Published online Jun 14, 2008. doi: 10.3748/wjg.14.3583
Revised: April 15, 2008
Accepted: April 22, 2008
Published online: June 14, 2008
Acute complicated diverticulitis, particularly with colon perforation, is a rare but serious condition in transplant recipients with high morbidity and mortality. Neither acute diverticulitis nor colon perforation has been reported in young heart-lung grafted patients. A case of subclinical peritonitis due to perforated acute sigmoid diverticulitis 14 years after heart-lung transplantation is reported. A 26-year-old woman, who received heart-lung transplantation 14 years ago, presented with vague abdominal pain. Physical examination was normal. Blood tests revealed leukocytosis. Abdominal X-ray showed air-fluid levels while CT demonstrated peritonitis due to perforated sigmoid diverticulitis. Sigmoidectomy and end-colostomy (Hartmann’s procedure) were performed. Histopathology confirmed perforated acute sigmoid diverticulitis. The patient was discharged on the 8th postoperative day after an uneventful postoperative course. This is the first report of acute diverticulitis resulting in colon perforation in a young heart-lung transplanted patient. Clinical presentation, even in peritonitis, may be atypical due to the masking effects of immunosuppression. A high index of suspicion, urgent aggressive diagnostic investigation of even vague abdominal symptoms, adjustment of immunosuppression, broad-spectrum antibiotics, and immediate surgical treatment are critical. Moreover, strategies to reduce the risk of this complication should be implemented. Pretransplantation colon screening, prophylactic pretransplantation sigmoid resection in patients with diverticulosis, and elective surgical intervention in patients with nonoperatively treated acute diverticulitis after transplantation deserve consideration and further studies.
- Citation: Markogiannakis H, Konstadoulakis M, Tzertzemelis D, Antonakis P, Gomatos I, Bramis C, Manouras A. Subclinical peritonitis due to perforated sigmoid diverticulitis 14 years after heart-lung transplantation. World J Gastroenterol 2008; 14(22): 3583-3586
- URL: https://www.wjgnet.com/1007-9327/full/v14/i22/3583.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.3583
Abdominal complications are common in solid organ transplant recipients. They include esophagitis, gastritis, duodenitis, hernia, cholelithiasis or diverticulosis with minor morbidity and peptic ulcer disease, choledocholithiasis, acute cholecystitis, acute cholangitis, acute pancreatitis, hepatitis, hepatic or pancreatic abscess, bowel obstruction, megacolon, colitis, perirectal abscess, acute appendicitis, acute diverticulitis, gastrointestinal tract hemorrhage and viscus perforation with significant morbidity and mortality[1–12]. They may occur early after transplantation or even years later[45781012]. Successful management requires a high index of suspicion, early diagnosis and prompt treatment; wherever doubt exists, laparotomy is the appropriate way to establish a definite diagnosis[1–4791012].
Colon perforations may also occur in the early to late post-transplantation period[45912]. Early-onset perforations are secondary to perioperative hypoper-fusion, increased intraluminal pressure from narcotics, use of bowel stimulants, and high-dose immunosuppression while late perforations are often related to acute diverticulitis and invasive fungal or viral colonic disease[45912].
Acute complicated diverticulitis, particularly with colon perforation, is a rare but very serious condition in transplant recipients and remains a challenging surgical problem. Furthermore, neither acute diverticulitis nor colon perforation has been reported until now in heart-lung transplanted young patients. We herein report a case of subclinical peritonitis due to perforated acute sigmoid diverticulitis 14 years after heart-lung transplantation in a 26-year-old woman.
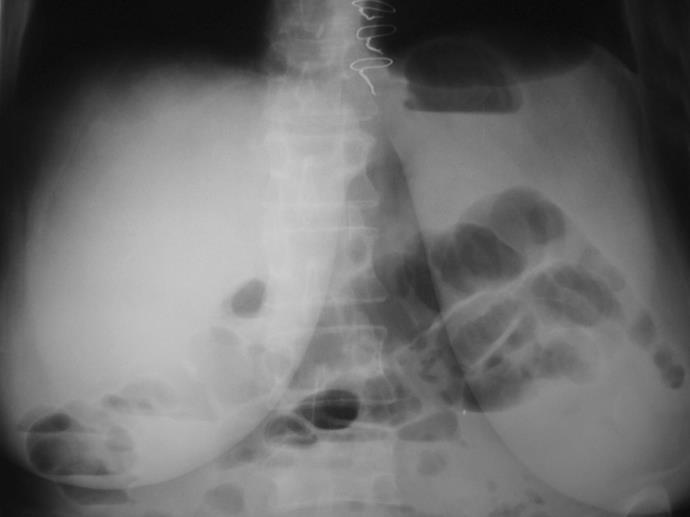
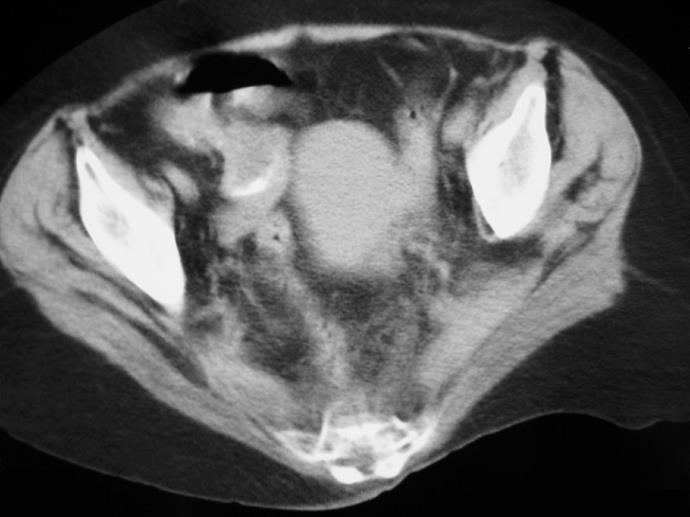
A 26-year-old female patient presented with vague abdominal pain of 24 h duration. The patient received combined heart-lung transplantation because of Eisenmenger’s syndrome 14 years ago. During the post-transplantation period, her medical history was uneventful. She was treated with azathioprine and cyclosporine. On admission, vital signs and physical examination were normal while blood tests revealed leukocytosis (WBC: 19 × 109/L). Upright chest radiography was normal and abdominal X-ray showed air-fluid levels but no free air (Figure 1). Tests were negative for acute cytomegalovirus (CMV) disease. Abdominal computed tomography (CT) scan demonstrated sigmoid colon perforation resulting in peritonitis (Figure 2).
Operative intervention was carried out immediately under broad spectrum antibiotic coverage. Laparotomy revealed diffuse fecal contamination of the abdomen due to perforated sigmoid diverticulitis. Meticulous lavage of the peritoneal cavity, sigmoidectomy and an end-colostomy (Hartmann’s procedure) were performed. Histopathologic examination of the resected specimen confirmed sigmoid colon diverticula, acute diverticulitis, and perforation of one diverticulum. No signs of bacterial, fungal, or viral infection were detected.
The postoperative course was uneventful and the patient was discharged on the 8th postoperative day. The colostomy was closed 6 months later. At a follow-up of 6 months, she is alive with no recurrence of colonic disease.
Abdominal and, particularly, gastrointestinal complications are common in transplanted patients representing an important source of morbidity and mortality[2–4]. They are reported in 6.3%-51% of solid organ transplanted patients with a mortality rate, particularly of major complications, of 7.7%-63%[1–68913–16]. Clinical presentation, even in peritonitis, may be atypical in the immunosuppressed transplant recipient due to the masking effects of the immunosuppression, particularly steroid medication on symptoms and signs[5816]. This may result in delayed presentation and diagnosis or even misdiagnosis[15]. This patient, although not receiving corticosteroids, but azathioprine and cyclosporine, presented with vague abdominal pain and normal abdominal clinical examination despite suffering from peritonitis due to colonic perforation.
The high mortality of gastrointestinal complications appears to be related to the effects of the immuno-suppression and the associated response to sepsis. Reduction of these complications and associated morbidity and mortality can be achieved by improved preventive measures, prompt diagnosis, immediate surgical management, and reduced or steroid-sparing immunosuppressive protocols[129101216]. Increased dosages of maintenance steroid regimens may correlate with the occurrence of gastrointestinal complications[16] while the time interval between onset of symptoms and operative intervention and mean corticosteroid dose are associated with mortality[10].
Asymptomatic diverticulosis has been reported in 39.8% of heart transplanted patients[7]. In a study of renal transplant recipients, the incidence of diverticulosis was 12.7%; major colonic complications eventually developed in 57.1% of these patients resulting in a mortality of 75%[17]. In patients with diverticulosis and a previous history of diverticulitis, consideration for elective segmental colectomy prior to transplantation was, thus, advocated[17]. It is worth mentioning, however, that the presence of colonic diverticula is deemed unlikely in young patients such as this case, and this may lead to late diagnosis. Although uncommon, the presented complication should, therefore be included in the differential diagnosis of young transplanted patients presenting with vague abdominal complaints.
Acute diverticulitis is a relatively rare, but serious problem in transplanted patients[6111215]. It is reported in 0.4%-8% of solid organ transplanted patients with a 0%-83.3% mortality rate[48111618–20]. However, no case of acute diverticulitis in patients with heart-lung transplantation has been reported before, particularly in young patients. Compared to the general population, heart and lung transplant recipients are at substantially increased risk of experiencing acute diverticulitis[1820]. In the study of Qasabian et al, all patients with severe diverticulitis survived and death occurred only in a conservatively treated patient in whom a definite diagnosis was not reached until post-mortem examination was made[18].
Diagnosis of diverticulitis poses a significant challenge in the immunosuppressed patients[111819]. Symptoms and physical examination usually do not reflect the severity of the disease while signs of infection, such as fever and tachycardia, may be absent. Laboratory testing is often unreliable and misleading in estimating the severity of the disease. Abdominal radiographs may be non-specific such as in our patient. Abdominal CT scan is the most reliable modality in determining the location and degree of pathology. A high index of suspicion, prompt diagnosis, reduction of immunosuppression, and early administration of broad spectrum antibiotics are essential for management and prognosis of these patients[1118–20]. If bowel perforation is suspected, immediate operative intervention with bowel resection and colostomy is indicated. In the setting of uncomplicated diverticulitis, it is prudent to proceed with colectomy following resolution of the acute episode, provided the patient is a reasonable operative candidate[1118–20].
Colon perforation has been observed in 0.5%-5.3% of solid organ recipients with a mortality of 0%-100%[13–613–15]. Moreover, colon perforation due to acute diverticulitis is a rare complication with a high mortality[2491012]. It has been described in kidney, heart, and lung transplant recipients[249101214]. Regarding colon perforation due to acute diverticulitis in renal graft recipients, 0.5%-3% have been reported to sustain perforation with a mortality of 12.5%-83.3%[2910]. In heart and lung grafted patients, this incidence is 3.4% and 4.8%-6.7%, respectively, with a mortality of 0%-50%[1216]. However, up to now, there has been no report of colon perforation due to acute diverticulitis in heart-lung transplanted patients.
History of diverticula[2] or acute diverticulitis[10] and steroid therapy[16] have been found to be risk factors for colon perforation. The time between onset of symptoms and operation, intensity of immunosuppression (mean corticosteroid dose), and nutritional status (levels of serum albumin) are associated with the mortality of patients with colon perforation[912]. Immediate diagnosis and early, aggressive care consisting of surgical intervention, broad spectrum antibiotics, and reduced or steroid-sparing immunosuppression are crucial to outcome[81012]. Furthermore, although not uniformly supported in the literature, pretransplantation colon screening and prophylactic sigmoidectomy in patients with diverticulosis, and elective surgical intervention in patients with a nonoperatively treated episode of acute diverticulitis after transplantation have been suggested[11121820].
Even though in the presence of an acute abdomen laparotomy is the appropriate approach to establish a definitive diagnosis and to treat these patients, abdominal operations for urgent surgical conditions are associated with increased morbidity and mortality[412]. Significant reduction of morbidity and mortality can be achieved by prompt diagnosis and early surgical management[12910].
In conclusion, acute complicated diverticulitis, particularly with colon perforation, is a rare but serious condition in transplanted patients with high morbidity and mortality. Our patient is the first case of acute diverticulitis resulting in colon perforation in a young heart-lung graft recipient in the literature. Clinical presentation may be atypical. A high index of suspicion, urgent aggressive diagnostic investigation of even vague abdominal symptoms, adjustment of immunosuppression, adequate selection of antimicrobial agents, and prompt surgical treatment are critical. Strategies to reduce the risk of this complication should also be implemented in transplantation centres; thus, pretransplantation colon screening, prophylactic pretransplantation sigmoidectomy in patients with diverticulosis and elective surgical intervention in patients with a prior episode of acute diverticulitis after transplantation deserve further consideration and studies.
| 1. | Merrell SW, Ames SA, Nelson EW, Renlund DG, Karwande SV, Burton NA, Sullivan JJ, Jones KW, Gay WA Jr. Major abdominal complications following cardiac transplantation. Utah Transplantation Affiliated Hospitals Cardiac Transplant Program. Arch Surg. 1989;124:889-894. |
| 2. | Benoit G, Moukarzel M, Verdelli G, Hiesse C, Buffet C, Bensadoun H, Charpentier B, Jardin A, Fries D. Gastrointestinal complications in renal transplantation. Transpl Int. 1993;6:45-49. |
| 3. | Smith PC, Slaughter MS, Petty MG, Shumway SJ, Kshettry VR, Bolman RM 3rd. Abdominal complications after lung transplantation. J Heart Lung Transplant. 1995;14:44-51. |
| 4. | Maurer JR. The spectrum of colonic complications in a lung transplant population. Ann Transplant. 2000;5:54-57. |
| 5. | Watson CJ, Jamieson NV, Johnston PS, Wreghitt T, Large S, Wallwork J, English TA. Early abdominal complications following heart and heart-lung transplantation. Br J Surg. 1991;78:699-704. |
| 6. | Augustine SM, Yeo CJ, Buchman TG, Achuff SC, Baumgartner WA. Gastrointestinal complications in heart and in heart-lung transplant patients. J Heart Lung Transplant. 1991;10:547-555; discussion 555-556. |
| 7. | Rodriguez-Larrain JM, Ziebert JJ, Kfoury AG, Kuwada S, Taylor DO, Renlund DG. Incidence of adenomatous colorectal polyps in cardiac transplant recipients. Transplantation. 1997;64:528-530. |
| 8. | Lederman ED, Conti DJ, Lempert N, Singh TP, Lee EC. Complicated diverticulitis following renal transplantation. Dis Colon Rectum. 1998;41:613-618. |
| 9. | Stelzner M, Vlahakos DV, Milford EL, Tilney NL. Colonic perforations after renal transplantation. J Am Coll Surg. 1997;184:63-69. |
| 10. | Pirenne J, Lledo-Garcia E, Benedetti E, West M, Hakim NS, Sutherland DE, Gruessner RW, Najarian JS, Matas AJ. Colon perforation after renal transplantation: a single-institution review. Clin Transplant. 1997;11:88-93. |
| 11. | Detry O, Defraigne JO, Meurisse M, Bertrand O, Demoulin JC, Honore P, Jacquet N, Limet R. Acute diverticulitis in heart transplant recipients. Transpl Int. 1996;9:376-379. |
| 12. | Beaver TM, Fullerton DA, Zamora MR, Badesch DB, Weill D, Brown JM, Campbell DN, Grover FL. Colon perforation after lung transplantation. Ann Thorac Surg. 1996;62:839-843. |
| 13. | Owens ML, Wilson SE, Saltzman R, Gordon HE. Gastrointestinal complications after renal transplantation: predictive factors and morbidity. Arch Surg. 1976;111:467-471. |
| 14. | Faro RS, Corry RJ. Management of surgical gastrointestinal complications in renal transplant recipients. Arch Surg. 1979;114:310-312. |
| 15. | Steed DL, Brown B, Reilly JJ, Peitzman AB, Griffith BP, Hardesty RL, Webster MW. General surgical complications in heart and heart-lung transplantation. Surgery. 1985;98:739-745. |
| 16. | Mueller XM, Tevaearai HT, Stumpe F, Hurni M, Ruchat P, Fischer AP, Seydoux C, Goy JJ, von Segesser LK. Gastrointestinal disease following heart transplantation. World J Surg. 1999;23:650-655; discussion 655-656. |
| 17. | Sawyerr OI, Garvin PJ, Codd JE, Graff RJ, Newton WT, Willman VL. Colorectal complications of renal allograft transplantation. Arch Surg. 1978;113:84-86. |
| 18. | Qasabian RA, Meagher AP, Lee R, Dore GJ, Keogh A. Severe diverticulitis after heart, lung, and heart-lung transplantation. J Heart Lung Transplant. 2004;23:845-849. |
| 19. | Khan S, Eppstein AC, Anderson GK, Dengal MK, Eggenberger JC, Lee CS, Szilagy EJ, Margolin DA. Acute diverticulitis in heart- and lung transplant patients. Transpl Int. 2001;14:12-15. |
| 20. | Goldberg HJ, Hertz MI, Ricciardi R, Madoff RD, Baxter NN, Bullard KM. Colon and rectal complications after heart and lung transplantation. J Am Coll Surg. 2006;202:55-61. |