Published online May 14, 2008. doi: 10.3748/wjg.14.2939
Revised: March 8, 2008
Published online: May 14, 2008
A 10-year-old Chinese boy who had a history of congenital thrombocytopathy presented with severe iron deficiency anemia secondary to chronic gastric inflammation and duodenal ulcerations. Subtle oculocutaneous albinism led to the finding of diminished dense bodies in the platelets under electron microscopy, hence the diagnosis of Hermansky-Pudlak syndrome (HPS). Biopsies from the stomach and duodenum revealed a lymphocytic infiltration in the submucosa, but H pylori infection was absent. The gastroduodenitis responded to the treatment with omeprazole while iron deficiency anemia was corrected by oral iron therapy. HPS is a rare cause of congenital bleeding disorder with multisystemic manifestations. Upper gastrointestinal involvement is rare and should be distinguished from a mere manifestation of the bleeding diathesis.
- Citation: Lee ACW, Poon KH, Lo WH, Wong LG. Chronic ulcerative gastroduodenitis as a first gastrointestinal manifestation of Hermansky-Pudlak syndrome in a 10-year-old child. World J Gastroenterol 2008; 14(18): 2939-2941
- URL: https://www.wjgnet.com/1007-9327/full/v14/i18/2939.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.2939
Hermansky-Pudlak syndrome (HPS) is a rare form of congenital platelet disorder, affecting 1 in 500 000-1 000 000 populations of different ethnicity[1]. A high prevalence is seen in northern Puerto Rico where 1 per 1800 people is affected. It is inherited as an autosomal recessive disorder of intracytoplasmic organelle-specific protein biosynthesis and trafficking[2]. Eight subtypes with known genetic mutations have been described[13–7]. The disease is characterized by oculocutaneous albinism and bleeding diathesis due to platelet storage pool deficiency. Colitis is an important bowel complication in patients with HPS[8]. Involvement of the upper gastrointestinal tract has not been reported and can be potentially confused with thrombocytopathic bleeding. Our successful diagnosis and management under such circumstances is reported below.
The patient first presented at 5 years of age with a longstanding history of easy bruising and recurrent epistaxis. Both parents were of Chinese origin and unrelated. There was no history of bleeding into muscles, joints or the gastrointestinal tract. He had occasional mild eczema but no recurrent infections. Initial physical examination was remarkable only for multiple bruises of varying ages on his legs. The first laboratory investigations revealed mild thrombocytopenia (platelet counts, 118 and 84 × 109/L on two occasions) with normal platelet volume and morphology under light microscopy. A microcytic, hypochromic anemia (Hb, 10.4 g/dL) due to β-thalassemia trait was also found. The coagulation screen was normal.
Four months later, he had a scalp laceration after a minor fall at home. The wound was sutured but he was re-admitted a few hours later because of progressive wound swelling. An excessive scalp hematoma was found but intracranial bleeding was excluded on computer tomography (CT) scan. The total blood counts were remarkable with Hb 9.3 g/dL and platelets 91 × 109/L. A prolonged bleeding time of 13 min was then documented. Platelet function studies showed a diminished response to collagen and no response to arachidonic acid while response to adenosine diphosphate (ADP), adrenaline, ristocetin and calcium ionophore was normal. The findings were suggestive, but not typical, of storage pool deficiency.
The child has had only mild bleeding manifestations since then with cutaneous bruises and epistaxis. None of them required any hemostatic control other than local pressure. His skin color was paler compared with other children but the color of his hair and iris was not noticeably different. His mother recalled that he had once developed severe sunburn with skin blistering after having fun on the beach and he would never tan under the sun.
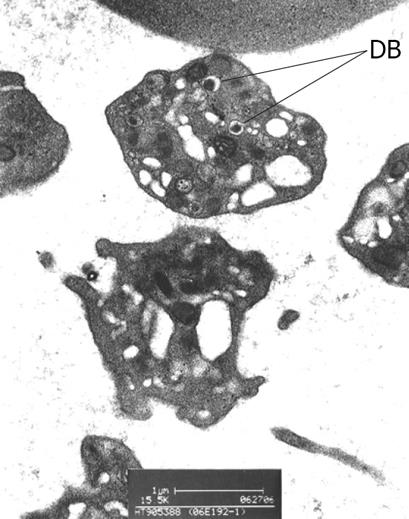
He presented at 10 years of age again because of a 3-mo history of recurrent severe epigastric pain, nausea and vomiting. There was no diarrhea, overt gastrointestinal bleeding or joint pain. He had lost 2.2 kg over the course of the illness. The blood counts showed Hb 5.9 g/dL and platelet 237 × 109/L. Serum biochemistries including hepatic transaminases and amylase were normal except for diminished ferritin level (30 pmol/L, normal 67-896). Tests for C-reactive protein, erythrocyte sedimentation rate (ESR), anti-nuclear antibody, serum IgE, C3 and C4 were all normal. Bacterial, viral and parasitic studies of the stool were negative, while occult blood was found. C13-urea breath test was negative. An ophthalmological consultation revealed diminished pigmentations in the iris and retina. Electron microscopy showed that dense bodies were diminished in some platelets and were absent in other platelets (Figure 1). The diagnosis of HPS was therefore made.
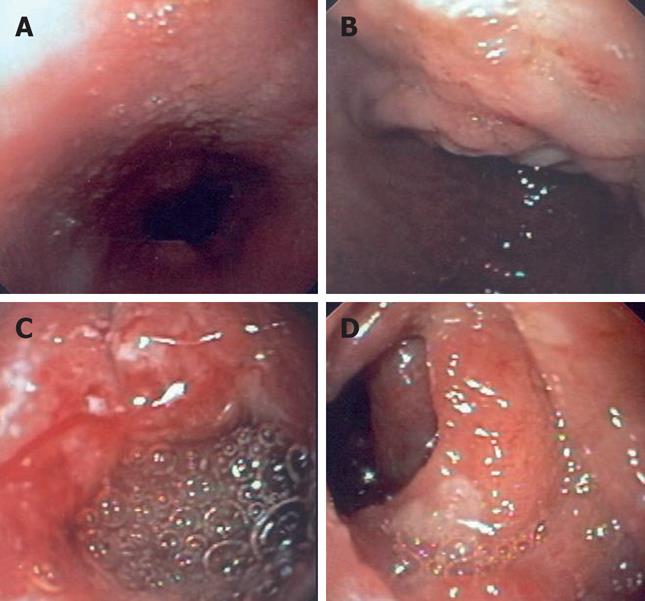
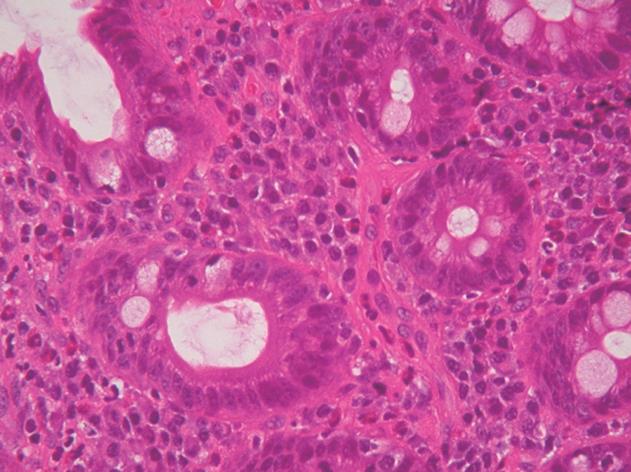
On esophagogastroduodenoscopy, scattered areas of inflammatory changes were noted in the esophagus and stomach. Mucosal ulcerations were noted in the first and second parts of the duodenum (Figure 2A-D). Biopsies taken from the stomach and the duodenum showed a mixed chronic infiltration with lymphocytes, plasma cells and some eosinophils in the lamina propria consistent with inactive chronic gastritis and non-specific duodenitis, respectively (Figure 3). H pylori-like organism and intracellular ceroid-lipofuscin inclusions were not found.
The child was treated with omeprazole 20 mg (0.8 mg/kg) daily and iron (elemental iron 6 mg/kg per day) orally. He also received counseling on protection from solar damage with respect to his visual and dermatological vulnerabilities. Reassessment 5 wk later showed complete remission of epigastric pain, near total correction of anemia, complete ulcer healing and marked improvement in the gastric and duodenal inflammation on endoscopic and histologic examination. Omeprazole was given for 4 mo until his premorbid body weight and hemoglobin levels were restored. A normal fasting serum level of gastrin (16 pmol/L, normal < 55) obtained after cessation of omeprazole excluded hypergastrinemia.
However, two weeks after stopping omeprazole, the clinical symptoms and endoscopic signs of gastroduodenitis recurred. Although a full gastrointestinal workup was declined, the child responded again to omeprazole treatment, which would be given for long term acid suppression.
Although the combination of oculocutaneous albinism and platelet function disorder has only been described in HPS[910], the definitive diagnosis was delayed in this patient. This was in part due to the subtleness of the hypopigmentation and the fact that the condition has not been previously reported in Hong Kong. Nevertheless, the emergence of an unusual complication during the course of the child’s illness prompted to a re-evaluation, thus establishing the diagnosis of HPS. It is interesting that our case experienced marked upper gastrointestinal inflammation in association with his rare inherited disorder.
In addition to bleeding tendency, visual and cutaneous problems, patients with HPS may be complicated by diseases of the lungs, the gastrointestinal tract, the heart, and the kidneys[111]. Chronic neutropenia with recurrent infections have been reported in a few children with type 2 HPS[12]. Progressive pulmonary fibrosis, appearing during the fourth decade of life, is the most important cause of early mortality among patients with HPS[113]. It primarily affects individuals with types 1 and 4 HPS.
Gastrointestinal complications are an important manifestation in patients with HPS. Granulomatous colitis is the most frequently reported feature and may affect 10%-20% of patients with HPS[114]. The mean age at presentation is 15 years and about 15% of patients may present with severe inflammatory lesions. Granulomatous colitis may resemble Crohn’s disease both clinically and histologically. The clinical features include signs and symptoms of inflammatory bowel disease like abdominal pain, bloody diarrhea, symptoms of bowel constriction, and perianal fistula[15]. Microscopically, the bowel shows areas of hyperemia and denuded epithelium with non-necrotizing granulomas. Ceroid deposits may be identified in the intestinal lesions but they may be absent even with severe disease[8]. Management of granulomatous colitis in HPS is also similar to Crohn’s disease and consists of immunomodulatory therapy. Total colectomy has been required in a few patients with severe illness[1814].
Extra-colonic involvement of the gastrointestinal tract in HPS is unusual[8] and the clinical features and specific management have not been characterized. In the present case, the patient’s clinical manifestations were similar to peptic ulceration except that H pylori infection was absent and rapid relapse followed cessation of therapy with proton-pump inhibitor. Treatment with a proton-pump inhibitor was found to be satisfactory, but the optimal duration of treatment was not known.
In summary, HPS is an unusual cause but an important differential diagnosis of upper gastrointestinal inflammatory disease in children. Endoscopic evaluation is a safe and helpful adjunct in the diagnosis, but the optimal long-term management and outcomes of the gastrointestinal disease are unknown.
| 1. | Gahl WA; Gene reviews: Hermansky-Pudlak syndrome. Last update on November 27, 2007. Available from: URL: http://www.geneclinics.org/profiles/hps/details.html. |
| 2. | Di Pietro SM, Dell'Angelica EC. The cell biology of Hermansky-Pudlak syndrome: recent advances. Traffic. 2005;6:525-533. |
| 3. | Hermos CR, Huizing M, Kaiser-Kupfer MI, Gahl WA. Hermansky-Pudlak syndrome type 1: gene organization, novel mutations, and clinical-molecular review of non-Puerto Rican cases. Hum Mutat. 2002;20:482. |
| 4. | Anderson PD, Huizing M, Claassen DA, White J, Gahl WA. Hermansky-Pudlak syndrome type 4 (HPS-4): clinical and molecular characteristics. Hum Genet. 2003;113:10-17. |
| 5. | Huizing M, Hess R, Dorward H, Claassen DA, Helip-Wooley A, Kleta R, Kaiser-Kupfer MI, White JG, Gahl WA. Cellular, molecular and clinical characterization of patients with Hermansky-Pudlak syndrome type 5. Traffic. 2004;5:711-722. |
| 6. | Li W, Zhang Q, Oiso N, Novak EK, Gautam R, O'Brien EP, Tinsley CL, Blake DJ, Spritz RA, Copeland NG. Hermansky-Pudlak syndrome type 7 (HPS-7) results from mutant dysbindin, a member of the biogenesis of lysosome-related organelles complex 1 (BLOC-1). Nat Genet. 2003;35:84-89. |
| 7. | Morgan NV, Pasha S, Johnson CA, Ainsworth JR, Eady RA, Dawood B, McKeown C, Trembath RC, Wilde J, Watson SP. A germline mutation in BLOC1S3/reduced pigmentation causes a novel variant of Hermansky-Pudlak syndrome (HPS8). Am J Hum Genet. 2006;78:160-166. |
| 8. | de Leusse A, Dupuy E, Huizing M, Danel C, Meyer G, Jian R, Marteau P. Ileal Crohn's disease in a woman with Hermansky-Pudlak syndrome. Gastroenterol Clin Biol. 2006;30:621-624. |
| 9. | Hermansky F, Pudlak P. Albinism associated with hemorrhagic diathesis and unusual pigmented reticular cells in the bone marrow: report of two cases with histochemical studies. Blood. 1959;14:162-169. |
| 10. | Scheinfeld NS. Syndromic albinism: a review of genetics and phenotypes. Dermatol Online J. 2003;9:5. |
| 11. | Wei ML. Hermansky-Pudlak syndrome: a disease of protein trafficking and organelle function. Pigment Cell Res. 2006;19:19-42. |
| 12. | Huizing M, Gahl WA. Disorders of vesicles of lysosomal lineage: the Hermansky-Pudlak syndromes. Curr Mol Med. 2002;2:451-467. |
| 13. | Sandberg-Gertzen H, Eid R, Jarnerot G. Hermansky-Pudlak syndrome with colitis and pulmonary fibrosis. Scand J Gastroenterol. 1999;34:1055-1056. |
| 14. | Schinella RA, Greco MA, Cobert BL, Denmark LW, Cox RP. Hermansky-Pudlak syndrome with granulomatous colitis. Ann Intern Med. 1980;92:20-23. |
| 15. | Goswami GK, Sadler MA, Siegel S. Small-bowel stricture in a woman with oculocutaneous albinism (Hermansky-Pudlak syndrome). AJR Am J Roentgenol. 2000;174:1163-1164. |