Published online Jul 14, 2008. doi: 10.3748/wjg.14.4249
Revised: May 21, 2008
Accepted: May 28, 2008
Published online: July 14, 2008
Arteriovenous fistula (AVF) involving the inferior mesenteric vessels is rare, and the affected patients usually present with abdominal pain, mass, or features of established portal hypertension. Colonic ischemia is a less common and more serious manifestation of AVF. We report a case of ischemic colitis secondary to inferior mesenteric AVF in a patient who underwent a previous liver transplantation, subsequently developed portal vein stenosis, and then presented with acute lower gastrointestinal bleeding. He underwent percutaneous transhepatic placement of a portal vein stent and left colectomy.
- Citation: Kim IH, Kim DG, Kwak HS, Yu HC, Cho BH, Park HS. Ischemic colitis secondary to inferior mesenteric arteriovenous fistula and portal vein stenosis in a liver transplant recipient. World J Gastroenterol 2008; 14(26): 4249-4252
- URL: https://www.wjgnet.com/1007-9327/full/v14/i26/4249.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4249
Arteriovenous fistula (AVF) in the portal circulation is rare and usually involves the hepatic, splenic, or superior mesenteric vessels[1]. Inferior mesenteric AVF is uncommon, and only isolated cases have been reported[23]. Though inferior mesenteric AVF may be congenital[4–6], it results more often from penetrating traumas, such as a gunshot or knife wound, or may be a complication of arterial catheterization or abdominal surgery with bowel resection[237–9]. Inferior mesenteric AVF usually presents with abdominal pain, mass, or features of established portal hypertension[23]. Colonic ischemia is a less common and more serious manifestation of AVF[2].
Portal vein stenosis is a relatively rare vascular complication affecting 1%-2% of patients who have undergone orthotopic liver transplantation[1011]. Clinical symptoms of portal vein stenosis are usually less pronounced. Patients carrying this diagnosis may develop portal hypertension with ascites and esophageal varices, but portal vein stenosis is potentially devastating, leading to graft failure[1011].
We report a case of ischemic colitis secondary to an inferior mesenteric AVF in a patient who underwent a previous liver transplantation, subsequently developed portal vein stenosis, and then presented with acute lower gastrointestinal bleeding.
A 46-year-old man was admitted to our hospital for abdominal pain and hematochezia. Two years previously, he underwent cadaveric, orthotopic, whole liver transplantation due to hepatitis B-associated decompensated hepatic cirrhosis. Forty-two days after liver transplantation, the patient developed cyto-megalovirus colitis which was treated with intravenous ganciclovir, 5 mg/kg, twice per day for 4 wk. Follow-up colonoscopy showed healing of ulcers, and serology showed negative cytomegalovirus antigenemia. The patient had no history of abdominal trauma or abdominal surgery other than liver transplantation.
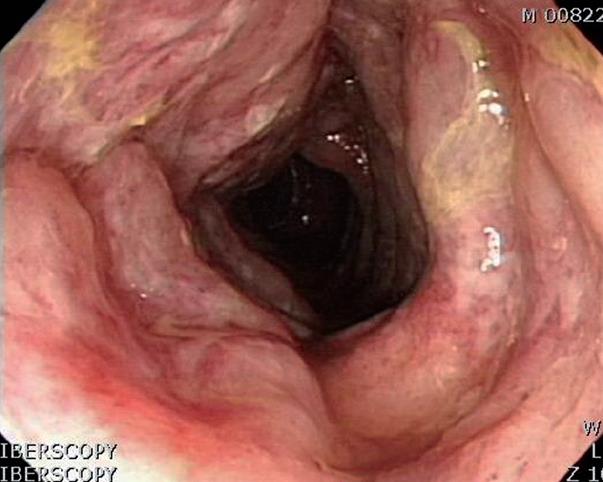
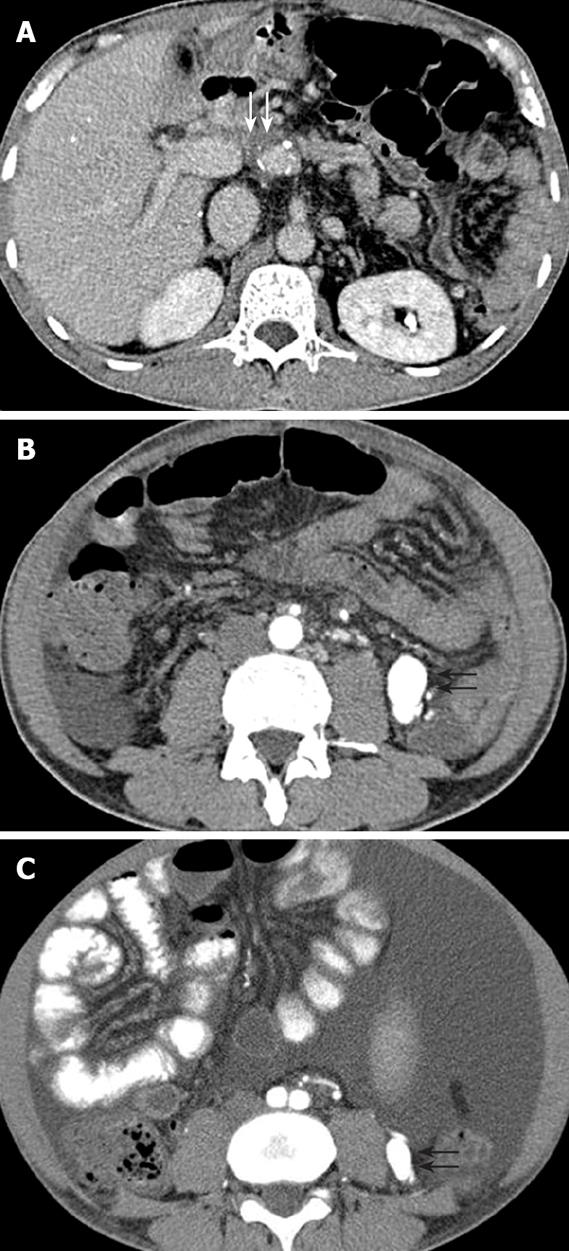
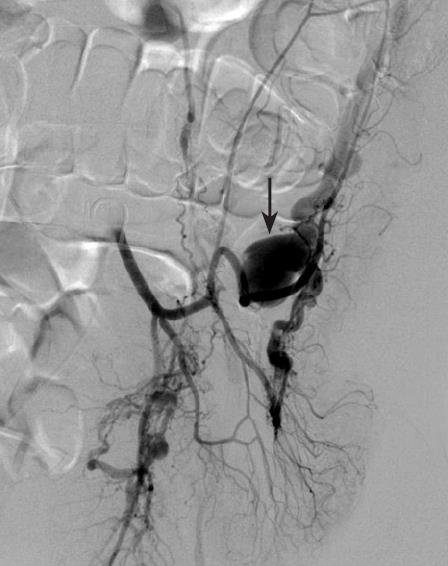
At the first clinical examination, the lower abdomen was distended and painful, but bowel sounds were decreased. Hematologic, biochemical and liver function tests showed 10.2 × 103 /mm3 white blood cells, 29.5 × 103 /mm3 red blood cells, 9.7 g/dL hemoglobin, 167 × 103 /mm3 platelet count, 75.3 mg/L C-reactive protein (range ≤ 5), 32 mg/dL blood urea nitrogen, 0.68 mg/dL serum creatinine, 45 U/L alanine aminotransferase, 15 U/L aspartate aminotransferase, 1.24 mg/dL total bilirubin, and 3.2 g/dL serum albumin. Colonoscopy showed diffuse ulceration, exudate, and hemorrhage in the sigmoid and descending colon, associated with narrowing of the lumen (Figure 1). Histopathologic evaluation of biopsy specimens from the colon revealed mucosal and submucosal hemorrhage and edema, with partial necrosis and ulceration of the mucosa. Blood and tissue analysis for cytomegalovirus and Clostridium difficile was negative. Stool cultures and samples were also negative for bacteria and parasites. A clinical diagnosis of ischemic colitis was made. Contrast-enhanced computed tomography (CT) showed severe stenosis at the anastomosis of the donor portal vein and the native portal vein (Figure 2A), and a 30 mm × 18 mm enhancing vascular structure in the left lower abdominal cavity connecting to the inferior mesenteric vein associated with venous stasis in the mesenteric vein (Figure 2B). Diffuse thickening of the wall of the sigmoid colon without mucosal enhancement was also seen. We reviewed a previous CT scan performed before liver transplantation and found a 10 mm × 8 mm enhancing vascular structure at the same location, indicating that the structure was increased in size over the two years following transplantation (Figure 2C). Angiography of the inferior mesenteric artery showed both the artery and its partner vein emerging from the lesion, along with very early opacification of the markedly dilated inferior mesenteric vein (Figure 3). Based on this, the mass-like vascular lesion was diagnosed as an AVF. Angiography also showed an additional small inferior mesenteric AVF with venous dilatation and decreased perfusion of the sigmoid colon. We felt that portal hypertension secondary to portal vein stenosis developed after liver transplantation, which contributed to enlargement of the inferior mesenteric AVF and venous congestion, and then resulted in decreased perfusion of the sigmoid colon and ischemic colitis. Therefore, we decided to attempt a percutaneous angioplasty for the portal vein stenosis and surgical repair of the inferior mesenteric AVF associated with severe ischemic change in the sigmoid colon.
The patient underwent a percutaneous transhepatic portography for portal vein stenosis. Portogram revealed an almost complete obstruction at the extrahepatic anastomosis of the portal vein and a marked delay of venous drainage of the mesenteric vein (Figure 4A). A 14 mm × 4 cm self-expandable bare metallic stent was deployed in the stenotic portal vein area, and a 10 mm × 4 cm balloon was dilated for residual stenosis. Portogram performed after stent deployment revealed good patency of the portal vein and no continuous contrast filling in the mesenteric vein (Figure 4B).
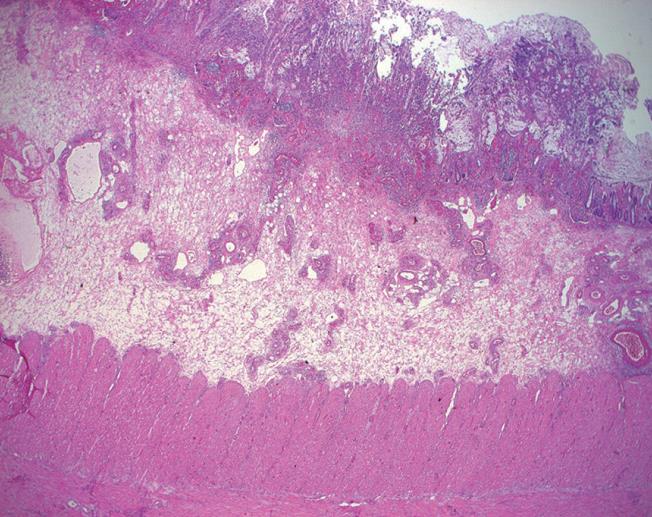
Two days after percutaneous angioplasty, the patient underwent a laparotomy for colon ischemia. After the mesocolon was ligated and divided, the sigmoid and descending colon with fistulae were resected. Pathological examination of the resected specimens demonstrated extensive necrosis of mucosa, diffuse inflammatory infiltrations extending into submucosa, and focally hyalinized thick-wall vessels, which were compatible with the symptoms of ischemic colitis (Figure 5). The patient’s postoperative course was uneventful, and an abdominal CT scan 6-mo later showed a mildly dilated inferior mesenteric vein without aneurysmal dilatation. The portal vein stent patency was good, with homogeneous enhancement of the liver.
Inferior mesenteric AVF is a rare splanchnic AVF. Only 11 cases have been reported in the literature[3]. Our patient had no history of abdominal trauma or abdominal surgery other than liver transplantation. An abdominal CT scan performed before liver transplantation demonstrated a small inferior mesenteric AVF, suggesting that the fistula is congenital in origin and increases in size after transplantation, resulting in the patient’s presentation.
The common clinical symptoms and signs of inferior mesenteric AVF include abdominal pain, mass, or bruit, or a combination of these symptoms[23]. More serious manifestations of mesenteric AVF are associated with portal hypertension, which is present in about 50% of patients with splanchnic AVF[1]. Okada et al[3] reported that 7 of 11 patients with inferior mesenteric AVF had either signs or symptoms of portal hypertension (mainly ascites, esophageal varices, or splenomegaly) or elevated portal venous pressure. Portal hypertension in an inferior mesenteric AVF is called “forward” or “hyperkinetic” portal hypertension and may result from both increased blood flow into the portal system and from compensatory increase in hepatic vascular resistance[2312]. Inferior mesenteric AVF may also be a factor predisposing to non-occlusive ischemic colitis[2]. An AVF is usually associated with decreased arterial blood flow to the tissue beyond it and increased venous pressure distal to it[212].
Portal venous stenosis in patients who have undergone orthotopic liver transplantation may be caused by disparity in the diameters of recipient and donor portal veins (particularly in pediatric transplanta-tions). Cryopreserved grafts, excessively long vessel stumps or thrombotic occlusion of the veno-venous bypass, or portosystemic shunt surgery can be used prior to transplantation[101113]. The majority of those patients who are found to have portal vein stenosis are otherwise asymptomatic and detected on routine screening ultrasound[10]. Contrast-enhanced CT scan and magnetic resonance imaging can clearly show portal vein stenosis. When patients are symptomatic, they also present with typical signs of portal hypertension, including ascites, esophageal varices, and splenomegaly with or without thrombocytopenia.
The present patient reported no usual symptoms of ischemic colitis, such as hematochezia, melena, or abdominal pain before liver transplantation. However, he suffered from esophageal variceal hemorrhages and ascites, which were thought to be caused by advanced hepatic cirrhosis and portal hypertension. Two years after transplantation, he presented with abdominal pain and hematochezia. Colonoscopy and histopathologic evaluation of biopsy specimens revealed ischemic colitis in the sigmoid and descending colon, and radiologic evaluation showed an inferior mesenteric AVF and portal vein stenosis, suggesting that the portal vein stenosis induced portal hypertension is associated with hepatofugal flow. High arterial flow due to inferior mesenteric AVF and venous stasis in the fistula due to hepatofugal flow, may have contribute to the pseudoaneurysmal dilatation of the inferior mesenteric vein in our patient, leading to augmentation of the preexisting inferior mesenteric AVF and induced the development of ischemic colitis due to steal phenomenon.
Percutaneous transhepatic balloon angioplasty or placement of metal stent has been widely accepted as a safe and effective procedure for portal vein stenosis following liver transplantation[13]. Our patient underwent percutaneous transhepatic deployment of a metal stent with balloon angioplasty. The stent patency was good, the stenosis was disappeared after treatment.
The choice of therapy for inferior mesenteric AVF is surgical correction with or without associated bowel resection[3]. Some studies reported that percutaneous endovascular embolization of the feeding artery may be useful in selected cases, particularly in critically ill patients[247]. In our case, the combination of clinical state, CT and endoscopic images and the presence of the large AVF all prompted a surgical repair.
Inferior mesenteric AVF is rare, but may be associated with portal hypertension and non-occlusive ischemic colitis. To our knowledge, this is the first report of inferior mesenteric AVF-induced ischemic colitis complicated by portal vein stenosis developed after liver transplantation.
| 1. | Van Way CW 3rd, Crane JM, Riddell DH, Foster JH. Arteriovenous fistula in the portal circulation. Surgery. 1971;70:876-890. |
| 2. | Capron JP, Gineston JL, Remond A, Lallement PY, Delamarre J, Revert R, Veyssier P. Inferior mesenteric arteriovenous fistula associated with portal hypertension and acute ischemic colitis. Successful occlusion by intraarterial embolization with steel coils. Gastroenterology. 1984;86:351-355. |
| 3. | Okada K, Furusyo N, Sawayama Y, Ishikawa N, Nabeshima S, Tsuchihashi T, Kashiwagi S, Hayashi J. Inferior mesenteric arteriovenous fistula eight years after sigmoidectomy. Intern Med. 2002;41:543-548. |
| 4. | Matsui A, Iwai K, Kawasaki R, Wada T, Mito Y, Doi T. [Transcatheter embolization of an inferior mesenteric arteriovenous fistula with frequent mucous diarrhea]. Nippon Shokakibyo Gakkai Zasshi. 2007;104:194-199. |
| 5. | Baranda J, Pontes JM, Portela F, Silveira L, Amaro P, Ministro P, Rosa A, Pimenta I, Andrade P, Bernardes A. Mesenteric arteriovenous fistula causing portal hypertension and bleeding duodenal varices. Eur J Gastroenterol Hepatol. 1996;8:1223-1225. |
| 6. | Manns RA, Vickers CR, Chesner IM, McMaster P, Elias E. Portal hypertension secondary to sigmoid colon arteriovenous malformation. Clin Radiol. 1990;42:203-204. |
| 7. | Fabre A, Abita T, Lachachi F, Rudelli P, Carlier M, Bocquel JB, Remond A, Pech de Laclause B, Maisonnette F, Durand-Fontanier S. [Inferior mesenteric arteriovenous fistulas. Report of a case]. Ann Chir. 2005;130:417-420. |
| 8. | Peer A, Slutzki S, Witz E, Abrahmsohn R, Bogokowsky H, Leonov Y. Transcatheter occlusion of inferior mesenteric arteriovenous fistula: a case report. Cardiovasc Intervent Radiol. 1989;12:35-37. |
| 9. | Houdard C, Helenon C, Carles JF, Botella R, Favre M, Boulay J, Boschet P. [Inferior mesenteric arteriovenous fistula and ulcerative rectocolitis]. Arch Fr Mal App Dig. 1970;59:463-474. |
| 10. | Settmacher U, Nussler NC, Glanemann M, Haase R, Heise M, Bechstein WO, Neuhaus P. Venous complications after orthotopic liver transplantation. Clin Transplant. 2000;14:235-241. |
| 11. | Karakayali H, Boyvat F, Coskun M, Isiklar I, Sozen H, Filik L, Yilmaz U, Gur G, Haberal M. Venous complications after orthotopic liver transplantation. Transplant Proc. 2006;38:604-606. |
| 12. | Pasternak BM, Cohen H. Arteriovenous fistula and forward hypertension in the portal circulation. Angiology. 1978;29:367-373. |
| 13. | Woo DH, Laberge JM, Gordon RL, Wilson MW, Kerlan RK Jr. Management of portal venous complications after liver transplantation. Tech Vasc Interv Radiol. 2007;10:233-239. |