Published online May 7, 2008. doi: 10.3748/wjg.14.2763
Revised: February 15, 2008
Published online: May 7, 2008
AIM: To identify patients with persistent acute diverticulitis who might benefit from an early colonoscopy during their first hospitalization.
METHODS: All patients hospitalized between July 2000 and December 2006 for acute diverticulitis who underwent colonoscopy were included in the study. Patients were followed during hospitalization and after discharge. Patients were considered to have a persistent course of acute diverticulitis if symptoms continued after 1 wk of conventional treatment with IV antibiotics, or if symptoms recurred within 2 mo after discharge. Patients were considered to benefit from an early colonoscopy if the colonoscopy was therapeutic or if it changed a patient's outcome.
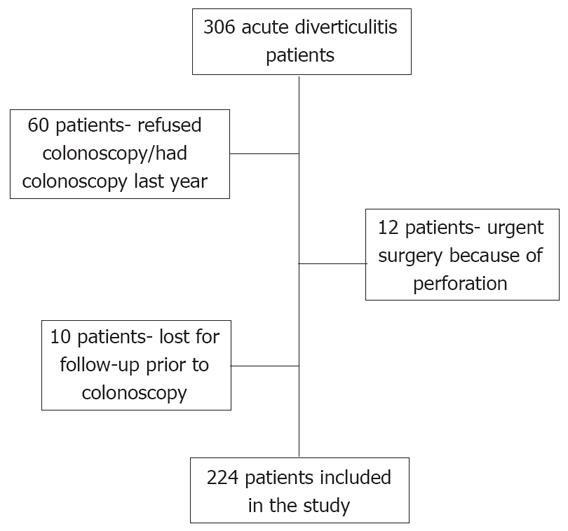
RESULTS: Three hundred and six patients were hospitalized between July 2000 and December 2006 with the diagnosis of acute diverticulitis. Two hundred and twenty four of these were included in the study group. Twenty three patients (10.3%) fulfilled the criteria for a persistent course of acute diverticulitis. Of them, four patients (17.4%) clearly benefited from an early colonoscopy; these patients’ clinical course is described. None of the patients with a regular non-persistent course demonstrated any benefit from colonoscopy.
CONCLUSION: Early colonoscopy detected other significant pathology, which accounted for the clinical presentation in 17% of patients with persistent acute diverticulitis. Therefore, we believe an early colonoscopy should be considered in all patients with a persistent clinical course.
- Citation: Lahat A, Yanai H, Sakhnini E, Menachem Y, Bar-Meir S. Role of colonoscopy in patients with persistent acute diverticulitis. World J Gastroenterol 2008; 14(17): 2763-2766
- URL: https://www.wjgnet.com/1007-9327/full/v14/i17/2763.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.2763
Diverticular disease of the colon is a common condition in Western societies. The incidence rises with age. By the age of 85 two thirds of the population in developed countries will have developed colonic diverticula[12]. Most patients will remain asymptomatic. Only a minority will have complications. The most common complication is acute diverticulitis which occurs in 10%-25% of patients[2–6]. In most patients, the disease is mild, responds well to antibiotic therapy and does not recur[7]. However, there are patients who suffer from a persistent disease course. This relatively small group of patients does not respond well to conventional therapy, usually suffers from longer disease duration and might experience recurrent exacerbations. These patients often require a more aggressive therapeutic approach.
Colonoscopy is advised after an attack of acute diverticulitis in order to completely evaluate the colonic lumen and exclude a potential malignancy. However, it is a common practice to postpone colonoscopy until symptoms have fully subsided and perform it at least six wk after discharge, in order to avoid the potential risk of converting a sealed perforation into a free perforation[8–12].
In two previous studies, we have shown that performing an early colonoscopy during hospitalization for acute diverticulitis is feasible and safe[1314]. Early in-hospital colonoscopy was associated with better patient compliance, but a lower rate of cecal intubation. Patients with persistent diverticulitis seemed to benefit most from having early colonoscopy. The aim of this study was, therefore, to assess the yield of performing an early colonoscopy on patients with persistent acute diverticulitis, and to try to identify the subgroup of patients with persistent acute diverticulitis who might benefit from an early colonoscopy during their first hospitalization.
All patients who were hospitalized between July 2000 and December 2006 for acute lower abdominal pain, fever above 38°C and leukocytosis above 12 000, and who were suspected of having acute diverticulitis, were prospectively studied. All patients underwent abdominal CT and only those with CT findings compatible with acute diverticulitis were included in the study group. CT criteria for acute diverticulitis included the presence of colonic diverticuli, thickening of the colonic wall at the site of the diverticuli and peri-colic fat infiltration.
During hospitalization, patients were treated with IV antibiotics suitable to cover abdominal flora (usually ampicillin and garamycin) at the appropriate dosages.
Patients were considered to have a persistent course of acute diverticulitis if symptoms continued after 1 wk of conventional treatment with IV antibiotics, or if symptoms recurred within 1 mo after discharge.
All patients enrolled in the study underwent colonoscopy. Early colonoscopy was defined as colonoscopy performed during hospitalization on symptomatic patients or within 6 wk of the initial presentation. Late colonoscopy was defined as when the procedure was performed at least 6 wk after discharge, and when the patient was asymptomatic. The timing of the colonoscopy was based upon randomization protocols, as described in our previous two studies[1314].
All patients were closely followed during hospitalization and after discharge. Their follow-up after discharge was done by regular phone calls, conducted by the study coordinator as to their well being.
Patients enrolled in this study belong to a database of patients with acute diverticulitis. This database was used in our previous publications as well[13–15].
Patients were considered to benefit from an early colonoscopy if the colonoscopy was therapeutic or if it changed the patient’s outcome. Excluded from the study group were patients who refused to undergo colonoscopy (either early or late), patients with a history of colonoscopy within one year prior to the current episode of acute diverticulitis, patients operated on due to colonic perforation and patients lost to follow-up. The study was approved by the local ethics committee.
Patients’ characteristics were analyzed by the χ2 test with Yates correction. Statistical analyses were conducted by using Statsoft software (Tulsa, OK, USA).
Three hundred and six patients were hospitalized at the Chaim Sheba Medical Center between July 2000 and December 2006 with the diagnosis of acute diverticulitis. Eighty two patients did not undergo colonoscopy and, therefore, only 224 patients were included in the study group (Figure 1).
Twenty three patients (10.3%) fulfilled the criteria for a persistent course of acute diverticulitis. Fourteen patients underwent an early colonoscopy and the other nine a late colonoscopy. Four patients (17.4%) clearly benefited from an early colonoscopy, whereas the remaining 19 patients underwent colonoscopy with no significant findings apart from the detection of diverticula and occasionally inflammation. Twelve of these patients eventually underwent sigmoidectomy because of recurrent episodes of diverticulitis, and their symptoms resolved. An additional two patients were offered sigmoidectomy, but refused. They continued to experience recurrent episodes of acute diverticulitis. The remaining five patients recovered completely with no further symptoms during a mean follow up period of 2.2 years. Interestingly, none of the patients with a regular non-persistent course demonstrated any benefit from colonoscopy (Table 1). Thus, colonoscopy was found to be beneficial only in patients with a persistent course of diverticulitis. The 4 patients in whom early colonoscopy seemed to be beneficial are described here.
| Colonoscopy | Protracted course (n = 23) | Non-protracted course (n = 201) |
| Beneficial | 4 (17.4%)b | 0 |
| Non-beneficial | 19 (82.6%) | 201 |
A 55-year-old man was admitted to another hospital 2 mo earlier with a clinical picture of acute diverticulitis. The patient was treated conservatively with IV antibiotics and was discharged after his symptoms subsided. Due to recurrent abdominal pain and fever he was readmitted to our hospital. In-hospital colonoscopy detected an obstructive mass in the sigmoid colon. Histology showed an adenocarcinoma. The patient underwent a sigmoidectomy.
A 50-year-old woman was hospitalized due to left lower quadrant pain, fever and weight loss of 6 kg over a 4 mo period. CT was interpreted as compatible with acute diverticulitis (Figure 2). After conservative treatment with IV antibiotics her symptoms improved and she was discharged. However, her symptoms did not resolve and she continued to have left lower quadrant pain. A colonoscopy, performed 2 mo later, revealed an obstructing mass in the sigmoid colon. Histology confirmed the diagnosis of adenocarcinoma. While waiting for her operation, she developed a free perforation and underwent emergency surgery with tumor resection and a temporary colostomy. Earlier colonoscopy could probably have enabled her to undergo elective surgery with primary closure of the colon.
A 60-year-old man was transferred from another hospital where he was hospitalized because of acute diverticulitis with an abscess in the left lower abdominal quadrant. The abscess was treated with IV antibiotics, but with no clinical response. A CT-guided drainage of the abscess was performed. Symptoms persisted, and the patient underwent colonoscopy. On colonoscopy, a 2-cm polyp was detected at the beginning of the inflamed area, 15 cm from the anus. Histology demonstrated a moderately differentiated adenocarcinoma arising in a tubulovillous adenoma. The tumor infiltrated the submucosa as well. No diverticuli were seen. The mucosa of the colonic segment between 15-30 cm looked irregular and biopsies showed nonspecific chronic inflammation. The patient underwent sigmoidectomy with resolution of his symptoms.
A 73-year-old woman was admitted with symptoms suggestive of acute diverticulitis. CT showed a thickened bowel wall of the sigmoid colon with multiple diverticula. The patient was treated with IV antibiotics for 10 d, with no improvement. On the 10th d of her hospitalization she underwent colonoscopy. On colonoscopy, a small chicken bone was found trapped in the diverticulum, with a purulent discharge from that diverticulum.
Removal of the bone during the colonoscopy produced complete recovery, and the patient was discharged asymptomatic and afebrile 1 d following the procedure.
In this prospective study, we assessed the value of performing an early colonoscopy in a selective group of patients with a persistent course of acute diverticulitis.
Our data showed 17.4% of such patients will benefit from an early colonoscopy. We believe non-responders to conventional therapy form a special subgroup of patients with acute diverticulitis. These patients have a more severe disease and worse prognosis, as demonstrated by the fact that sixty-five percent of these patients eventually underwent a sigmoidectomy.
In our previous publications, we showed the main disadvantage of performing an early colonoscopy during hospitalization is the higher rate of incomplete examinations (18%)[1314]. However, in this small but important group of patients with a persistent disease course, an early colonoscopy seemed to be beneficial. Therefore, the main question is whether in cases of persistent course of acute diverticulitis the benefit of performing an early colonoscopy prevails over the risk of an incomplete examination. Identifying the patients from this group in whom a benefit is expected from an early colonoscopy would probably contribute to decision making. Therefore, in this study we focused on patients with a persistent course of acute diverticulitis in whom colonoscopy was beneficial. Three of the four patients (patient No. 1, 3, 4) were briefly mentioned in our previous publications[89]. In this paper we concentrated on those patients and added an additional patient to our series.
However, we were unable to determine predictors for the subgroup of patients who may benefit from early colonoscopy. The reasons for this might be the small number of patients involved, or, simply, because there are no such predictors.
Nevertheless, in the light of the significant findings in this small group of patients, we believe colonoscopy should be offered to all patients with a protracted disease course. However, it is not advocated for patients with a non-protracted course.
In conclusion, early colonoscopy should be considered in all patients with a protracted clinical course. In this small group of patients, 17% of the patients will benefit from the procedure with no additional risk of complications.
Patients with persistent acute diverticulitis have longer disease duration and do not respond to conventional therapy. In previous studies we showed that early in-hospital colonoscopy is feasible and safe in patients with acute diverticulitis.
This study was designed to investigate the benefit from performing an early colonoscopy during hospitalization in patients with persistent acute diverticulitis.
Persistent acute diverticulitis affects about 10% of acute diverticulitis patients. This study showed that in this special group of patients, performing an early colonoscopy had a therapeutic benefit of 17%. Considering that performing an early colonoscopy during an attack of acute diverticulitis was shown to be safe in previous studies, this study suggests an early in-hospital colonoscopy should be considered in all patients with a persistent course of acute diverticulitis.
In this prospective study, the authors focused on the yield of performing an early colonoscopy in a well defined group of patients with acute diverticulitis - patients who suffer from a persistent disease course. Study results suggest that in this small group of patients early colonoscopy will detect other significant pathology which will change patient’s management in 17% of cases. Therefore, performing an early colonoscopy in patients with persistent diverticulitis is well advised.
| 1. | Hughes LE. Postmortem survey of diverticular disease of the colon. I. Diverticulosis and diverticulitis. Gut. 1969;10:336-344. |
| 2. | Garcia G. Diverticulitis. Eds. Infections of the gastrointestinal tract, 2nd ed. Philadelphia: Lippincott Williams & Wilkins 2002; 306-316. |
| 3. | Parks TG. Natural history of diverticular disease of the colon. Clin Gastroenterol. 1975;4:53-69. |
| 4. | Painter NS, Burkitt DP. Diverticular disease of the colon, a 20th century problem. Clin Gastroenterol. 1975;4:3-21. |
| 5. | Farrell RJ, Farrell JJ, Morrin MM. Diverticular disease in the elderly. Gastroenterol Clin North Am. 2001;30:475-496. |
| 6. | Wong WD, Wexner SD, Lowry A, Vernava A 3rd, Burnstein M, Denstman F, Fazio V, Kerner B, Moore R, Oliver G. Practice parameters for the treatment of sigmoid diverticulitis--supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum. 2000;43:290-297. |
| 7. | Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, Gonzalez-Ruiz C, Essani R, Beart RW Jr. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005;100:910-917. |
| 8. | Almy TP, Howell DA. Medical progress. Diverticular disease of the colon. N Engl J Med. 1980;302:324-331. |
| 9. | Penfold JC. Perforation of the colon complicating colonoscopy: report of a case. Dis Colon Rectum. 1975;18:626-627. |
| 10. | Forde KA. Colonoscopy in complicated diverticular disease. Gastrointest Endosc. 1977;23:192-193. |
| 11. | Dean AC, Newell JP. Colonoscopy in the differential diagnosis of carcinoma from diverticulitis of the sigmoid colon. Br J Surg. 1973;60:633-635. |
| 12. | Panish JF. Limitations and complications of colonoscopy. Gastrointest Endosc. 1980;26:20S-21S. |
| 13. | Sakhnini E, Lahat A, Melzer E, Apter S, Simon C, Natour M, Bardan E, Bar-Meir S. Early colonoscopy in patients with acute diverticulitis: results of a prospective pilot study. Endoscopy. 2004;36:504-507. |
| 14. | Lahat A, Yanai H, Menachem Y, Avidan B, Bar-Meir S. The feasibility and risk of early colonoscopy in acute diverticulitis: a prospective controlled study. Endoscopy. 2007;39:521-524. |
| 15. | Lahat A, Menachem Y, Avidan B, Yanai H, Sakhnini E, Bardan E, Bar-Meir S. Diverticulitis in the young patient--is it different? World J Gastroenterol. 2006;12:2932-2935. |