Published online Jun 14, 2008. doi: 10.3748/wjg.14.3579
Revised: March 12, 2008
Accepted: March 19, 2008
Published online: June 14, 2008
AIM: To investigate the clinical value of ultrasonographic diagnosis of biliary atresia (BA), a retrospective analysis of the sonogram of 20 children with BA was undertaken.
METHODS: Ultrasonography (US) was performed in 20 neonates and infants with BA, which was confirmed with cholangiography by operation or abdominoscopy. The presence of triangular cord, the size and echo of liver, the changes in empty stomach gallbladder and postprandial gallbladder were observed and recorded.
RESULTS: The triangular cord could be observed at the porta hepatis (thickness: 0.3-0.6 cm) in 10 cases. Smaller triangular cord (0.2-0.26 cm) can be observed in 3 cases. The gallbladder was not observed in 2 cases, and 1 case showed a streak gallbladder without capsular space. The gallbladders of 15 cases were flat and small. The gallbladders of 2 cases were of normal size and appearance, however, there was no postprandial contraction. The livers of all cases showed hepatomegaly and heterogeneous echogenicity. Statistical analysis was performed to compare the hepatomegaly and heterogeneous echogenicity and the stage of hepatic fibrosis.
CONCLUSION: The presence of the triangular cord at the porta hepatis is specific. However, it is not the only diagnostic criterion, since flat and small gallbladder and poor contraction are also of important diagnostic and differential diagnostic significance. The degree of hepatomegaly and heterogeneous echogenicity is proportional with liver fibrosis, and able to indicate the duration of course and prognosis.
- Citation: Li SX, Zhang Y, Sun M, Shi B, Xu ZY, Huang Y, Mao ZQ. Ultrasonic diagnosis of biliary atresia: A retrospective analysis of 20 patients. World J Gastroenterol 2008; 14(22): 3579-3582
- URL: https://www.wjgnet.com/1007-9327/full/v14/i22/3579.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.3579
Biliary atresia (BA)[1] is a common progressive and obstructive pathological change in the intrahepatic and extrahepatic ducts, often causing immediate cirrhosis and leading to death. Prompt and accurate early diagnosis determines its optimal operation opportunity and therapeutic efficacy. With the updating of ultrasonic apparatus, especially the application of high resolution detecting head, the sonogram becomes increasingly clear, and more doctors have accumulated experience with the ultrasonic diagnosis of BA. However, no general and unitive diagnostic criteria for BA are available at present. The present study was to summarize the manifestations of sonogram for BA, and the clinical diagnostic value of ultrasonography (US) for biliary artresia, in order to provide evidence for its early diagnosis.
Twenty children with BA admitted to our hospital from January, 2004 to March, 2007 were included in this study. The diagnosis of BA was confirmed at operation in 17 children and at abdominoscopy in 3 children. There were 6 males and 14 females at the age of 37-146 d. According to Kasai classification, BA was classified as type I in 1, type II in 3 and type III in 16 children, respectively.
Voluson 730D (Kretz Company) was used. The frequency of transducer for convex and linear array was 3.5-5.5 MHz and 7.5-10 MHz, respectively. The patients were fasted for 3-4 h before examination. Examination was performed with suckling. Sedative was administered to those who kept crying. The patients were examined at a supine position. Oblique section scan under the right rib and multiple cross section scan between ribs were performed to examine liver, gallbladder, and porta hepatis. The transducer was inclined to the right branch of portal vein. Presence of triangular cord, roughness and internal echo of the liver and gallbladder was recorded. Gallbladder at empty stomach and 1, 2 and 3 h postprandial was determined. Changes in size of gallbladder before and after meal were observed dynamically to understand the contractile function of gallbladder. All the sonograms were maintained in the picture archiving and communication system (PACS).
Pearson correlation coefficient was used to determine the correlation of liver size and heterogeneous echogenicity to the liver fibrosis stage.
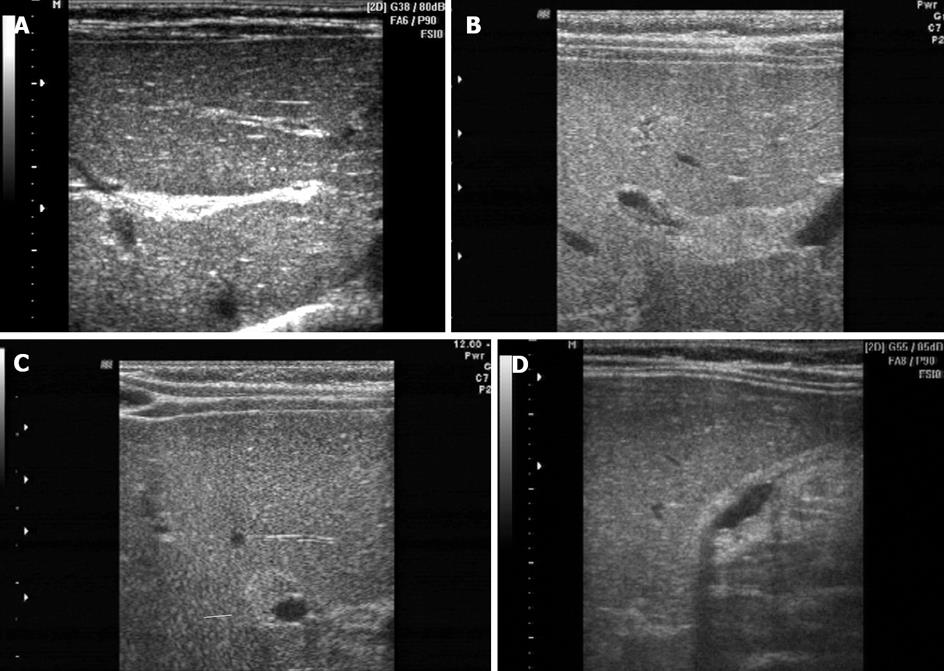
Fourteen out of the 20 BA cases were accurately diagnosed by ultrasound. A triangular cord sign was found at the porta hepatic in 13 cases and an obvious triangular cord was observed in 10 cases. The diameter was about 1.2-2.5 cm and the thickness was about 0.3-0.8 cm. An inverted triangular cord was observed (Figure 1A) and a long streak of the triangular cord was found in 7 cases was (Figure 1B). The triangular cord found in 3 cases too small to be identified in 3 cases. The diameter was about 0.9-1.6 cm, and the thickness was about 0.2-0.26 cm. Cross section scan of the right branch of portal vein showed that the triangular cord sign at the porta hepatis surrounded the right anterior part of the right branch of portal vein, rather than the whole part. In addition, cross section scan of the right branch of portal vein was easier than longitudinal section scan of the triangular cord sign. As shown in Figure 1C, one case of BA had no triangular cord sign at the porta hepatic. Six cases were misdiagnosed due to the absence of triangular cord sign at the porta hepatis.
The manifestations of gallbladder in 20 cases of BA were as follows: (1) absence of gallbladder in 2 cases, (2) vacant and flat gallbladder in 1 case with a streak high echoic area; (3) flat and small gallbladder in 14 cases (Figure 1D), (4) gallbladder with almost a normal size and appearance.
The liver in the 20 BA cases was generally enlarged, and its length under the ribs was 1.8-4.5 cm. Rough parenchyma echo was observed in 7 cases. General echo enhancement and roughness were observed in 13 cases. The degree of hepatomegaly and heterogeneous echogenicity was not related with age, but with the degree of liver fibrosis, suggesting that the size of liver and changes in parenchyma echo could indicate the course and prognosis of BA.
Different diagnostic methods of BA, such as radionuclide-imaging and magnetic resonance cholangio-pancreatography (MRCP), have been reported in the literature[2–5]. However, they have different limitations. It was reported that radionuclide-imaging of liver and gallbladder can give false positive results, since there is a fully obstructive stage due to cholangitis or cholestasis in neonatal hepatitis syndrome and infantile hepatitis syndrome[6–8]. When there is deficient choleresis or the diameter of biliary tract is too small, they would be easily misdiagnosed as BA[9–11]. With the improvement and updating of ultrasonic apparatus, and the enhancement of resolution, clear image can be obtained with a high frequency detecting head. Since the abdominal wall of children is thin, ultrasonic inspection is repeatable, convenient and non-invasive, making it more predominant than other diagnostic methods[1213] for BA.
Some studies demonstrated that the triangular cord at the porta hepatis in BA patients is a direct and specific diadynamic criterion for US, which emphasizes its importance in the diagnosis of BA and significantly increases the accurate rate of BA diagnosis[14–16]. In the present study, 13 cases were diagnosed as BA according to the triangular cord at the porta hepatis. Among them, the triangular cord in 3 cases was relatively small and difficult to identify. The diameter was only 0.2-0.26 cm. However, accurate diagnosis was made based on flat and small gallbladder, irregular shape, poor contraction, enlarged liver and parenchyma echo. Six cases were misdiagnosed due to the absence of the triangular cord. The reasons why the triangular cord is absent are as follows: (1) there is no triangular cord sign at the porta hepatic, (2) the triangular cord is too small to be identified, and (3) the doctor cannot show the triangular cord due to his or her inexperience with US[17–19]. These problems suggest that the triangular cord is not the only diagnostic criterion for BA. We should not ignore some important indirect changes in liver and gallbladder when diagnosing BA[2021]. When the triangular cord at the porta hepatis is relatively small or does not exist, the size and appearance of gallbladder and liver[22], changes in their contractile function[23] and parenchyma echo will help to diagnose BA[2425].
In this study, the triangular cord at the porta hepatis did not surround the whole right branch of portal vein. Cross section scan of the right branch of portal vein showed that the triangular cord adhered tightly to its right anterior area and was easier to show the triangular cord than longitudinal section scan.
In conclusion, the manifestations of sonograms on BA can be summarized as follows. (1) The triangular cord sign at the porta hepatis is one of the direct and specific objective criteria for BA, but not the only one. (2) The manifestations of gallbladder can be classified into four types: absence of gall bladder, vacant and flat gallbladder, flat and small gallbladder, and gallbladder with almost normal size and appearance. (3) The degree of hepatomegaly and heterogeneous echogenicity of liver parenchyma echo are positively correlated to liver fibrosis, which is able to indicate duration and prognosis of BA and provide reliable clinical evidence for choosing operation opportunity.
The present research was to summarize the manifestations of sonogram on biliary atresia (BA), and the clinical diagnostic value of ultrasonography (US) for BA. The presence of triangular cord in the right and left hepatic ducts can become an objective index of the ultrasonic diagnosis of BA. However, it is not the only diagnostic criterion. Flat and small gallbladder and poor contraction are also important for diagnosis and differential diagnosis of BA.
Studies demonstrated that the triangular cord at the porta hepatis in BA patients is a direct and specific criterion for US, which emphasizes its importance in the diagnosis of BA and significantly increases the accurate BA diagnosis rate. It has become an indispensable evidence for the diagnosis of BA.
The triangular cord at the porta hepatis did not surround the whole right branch of portal vein. Cross section scan of the right branch of portal vein revealed that the triangular cord adhered tightly to its right anterior area and was easier to show the triangular cord than longitudinal section scan.
The manifestations of sonogram on BA and the clinical diagnostic value of US for BA can provide strong evidence for its early diagnosis. The presence of triangular cord in the right and left hepatic ducts was specific, and can become an objective index for the ultrasonic diagnosis of BA. However, it was not the only diagnostic criterion. Flat and small gallbladder and poor contraction were also important in the diagnosis and differential diagnosis of BA.
The authors investigated the clinical value of ultrasonographic diagnosis of BA and a retrospective analysis of the sonogram of 20 children with BA was undertaken. The manuscript is very interesting and the study was well designed.
| 1. | Shi WJ, Wang QY, Zhang SD, Fei DK, Gao JT, Wang DZ, Liu GL, Xiao SD, Yin JZ, Zhang CL. Biliary tract surgery. 1st ed. Shanghai: Shanghai Science and Technology Publishing Company 1993; 127. |
| 2. | Norton KI, Glass RB, Kogan D, Lee JS, Emre S, Shneider BL. MR cholangiography in the evaluation of neonatal cholestasis: initial results. Radiology. 2002;222:687-691. |
| 3. | Cox KL, Stadalnik RC, McGahan JP, Sanders K, Cannon RA, Ruebner BH. Hepatobiliary scintigraphy with technetium-99m disofenin in the evaluation of neonatal cholestasis. J Pediatr Gastroenterol Nutr. 1987;6:885-891. |
| 4. | Berdon WE, Condon VR, Currarino G, FItz CR, Leonides JC, Parker B, Slovis T, Wood B. Caffey’s Pediatric X-Ray Diagnosis. St Louis, Missouri: Elsevier Mosby 1993; 1055. |
| 5. | Choi SO, Park WH, Lee HJ, Woo SK. 'Triangular cord': a sonographic finding applicable in the diagnosis of biliary atresia. J Pediatr Surg. 1996;31:363-366. |
| 6. | Kamińska A, Pawlowska J, Jankowska I, Swiatek-Rawa E, Socha P, Kamiński A, Teisseyre M, Czubkowski P, Toth K. Hepatobiliary scanning in the diagnosis of biliary atresia. Med Sci Monit. 2001;7 Suppl 1:110-113. |
| 7. | Ge YB, Xu H, Chen J, Lie RH, Xie JQ, Huang H, Wang D. Diagnostic value of 99mTc-EHIDA liver and gall imaging for congenital biliary atresia. Ji’nan Daxue Xuebao. 2002;23:108. |
| 8. | Duan QJ, Wei GF, Cao QH. Differential diagnosis for infantile hepatitis syndrome and congenital biliary atresia using radionuclide dynamic imaging of liver and gall. Weifang Yixueyuan Xuebao. 1998;20:145. |
| 9. | Jaw TS, Kuo YT, Liu GC, Chen SH, Wang CK. MR cholangiography in the evaluation of neonatal cholestasis. Radiology. 1999;212:249-256. |
| 10. | Guibaud L, Lachaud A, Touraine R, Guibal AL, Pelizzari M, Basset T, Pracros JP. MR cholangiography in neonates and infants: feasibility and preliminary applications. AJR Am J Roentgenol. 1998;170:27-31. |
| 11. | Fan GM, Chen LY, Guo QY, Hou Y, Sun CP. MRI diagnosis for biliary atresia. Zhongguo Yixue Yingxiang Zazhi. 2004;12:244-246. |
| 12. | Carroll BA, Oppenheimer DA, Muller HH. High-frequency real-time ultrasound of the neonatal biliary system. Radiology. 1982;145:437-440. |
| 13. | Lin WY, Lin CC, Changlai SP, Shen YY, Wang SJ. Comparison technetium of Tc-99m disofenin cholescintigraphy with ultrasonography in the differentiation of biliary atresia from other forms of neonatal jaundice. Pediatr Surg Int. 1997;12:30-33. |
| 14. | Kim MJ, Park YN, Han SJ, Yoon CS, Yoo HS, Hwang EH, Chung KS. Biliary atresia in neonates and infants: triangular area of high signal intensity in the porta hepatis at T2-weighted MR cholangiography with US and histopathologic correlation. Radiology. 2000;215:395-401. |
| 15. | Xie YR, Lv MD, Zhang ZD, Li GS, Liu JD. Echo of portal fibrous plaque: reliable diagnostic evidence for infantile biliary atresia. Zhonghua Yixue Chaosheng Zazhi. 1997;13:38-39. |
| 16. | Park WH, Choi SO, Lee HJ, Kim SP, Zeon SK, Lee SL. A new diagnostic approach to biliary atresia with emphasis on the ultrasonographic triangular cord sign: comparison of ultrasonography, hepatobiliary scintigraphy, and liver needle biopsy in the evaluation of infantile cholestasis. J Pediatr Surg. 1997;32:1555-1559. |
| 17. | Azuma T, Nakamura T, Nakahira M, Harumoto K, Nakaoka T, Moriuchi T. Pre-operative ultrasonographic diagnosis of biliary atresia--with reference to the presence or absence of the extrahepatic bile duct. Pediatr Surg Int. 2003;19:475-477. |
| 18. | Ma JD, Zhang YL, Ma RB, Yao SQ. Type-B ultrasonic diagnosis and clinical validation for biliary atresia. Zhongguo Chaosheng Yixue Zazhi. 1996;12:38-40. |
| 19. | Tan Kendrick AP, Phua KB, Ooi BC, Subramaniam R, Tan CE, Goh AS. Making the diagnosis of biliary atresia using the triangular cord sign and gallbladder length. Pediatr Radiol. 2000;30:69-73. |
| 20. | Tan Kendrick AP, Phua KB, Ooi BC, Tan CE. Biliary atresia: making the diagnosis by the gallbladder ghost triad. Pediatr Radiol. 2003;33:311-315. |
| 21. | Huang ZH, Yue GR, Dong YT. The differential diagnostic significance of ultrasonic inspection on gallbladder and duodenal juice draining examination for infantile jaundice. Zhonghua Yixue Zazhi. 2004;28:134-136. |
| 22. | Huang YJ, Huang ZH, Yue GR, Dong YS, Wang G. The diagnostic value of ultrasonic inspection on changes of gallbladder size before and after breast-feeding for infantile hepatitis syndrome and biliary atresia. Guang dong Yixue. 2004;25:39-40. |
| 23. | Park WH, Choi SO, Lee HJ. The ultrasonographic 'triangular cord' coupled with gallbladder images in the diagnostic prediction of biliary atresia from infantile intrahepatic cholestasis. J Pediatr Surg. 1999;34:1706-1710. |
| 24. | Bates MD, Bucuvalas JC, Alonso MH, Ryckman FC. Biliary atresia: pathogenesis and treatment. Semin Liver Dis. 1998;18:281-293. |