INTRODUCTION
Trichinosis is a parasitic disease of mammals caused by the nematode parasite Trichinella spp. It is an important zoonotic infection caused by humans eating raw or inadequately cooked meat of infected animals. Infection is most common in omnivores (horses, humans, pigs and rats) and carnivores (cats, dogs, and seals), and pigs and rodents play an important role in the epidemiology of the disease. The main source of infection in Thailand has been pigs, but wild boar, jackal and black bear have also been identified as sources of trichinosis[1]. Unlike other parasitic infections, trichinosis has been a major public health problem in Asia, including Korea and Thailand[2–4].
Since 1962, more than 7300 infections and 97 deaths have occurred in Thailand in 135 outbreaks (morbidity rate 0.04 per 100 000 people); however, this figure may underestimate the actual number of cases[4]. Until recently, T. spiralis, T. pseudospiralis and T. papuae were the only human-infecting species in Thailand. T. spiralis was the causative agent of most early outbreaks of trichinosis[5]. More recently, T. pseudospiralis and T. papuae infections in some areas of Thailand have been reported[67]. The first outbreak of trichinosis in Thailand in 1962 involved 56 patients and resulted in 11 deaths in the Mae Sariang District, Mae Hong Son Province[5]. The highest annual number of hospital recorded trichinosis cases recorded in Thailand was 557 in 1983. Historically, most infections result from consumption of raw pork in the form of “lahb” and “nahm,” favorite dishes of north, Thailand[8]. The incidence of T. spiralis larvae in dog meat in the areas favoring dog meat consumption is a major public health problem in the future, the popular food of people in the northeast area. Srikitjakarn et al reported T. spiralis was found in 1.67% of 421 samples of dog meat in Tarae District, Sakonnakon Province[9]. Raw dog meat was a source of infection in Kaeng Khlo District, Chaiyaphum Province in December 1984[10].
From the past to present, trichinosis is still reported every year in Thailand; therefore, this article reviews the literature on the distribution, prevalence and cause of trichinosis in Thailand, including the annual epidemiological surveillance, a report by the Bureau of Epidemiology, Department of Disease Control, Ministry of Public Health, Thailand, 1971-2006. Morbidity is described by year, month of the year, age group, region and province.
REPORT CASES OF TRICHINOSIS PER 100 000 PER CAPITA BY YEAR, THAILAND
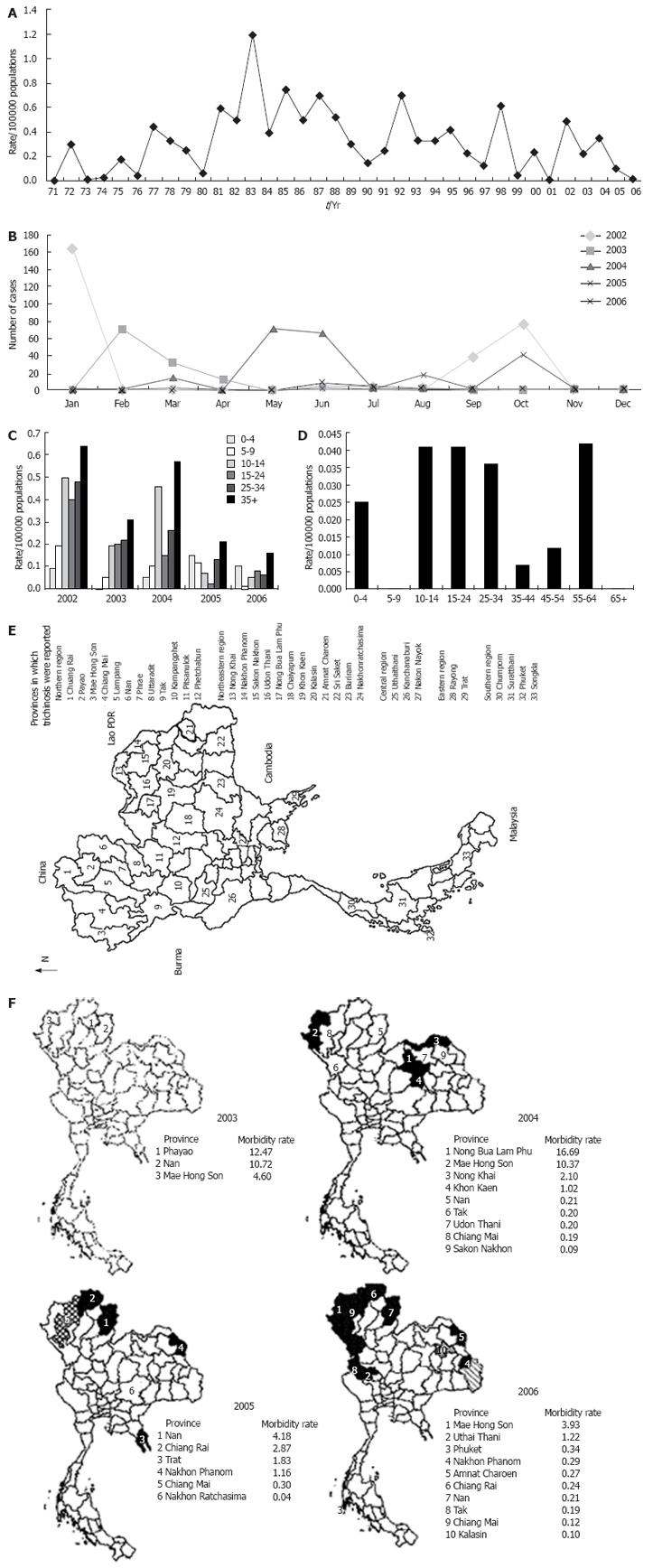
The first outbreak of trichinosis in Thailand, in 1962, involved 56 patients resulting in 11 deaths[5]. In an April 1973 outbreak, 31 persons were involved, ranging from 9 to 72 years, and one adult female died[8]. In 1980, trichinosis was reported, the infection being caused by the consumption of wild squirrel[11]. An epidemic of trichinosis involving 177 patients and 13 deaths occurred in 1981[12]. The highest annual number of hospital recorded trichinosis cases was 557 in 1983[13]. This figure is considered an underestimation of the actual number of cases involved in the outbreaks. Khambooruang reported 118 discrete outbreaks of the disease involving 5400 patients and 95 deaths[14]. In 8 cases of childhood trichinosis reported[15]. An outbreak of trichinosis affecting 59 individuals resulting in one death occurred in during 1994-1995. This was the first report of an epidemic of human infection caused by T. pseudospiralis[6]. Takahashi et al (2000) reported 120 outbreaks from 1962 to 2000 involving nearly 6700 patients and 97 deaths[16]. Chotmongkol et al presented the progressive generalized muscle hypertrophy weakness for 3 mo with the 49-year-old man who infected with T. spiralis[17]. More than 7300 infections with 97 deaths occurred in about 130 outbreaks, since 1962[18]. Recently, T. papuae was identified as the etiological agent of trichinosis involving 19 people after eating raw wild pig[13]. More than 5 outbreaks were reported by the Bureau of Epidemiology, Department of Disease Control, Ministry of Public Health, Thailand. Reported morbidity rate of trichinosis cases increased from 0.04 in 1997 to 0.57 in 1998. In 1999 and 2000, the number of reported morbidity rate decreased to 0.03 and 0.21 respectively. No cases were recorded in 2001, but then 0.46, 0.20 and 0.34 occurred in 2002, 2003 and 2004, respectively. In 2005 and 2006, 0.12 and 0.03 of morbidity rates were reported by the Bureau of Epidemiology, Department of Disease Control, Ministry of Public Health (Figure 1A). Morbidity rate of trichinosis cases during 1997, 1998, 1999, 2000, 2001, 2002, 2003, 2004, 2005 and 2006 were 61, 351, 16, 128, 0, 289, 126, 154, 73 and 19, respectively. More than 135 outbreaks have been reported totaling 7340 patients and 97 deaths. Most of cases were classified by occupation and place of treatment were agriculture and community hospital[18].
Figure 1 Reported cases of trichinosis in Thailand.
A: Morbidity rate (per 100 000 populations) of trichinosis cases was reported by the Bureau of Epidemiology, Department of Disease Control, Ministry of Public Health, 1971-2006; B: Reported by month, 2002-2006; C: Reported per 100 000 populations by age-group, 2000-2006; D: Reported per 100 000 populations by age-group, 2006; E: Distribution by region during 1962-2006; F: Reported per 100 000 populations by Province, 2004-2006.
REPORT CASES OF TRICHINOSIS BY MONTH, THAILAND
The distribution of trichinosis was reported by month from 1962 and 2006, more frequently during October to January. Cases were reported most frequently in months during communal feasts celebrating the Thai New Year, though few of them have been documented. During 2002 to 2006, the number of reported trichinosis cases differed from previously recorded reports. In 2002, the highest of number of trichinosis cases was reported in January. The number of cases was decreased in 2003 overall, and February had the highest of reported trichinosis cases. In 2004, May and June were the months with the highest trichinosis cases, and in 2005, October was the highest trichinosis report month. The most recent data from 2006 shows that June is the month with the highest number of trichinosis cases (Figure 1B)[18].
REPORT CASES OF TRICHINOSIS PER 100 000 PER CAPITA BY AGE GROUP
Previous research demonstrates variability in reports of trichinosis by age-group. Of 31 persons in an outbreak of trichinosis occurred in Chiang Rai Province, ranging from 9 to 72 years, one adult female died[8]. In Thailand, 8 cases of childhood trichinosis were reported in several studies[15]. Charkrit reported the youngest patient was about 1 year old[19]. Chotmongkol et al presented the progressive generalized muscle hypertrophy and weakness over a three-month period in a 49-year-old man infected with T. spiralis[17]. Kaewpitoon et al have reported that trichinosis cases are common in the 35-44 groups[4]. Since 2002, the distribution of human trichinosis cases by age groups has been collected by the annual epidemiological surveillance reports. Most patients are in the 35-44 groups, and many are over the age of 65. In 2002 and 2005, trichinosis cases were most frequently reported in the 35-44 groups, and this figure is very similar to previously reported research[417]. In 2006, the cases reported by the annual epidemiological surveillance varied considerably from reports of the past. Most, 66.67% patients were 15 to 44 years old. The youngest and oldest patients were 4 and 62 years old (Figure 1C). Reported cases of trichinosis per 100 000 people by age group in 2006, were similarly (0.036-0.042) across five age-groups as, that is, 10-14, 15-24, 25-34, 35-44 and 55-64 years old (Figure 1D). Infection occurs in men and women at the ratio of 1.7:1, 1:1.03, 1:1 and 1:1 in 2003, 2004, 2005 and 2006, respectively[18].
REPORT CASES OF TRICHINOSIS BY REGION, THAILAND
Trichinosis is more common in temperate than in tropical regions. The epidemiological surveillance reports of trichinosis have been conducted almost every year and data investigations reveal that outbreaks have occurred predominantly in rural areas. The annual epidemiological surveillance reports from 1962 to 2006 found consistently high numbers of cases in the north region. The north part of Thailand is responsible for 77.94% of all cases reported from 2002 to 2006. The northeast region was responsible for 21.61% of cases in 2004. In 2004, there were 124 reported cases in the northeast, representing the first time that a region other than the north had the highest number of cases. These results showed that trichinosis is a serious problem, particularly in the north and northeast regions of Thailand. Only small numbers of trichinosis cases were recorded in the central and south regions in 2005. The numbers of cases in other parts of Thailand were very few. In the central region, the infection rate was 0.3% of the total number of cases; the south region accounted for only 0.15% of cases. In 2006, most reported cases occurred in the north region (Figure 1E)[18].
REPORT CASES OF TRICHINOSIS PER 100 000 PEOPLE, BY PROVINCE
Most outbreaks that occurred during 1962 to 2006 were located in the north region. The most severely affected areas in the north region were the highland provinces of Chiang Rai, Nan, Chiang Mai, Mae Hong, Son Payao, Lampang, Phrae, Uttaradit, Pitsanuloke, Phetchabun, Tak and Kamphangphet[81219–21]. The first outbreak of trichinosis occurred in the Mae Sariang District, Mae Hong Son Province[5]. The second outbreak was in 1963 at Prao District, Chiang Mai Province. In April 1973, an outbreak of trichinosis occurred in Mae Sruay District, Chiang Rai Province. 31 persons were involved, and 1 adult female died. All trichinosis cases included a history of having consumed raw pork in the form of “lahb” and “nahm,” favorite dishes of north Thailand[8]. An epidemic of trichinosis involving 177 patients resulted in 13 deaths in Kok-Ta-Back Village, Nong-Pai District, Petchabun Province[12]. Takahashi et al (2000) reported 120 outbreaks from 1962 to 2000 involving nearly 6700 patients and 97 deaths. The highest numbers of cases were in Chiang Mai, Chiang Rai and Nan provinces, 1776, 1739 and 894 respectively. The numbers of cases in other parts of Thailand were very few. The northeast region was responsible for the highest number of cases in some years mainly in 2004. Provinces involved were Non Bua Lam Phu, Nong Khai, Udon Thani, Sakon Nakhon, Nakon Phanom, Amnat Charoen, Kalasin, Khon kaen, Chaiyapum, Nakhonratchasima, Buriram and Sri Saket. In the central region, Uthaithani, Kanchanaburi, Nakon Nayok, Rayong and Trat provinces have been reported the number of trichinosis cases. In 1994, in the south of Thailand, an outbreak of trichinosis affecting 59 individuals resulted in 1 death in Chumporn Province. This was the first report of an epidemic of human infection caused by T. pseudospiralis[6]. At this time, Chumphon, Suratthani, Songkla and Phuket were the only provinces of the south region in which cases of trichinosis were observed. This is interesting because Phuket province is a popular destination for Thai and foreigner travelers.
The reported cases of trichinosis per 100 000 populations by province during 2003 to 2006 were classified by the bureau of the Epidemiology, Department of Disease Control, Ministry of Public Health, Thailand. In 2003, most trichinosis cases were reported from Payao, Nan and Mae Hong Son province, morbidity rate were 12.47, 10.72 and 4.60, respectively. The provinces with the highest rates of trichinosis cases in 2004 were Nong Bua Lam Phu, Mae Hong Son, Nong Khai, Khon Kaen, Nan, Tak, Udon Thani, Chiang Mai and Sakon Nakhon, 16.69, 10.37, 2.10, 1.02, 0.21, 0.20, 0.20, 0.19 and 0.09, respectively. Meanwhile, 2005 was comprised 6 provinces have been shown that the highest morbidity rate were Nan, Chiang Rai, Trat, Nakhon Phanom, Chiang Mai and Nakhon Ratchasima as 4.18 2.87 1.83 1.16 0.30 and 0.04, respectively. Recent, Mae Hong Son, Uthai Thani, Phuket, Nakhon Phanom, Amnat Charoen, Chiang Rai, Nan, Tak, Chiang Mai and Kalasin as 3.93, 1.22, 0.34, 0.29, 0.27, 0.24, 0.21, 0.19, 0.12 and 0.10, were the top ten leading rate of trichinosis cases in 2006 (Figure 1F)[18].
CONCLUSION
Studies of trichinosis in Thailand, since the first recorded outbreak in 1962 until 2006, show that most outbreaks occurred in the north of the country, an area in which popular, traditional dishes involve meat from pigs and wild boars, often eaten raw or under-cooked. Overall, more than 135 outbreaks have been reported during 1962-2006 involving 7340 patients and 97 deaths. Trichinosis is still a serious problem food-borne parasitic zoonoses in Thailand. No vaccines have been developed. Treatment exists for Trichinosis in humans if diagnosed promptly. Better prevention and control of trichinosis requires health education programs to improve the knowledge, attitude and behavior of people in the high-risk areas.
Peer reviewer: Yasuji Arase, MD, Department of Gastroenterology, Toranomon Hospital, 2-2-2 Toranomonminato-ku,
Tokyo 105-8470, Japan