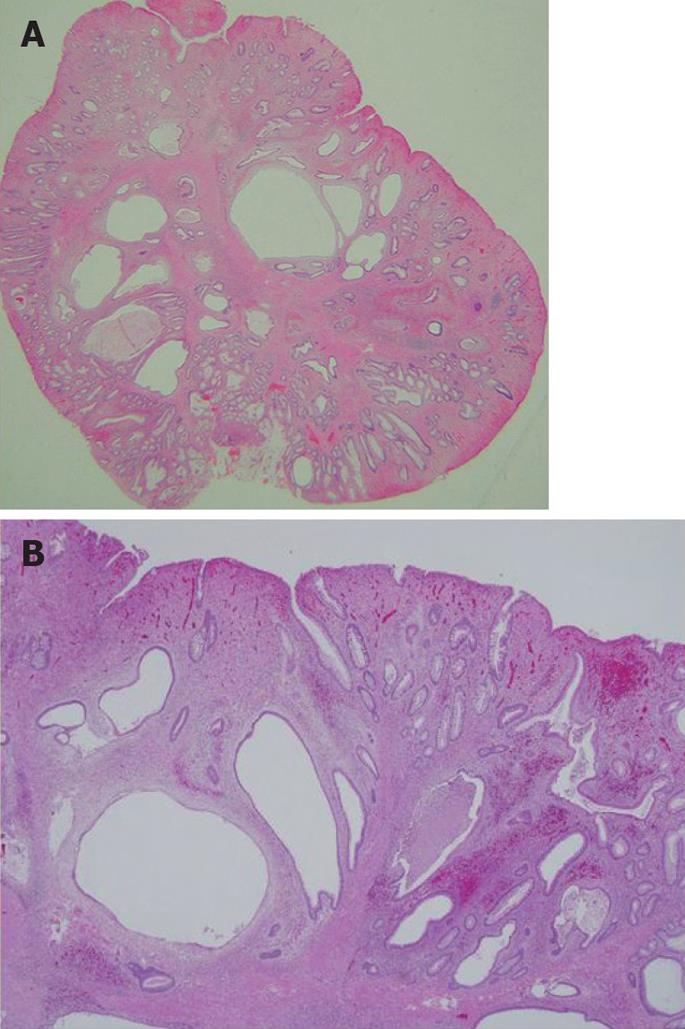
A case of inflammatory myoglandular polyp (IMGP) causing hematochezia is reported. The patient was a 33-year-old man who visited our hospital for further evaluation of hematochezia. Colonoscopy revealed a red, hard, spherical peduncular polyp with erosion and mucous exudation, about 20 mm in diameter, in the descending colon. Excluding the polyp, there was no lesion in the colorectum. Endoscopic polypectomy was performed. Histological examination of the specimen revealed inflammatory granulation tissue in the lamina propria, proliferation of smooth muscle, and hyperplastic glands with variable cystic changes. This polyp was diagnosed as an IMGP. The symptom of hematochezia was resolved after endoscopic resection. Our case shows that treatment is necessary for IMGP if intestinal bleeding occurs and endoscopists should be aware of the endoscopic characteristics of IMGP.
- Citation: Hirasaki S, Okuda M, Kudo K, Suzuki S, Shirakawa A. Inflammatory myoglandular polyp causing hematochezia. World J Gastroenterol 2008; 14(34): 5353-5355
- URL: https://www.wjgnet.com/1007-9327/full/v14/i34/5353.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.5353
Inflammatory myoglandular polyp (IMGP) is characterized by inflammatory granulation tissue in the lamina propria[1], proliferation of smooth muscle[2], and hyperplastic glands with variable cystic changes[3-7]. Only a small number of cases have been reported and the pathogenesis and natural history remain unclear[8-12]. Herein, we describe a relatively rare case of inflammatory myoglandular polyp causing hematochezia.
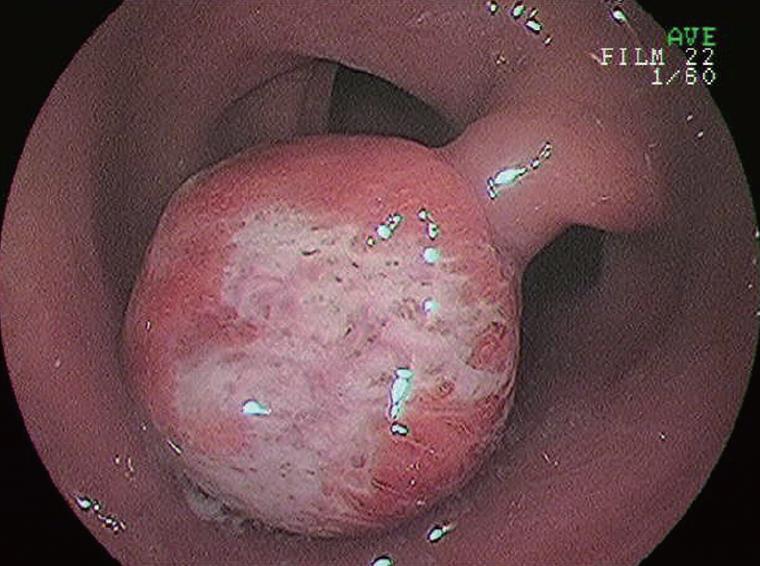
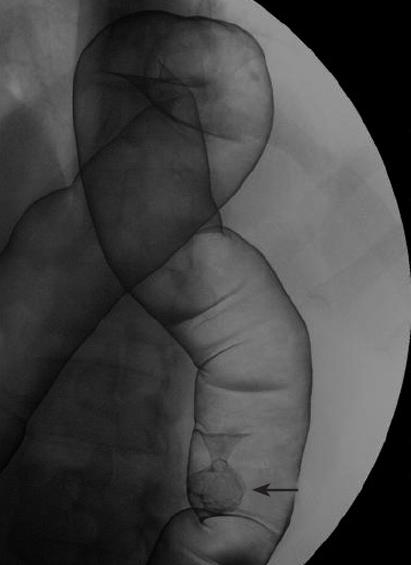
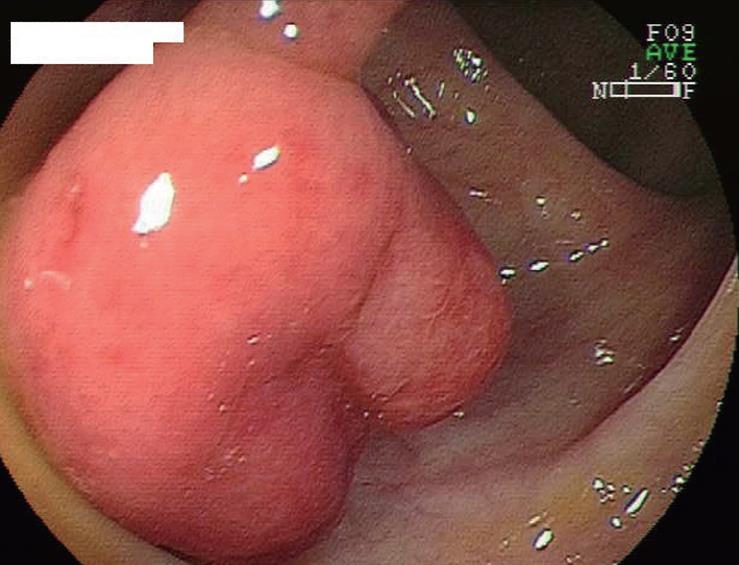
A 33-year-old man presented with the symptom of hematochezia. He was in good health with no specific family or past medical history. His body temperature was 36.7°C, blood pressure was 148/82 mmHg, and radial pulse rate was 70 beats/min and regular. He had neither anemia nor jaundice. Neurological examination revealed no abnormal findings. Abdominal palpation revealed tenderness in the left lower quadrant. Routine hematological examination and biochemical tests were within normal limits. Colonoscopy revealed a red, hard, spherical peduncular polyp with erosion and mucous exudation, about 20 mm in diameter, in the descending colon (Figure 1). With conventional colonoscopy, the lesion did not show type III or IV pit pattern although magnifying colonoscopy was not performed. We speculated that this polyp was non-neoplastic. It was suspected to be an inflammatory polyp from endoscopic findings although it should be distinguished from a juvenile polyp. An air contrast barium enema also revealed a pedunculated polyp in the descending colon (Figure 2). Excluding the polyp, there was no lesion in the colorectum. We speculated that the polyp in the descending colon was the causative lesion of hematochezia. Endoscopic polypectomy was performed. At polypectomy, polyp erosion was healed (Figure 3). Histological examination of the specimen revealed inflammatory granulation tissue in the lamina propria, proliferation of smooth muscle, and hyperplastic glands with variable cystic changes (Figure 4). The lesion was diagnosed as an IMGP. After endoscopic polypectomy, the symptom of hematochezia was resolved.
IMGP is a non-neoplastic colorectal polyp, first described by Nakamura et al[1]. IMGP is solitary, pedunculated and rarely, covered by a fibrin cap, and follows a benign course. Also, IMGP has no association with inflammatory bowel diseases and is located not only in the rectosigmoid, but also in the descending and transverse colon[3]. In the present case, it was located in the descending colon. Although the pathogenesis of IMGP remains unknown, Nakamura[1] proposed that chronic trauma from intestinal peristalsis may contribute to the pathogenesis of IMGP.
Only a small number of IMGP cases have been reported. According to Fujino et al[8], a review of the literature revealed 48 cases of IMGP in the large intestine up to 2001. However, recent advances in diagnostic techniques, especially the widespread use of colonoscopy for colorectal tumors, have enabled us to identify small and asymptomatic polyps, and reports on IMGP of the colon have been increasing[9,10]. Fujino et al[8] described that the macroscopic appearance is the pedunculated type in 83.3% of cases. In that report, the sites of IMGP in the large intestine were studied and 47 of 48 cases (97.9%) had lesions in the rectum to transverse colon. Thus, IMGPs of the large intestine are predominantly in the distal colon[8,9]. IMGPs in the colon are usually asymptomatic and often detected incidentally on barium enema or endoscopy[8-10]. Another review of the literature revealed that the main clinical feature of colorectal IMGPs is hematochezia[10,11]. Endoscopic characteristic findings include (1) pedunculated or semipedunculated, (2) red and (3) smooth, spherical and hyperemic surface with patchy mucous exudation and erosion[8,9]. In the present case, the endoscopic findings of the polyp were compatible with those of IMGP.
As to therapy, IMGP of the large intestine can best be removed endoscopically, because it is thought to be clinically and histologically benign. Most Japanese cases have been treated with polypectomy or endoscopic mucosal resection (EMR)[5,7-11]. If we could confirm the histological diagnosis of small colonic IMGPs by endoscopic biopsy, endoscopic resection of IMGP might be unnecessary because IMGP follows a benign course. However, the diagnosis of colorectal IMGPs could seldom be made by endoscopic biopsy and the final diagnosis of colonic IMGP depends on the pathological findings of EMR or endoscopic polypectomy specimens. Endoscopic or surgical treatment is necessary if gastrointestinal bleeding[9] or colonic intussusception occurs. Local excision of the polyp is curative. Kayhan et al[12] have reported a case of large IMGP (> 6 cm) that was too large to be removed endoscopically, and was thus treated with surgical resection. We consider that the percentage of patients with colonic IMGP who undergo surgical resection will decrease and endoscopic resection will increase in the future because of recent advances in diagnostic technologies such as improved endoscopic images.
In conclusion, we report a case of IMGP causing hematochezia. IMGP should generally be taken into consideration as a differential diagnosis of peduncular polyp of the colon. IMGP of the large intestine is not fatal and patients remain asymptomatic in their daily lives except for gastrointestinal bleeding or bowel obstruction. Therefore, it is likely that there are many latent patients with IMGP who might be incidentally discovered in the future. Endoscopists should be aware of that IMGP may exhibit the aforementioned endoscopic characteristics and may cause hematochezia. The causes of IMGP are still obscure, and further accumulation of cases may disclose their pathogenesis.
| 1. | Nakamura S, Kino I, Akagi T. Inflammatory myoglandular polyps of the colon and rectum. A clinicopathological study of 32 pedunculated polyps, distinct from other types of polyps. Am J Surg Pathol. 1992;16:772-779. |
| 2. | Griffiths AP, Hopkinson JM, Dixon MF. Inflammatory myoglandular polyp causing ileo-ileal intussusception. Histopathology. 1993;23:596-598. |
| 3. | Bhathal PS, Chetty R, Slavin JL. Myoglandular polyps. Am J Surg Pathol. 1993;17:852-853. |
| 4. | Gomez Navarro E, del Rio Martin JV, Sarasa Corral JL, Melero Calleja E. [Myoglandular inflammatory polyp located in the distal end of the rectum]. Rev Esp Enferm Dig. 1994;85:45-46. |
| 5. | Nagata S, Sumioka M, Sato O, Miyamoto M, Watanabe C, Yamada H, Hirata K, Imagawa M, Haruma K, Kajiyama G. [Five cases of inflammatory myoglandular polyp]. Nippon Shokakibyo Gakkai Zasshi. 1998;95:145-150. |
| 6. | Bhardwaj K, Mohan H, Chopra R, Bhardwaj S, Sachdev A. Inflammatory myoglandular polyp of rectum. Indian J Gastroenterol. 1998;17:63-64. |
| 7. | Harada N, Chijiiwa Y, Yao T, Koyanagi M, Ono Y, Motomura S. Inflammatory myoglandular polyp. J Clin Gastroenterol. 1999;29:104-105. |
| 8. | Fujino Y, Orii S, Nakamura S, Sugai T, Saito S, Yamaguchi T, Noro S, Ishii M, Inomata M, Suzuki K. Five cases of colorectal inflammatory myoglandular polyps. Gastroenterological Endoscopy. 2001;43:1281-1286. |
| 9. | Moriyama T, Matsumoto T, Hizawa K, Tada S, Fuchigami T, Iwai K, Yao T, Iida M. Inflammatory myoglandular colorectal polyps: a case series of nine patients. Endoscopy. 2003;35:363-365. |
| 10. | Tashiro M, Yoshikawa I, Matsuhashi T, Yamasaki T, Nishikawa S, Taguchi M, Yamasaki M, Kume K, Otsuki M. Images of interest. Gastrointestinal: inflammatory myoglandular polyp of the colon. J Gastroenterol Hepatol. 2005;20:1123. |
| 11. | Becheanu G, Stamm B. Inflammatory myoglandular polyp--a rare but distinct type of colorectal polyps. Pathol Res Pract. 2003;199:837-839. |
| 12. | Kayhan B, Kucukel F, Akdogan M, Ozaslan E, Kucukbas TA, Atoglu O. Inflammatory myoglandular polyp: a rare cause of hematochezia. Turk J Gastroenterol. 2004;15:117-119. |
Peer reviewer: Dr. James E East, Department of Gastroenterology, St. Mary’s Hospital, Clarence Wing, Praed Street, London W2 1NY, United Kingdom
S- Editor Zhong XY L- Editor Wang XL E- Editor Zhang WB