Published online Jan 7, 2008. doi: 10.3748/wjg.14.46
Revised: September 15, 2007
Published online: January 7, 2008
AIM: To evaluate the factors involved in the impairment of health-related quality of life (HRQOL) in patients with celiac disease.
METHODS: A multicenter, cross-sectional prospective study was performed in patients with celiac disease who completed two HRQOL questionnaires: the gastrointestinal quality of life index (GIQLI) and the EuroQol-5D (EQ).
RESULTS: Three hundred and forty patients (163 controlled with a gluten-free diet, and 177 newly diagnosed with a normal diet) were included. The GIQLI score was significantly better in patients on a gluten-free diet (GFD) than in non-treated patients on their usual diet, both in terms of the overall score (3.3 vs 2.7, respectively; P < 0.001), as well as on the individual questionnaire dimensions. Both the preference value of the EQ as the visual analogue scale were significantly better in treated than in non-treated patients (0.93 vs 0.72, P < 0.001 and 80 vs 70, P < 0.001, respectively). Variables significantly associated with a worse HRQOL score were female gender, failure to adhere to a GFD, and symptomatic status.
CONCLUSION: In untreated celiac disease, the most important factors that influence patient perception of health are the presence of symptoms and a normal diet. HRQOL improves to levels similar to those described in the general population in celiac disease patients well controlled with a GFD.
- Citation: Casellas F, Rodrigo L, Vivancos JL, Riestra S, Pantiga C, Baudet J, Junquera F, Diví VP, Abadia C, Papo M, Gelabert J, Malagelada J. Factors that impact health-related quality of life in adults with celiac disease: A multicenter study. World J Gastroenterol 2008; 14(1): 46-52
- URL: https://www.wjgnet.com/1007-9327/full/v14/i1/46.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.46
Celiac disease (CD) is a chronic immuno-inflammatory enteropathy that appears in genetically predisposed patients. Patients with this disease develop characteristic small-intestinal-mucosal changes, due to hypersensitivity to gluten. Several epidemiological factors, including a dramatic increase in the diagnosis of CD[1] and changes in its presentation, with the appearance of atypical forms, that may even mimic functional diseases, as well as the fact that it affects people of any age[2] mean that CD is currently considered a common and important health-care problem. It affects approximately 1%-2% of adults in Western European populations[3].
Although the understanding of the immunology and physiopathology of CD is extensive[45], the impact of the disease from the patient’s point of view has received less attention. The chronic nature of the condition, together with the limitations imposed by the need to follow a permanent restrictive diet, substantial numbers of physician visits, the risk of associated diseases and potential complications, mean that CD can have a considerable negative impact on health-related quality of life (HRQOL). Due to the lack of disease-specific instruments to measure HRQOL in CD patients, generic questionnaires, such as the SF-36 or EuroQol-5D (EQ), have been used. Overall perception of HRQOL is rated as bad or fair by 63% of patients before diagnosis of CD, and improves to 77% after treatment[6]. However, at least one study has indicated that treated CD patients rate their overall well-being, as measured with a visual analog scale (VAS), quite highly, with 83.6% of patients being rated as 'very well' or 'well'[7]. Apart from dietary treatment, other factors have been suggested to influence the HRQOL in CD patients. Some disease-related factors, such as the presence of symptoms or associated co-morbidity, as well as the type of diagnosis used (symptom-detected vs screening-detected), have also been shown to impair CD patients’ HRQOL[89]. Non-disease-related factors, such as female gender, also have a negative impact on HRQOL[10], although this is also true in other chronic diseases[11]. The impairment of HRQOL in untreated celiac disease and its improvement after treatment with a gluten-free diet (GFD), has been confirmed using generic multidimensional HRQOL measures[12]. However, there is no agreement as to whether the HRQOL of treated CD patients is similar[81314] or not[1516] to that of the general population.
The aims of the present study were to measure and compare the HRQOL in treated and untreated CD patients using condition-specific and generic measures of HRQOL, and to analyze the factors impacting on HRQOL in these patients. A further objective was to compare scores on the generic measure of HRQOL for the two study groups with general population reference scores for the same instrument (EQ). To this end, we performed a multicenter study in a representative sample of patients from different parts of Spain, including both large and small cities, and both island and mainland regions.
Subjects were adult outpatients with CD who attended the Digestive Services Units of seven different Spanish hospitals, over a one-year period. Diagnosis was based on current serological and histological criteria[17]. A total of 340 CD patients were included. At the time of inclusion, patients were stratified into two groups, according to whether they were already following a GFD (GFD group) or whether they had not yet started on the GFD (pretreatment group).
All patients completed a questionnaire on demographic details, current symptoms, information on the disease, and issues related to the GFD. They also completed the Gastrointestinal Quality of Life Index (GIQLI) questionnaire and the EQ, two generic HRQOL instruments.
Patient compliance following the GFD was measured using an adapted version of the self-administered question-naire developed by Morisky et al[18]. The questionnaire consisted of four items which measure the degree of treatment compliance, answered using dichotomous response options (yes/no). Two questions asked about unintentional lack of compliance (“sometimes I forget my diet/sometimes I do not comply carefully with my diet”), while the other two questions dealt with intentional lack of compliance (“when I feel well I sometimes discontinue my diet/when not feeling well I sometimes discontinue my diet”). If either question 3 or 4 was answered affirmatively, the patient was considered to have voluntarily discontinued his or her diet. If either question 1 or 2 was answered in the affirmative, the patient was considered to have involuntarily neglected or forgotten his or her diet. This questionnaire was originally developed to measure compliance with medication, and was adapted for use in the current population by substituting drugs with GFD. In a previous study[2], many patients suggested that they never forgot about their diet; for that reason, a fifth option was added to the scale (“I never forget about my diet”). Patients checking this answer were considered good compliers.
In an ancillary study, 17 patients from the pre-treatment group completed the questionnaires both at inclusion, when they had not yet started on the GFD, and at least 6 mo following treatment with GFD.
HRQOL was assessed using two generic questionnaires. GIQLI is a self-administered questionnaire designed to assess HRQOL in patients with gastrointestinal diseases. It was chosen because it has been translated and validated for use in Spain[19]. The GIQLI consists of 36 items grouped into five domains of health (gastrointestinal symptoms, physical dysfunction, social dysfunction, emotional dysfunction and treatment effects). Responses are scored on a 4-point Likert scale, in which 4 corresponds to the highest level of functioning. The instrument produces five dimension scores and an overall score ranging from 0 to 4, with a higher score reflecting better HRQOL.
EQ is a short self-administered generic utility measure that provides both a descriptive profile and an overall index for HRQOL. The EQ includes five dimensions (mobility, personal care, daily activities, pain and anxiety-depression) answered on a 3-point scale ranging from no problems (level 1) to extreme problems (level 3). Combining one level of severity from each of the five dimensions generates a number of discrete health states that can be assigned preference values ranging from 0, which represents worst health status, to 1 (best health status). The EQ also includes a VAS that ranges from 0 (worst imaginable health status) to 100 (best imaginable health status), on which patients were asked to mark the point that best reflected their health status on the day of the interview. The EQ has also been translated and validated in Spanish[20]. As a reference, normal values for a representative sample of 12 245 members of the Spanish general population also exist for the EQ, and we used these as a control for the patients included in the present study[2122].
The Kolmogorov-Smirnov test showed that most of the study variables did not have a normal distribution. Descriptive analyses of socio-demographic, clinical and HRQOL data were therefore performed using medians and 25th and 75th percentiles. Qualitative variables were described as proportions. Comparisons between variables were performed using the Mann-Whitney U, Kruskal-Wallis or Fisher tests as appropriate. In the pre-treatment group, HRQOL was also analyzed depending on whether the diagnosis was performed on the basis of symptoms or on positive serology.
Three multiple linear regression models were developed to identify independent variables that influence HRQOL. Dependent variables in the three models were the overall GIQLI score, the EQ preference value index, and the EQ VAS scores. Independent variables in all models were GFD, sex, age, duration of symptoms, and the binary variables were existence of symptoms and presence of CD-associated diseases. Results obtained for the multiple linear regression model were the regression coefficient, t-test statistics, P values, and the variance inflation factor. The t test established whether the independent variables contributed to predicting the dependent variables. Higher t-test values indicate that the independent variable more strongly predicts the dependent variable. It has been considered that each independent variable contributes to predicting the dependent variable when P < 0.05. The variance inflation factor, a measure of multicollinearity, measures the inflation of the standard error of each regression coefficient for an independent variable due to redundant information in other independent variables. If the variance inflation factor is 1.0, there is no redundant information in the other independent variables. The level of statistical significance for the multiple regression model was set at P < 0.05.
A total of 340 patients from seven hospitals in different areas of Spain were included. Table 1 summarizes the socio-demographic and clinical characteristics, according to whether they were in the GFD group (n = 163) or the pre-treatment group (n = 177).
| Pre-treatment | GFD | |
| Number | 177 | 163 |
| Age (yr) | 44 (30-50) | 37 (28-47)a |
| Sex (male/female) | 74/103 | 42/121 |
| Smoking status | ||
| Smoker | 29 (16) | 33 (25) |
| Non-smoker | 148 (84) | 130 (75) |
| City of residence | ||
| < 100 000 inhabitants | 69 (43) | 61 (39) |
| 100 000-500 000 | 72 ( 45) | 65 (41) |
| > 500 000 | 18 (12) | 31 (20) |
| Family status | ||
| Single | 57 (33) | 67 (42) |
| Married | 108 (63) | 84 (53) |
| Widowed | 5 (4) | 8 (5) |
| Educational level | ||
| No studies | 7 (4) | 4 (2) |
| Primary | 56 (33) | 38 (24) |
| Secondary | 55 (32) | 61 (38) |
| University studies | 52 (31) | 55 (36) |
| Occupational status | ||
| Employee/self-employed | 67 (41) | 94 (62) |
| Retired/pensioner | 36 (22) | 14 (9) |
| Housewife | 30 (18) | 16 (10 ) |
| Student | 12 (7) | 19 (12) |
| Unemployed | 17 (12) | 10 (7) |
| Disease duration (mo) | - | 48 (24-84) |
| Duration of symptoms before diagnosis (mo) | 24 (7-84) | 12 (5-40) |
| Presence of symptoms at inclusion | 118 (80) | 52 (33)b |
| Presence of associated diseases at inclusion | 42 (41) | 41 (37) |
There were no relevant differences in demographic characteristics between the two groups. Age ranged from 15 to 78 years. Treated patients were younger than non-treated patients [median age 37 (28-47) vs 44 (30-50) years, respectively; P < 0.05], but the difference was not considered clinically relevant. The sample characteristics were also in accordance with the results of previous epidemiological studies of CD in Spain[2], with patients being young adults and predominantly female and non-smokers. Most patients lived in small to medium-sized cities, with < 500 000 inhabitants.
The duration of disease since diagnosis was not evaluated in the normal diet group because they were included at the time of diagnosis. There were no statistically significant differences in duration of symptoms before diagnosis of CD between treated and pre-treated patients. The disease presented in the classic form in 47 (32%) patients in the GFD group and in 13 (11%) patients in the normal diet group (P < 0.01). The most frequently presenting non-classical forms of CD included anemia (32%), cutaneous lesions (9%), and hypertransaminasemia (6%). Approximately 40% of patients had associated diseases, such as thyroid diseases (7%), selective IgA deficiency (3%), type I diabetes mellitus (5%), depression (11.1%), and chronic inflammatory arthropathy (8%). The percentage of asymptomatic patients at inclusion was significantly higher in the treated GFD group than in the normal diet group (80% vs 33%, P < 0.01). In the GFD group, 117 patients (73%) were classified as good compliers on the basis of their Morisky scores, 36 (22%) reported that they occasionally involuntarily neglected or forgot the diet, and eight (5%) had voluntarily discontinued the diet. Again in the GFD group, 47% of patients reported complete disappearance of symptoms since being on the diet, and 43% reported a significant improvement in symptoms. Eight per cent of patients reported a small improvement in symptoms, and 2% considered that their symptoms had not changed with treatment.
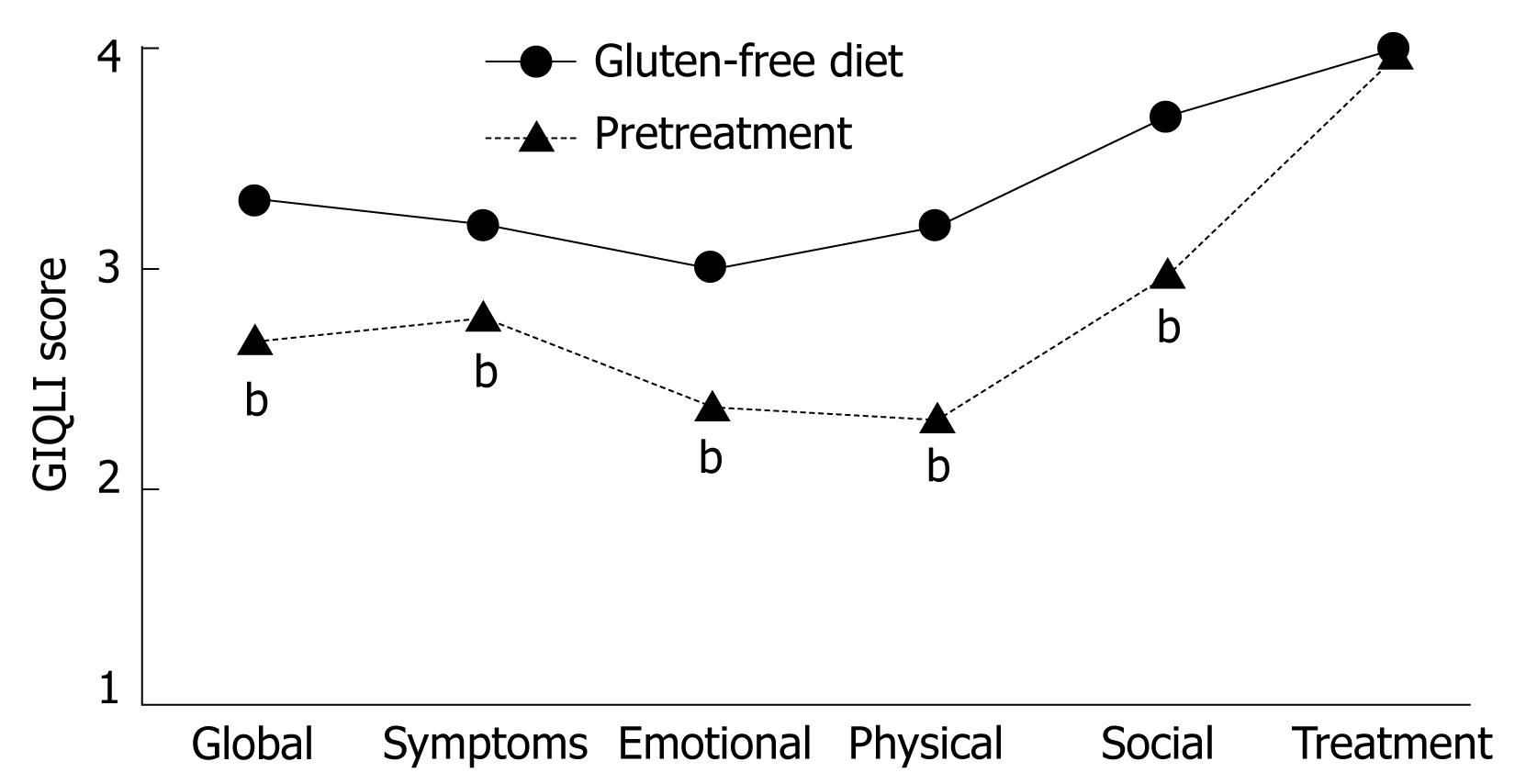
Figure 1 shows the overall score and the five dimensions of GIQLI for the GFD and pre-treatment groups. Patients in the GFD group reported significantly (P < 0.001) better HRQOL than patients in the pre-treatment group for the overall score and the gastrointestinal symptoms, and in the physical, social and emotional dysfunction dimensions.
Patients in the pre-treatment normal diet group scored best on GIQLI treatment effects domain [4.0 (3.0-4.0)], while the domains with the worst scores were physical dysfunction [2.3 (1.4-2.9)], emotional dysfunction [2.4 (1.8-3.0)], and gastrointestinal symptoms [2.8 (2.4-3.3)]. These results suggested that most impaired domains of health in newly diagnosed CD patients were related to symptomatic and emotional dimensions. In GFD patients, the best scored domain was also the treatment domain [4.0 (3.0-4.0)] and the worst scored was emotional dysfunction [3.0 (2.4-3.4)], which suggested that, although improved by treatment, the most sustained impairment affected the emotional dimension.
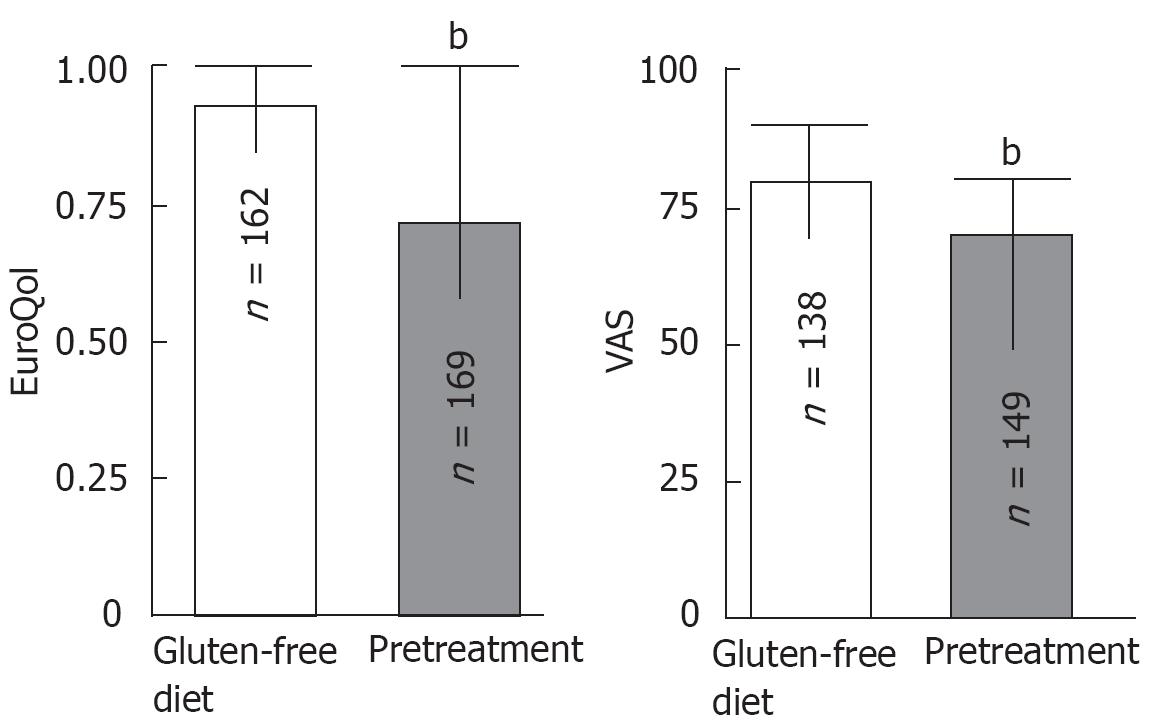
Median scores on the EQ preference value index and VAS are shown in Figure 2. The median EQ preference value was significantly higher in GFD patients than in the normal diet group [0.93 (0.85-1.0) vs 0.72 (0.58-1.0) respectively, P < 0.001]. The median VAS score was also significantly higher in GFD patients than in the normal diet group [80 (70-90) vs 70 (50-80) respectively, P < 0.001]. Presence (levels of severity 2 and 3) or absence (level 1) of problems for each EQ dimension for the GFD and normal diet patients are shown in Table 2. At diagnosis, the normal diet group patients reported problems with significantly greater frequently than those in the GFD group on all five dimensions of the EQ, which confirmed that GFD improved patient perception of health. In the normal diet group, problems were reported most frequently in the pain/discomfort (62%) and anxiety/depression (54.5%) dimensions, and least frequently in the self-care dimension (10.2%). In the GFD group, problems were reported most frequently on the EQ anxiety/depression dimension (33.9%), in consonance with the low score of the emotional dimension in the GIQLI observed in this group of patients.
| Variable | Pre-treatment | Gluten-free diet | ||
| No problems | Some problems | No problems | Some problems | |
| Mobility | 130 (74.3) | 45 (25.7) | 146b (90.1) | 16 (9.9) |
| Self-care | 158 (89.8) | 18 (10.2) | 161b (99.3) | 1 (0.7) |
| Usual activities | 113 (64.5) | 62 (35.5) | 135b (83.3) | 27 (16.7) |
| Pain/Discomfort | 67 (38) | 109 (62) | 117b (72.8) | 45 (27.7) |
| Anxiety/Depression | 80 (45.5) | 96 (54.5) | 107b (66.1) | 55 (33.9) |
Table 3 shows the results of the multiple regression analysis, which took the GIQLI overall score as a dependent variable for all patients. The analysis suggested that the presence of symptoms, normal diet and female gender were the strongest determinants (P < 0.001) for a worse perception of HRQOL.
| Independent variable | t-test statistics | P value | Variance inflation factor |
| Pretreatment/treatment | 4.989 | < 0.001 | 1.31 |
| Age | -0.725 | 0.469 | 1.31 |
| Gender (m/f) | -2.684 | 0.008 | 1.06 |
| Smoking habit | 1.038 | 0.301 | 1.02 |
| Symptoms duration | -1.813 | 0.072 | 1.08 |
| Presence of symptoms | -4.932 | < 0.001 | 1.31 |
| Associated diseases | -1.824 | 0.070 | 1.18 |
Similar results were obtained using the linear regression analysis with the EQ preference value index (Table 4) and the EQ VAS (Table 5) as the dependent variables, and included the same independent variables as described earlier. Presence of symptoms and normal diet represented significant determinants of worse HRQOL. In this case, the presence of CD-associated diseases was also associated with poorer HRQOL.
| Independent variable | t-test statistics | P value | Variance inflation factor |
| Pretreatment/treatment | 3.20 | 0.002 | 1.31 |
| Age | 0.44 | 0.663 | 1.20 |
| Gender (m/f) | -1.12 | 0.261 | 1.07 |
| Smoking habit | 0.58 | 0.559 | 1.02 |
| Symptoms duration | -1.61 | 0.109 | 1.08 |
| Presence of symptoms | -5.09 | < 0.001 | 1.31 |
| Associated diseases | -2.61 | 0.01 | 1.18 |
| Independent variable | t-test statistics | P value | Variance inflation factor |
| Pretreatment/treatment | 2.97 | 0.003 | 1.37 |
| Age | 0.81 | 0.420 | 1.23 |
| Gender (m/f) | -1.48 | 0.141 | 1.11 |
| Smoking habit | -0.49 | 0.624 | 1.02 |
| Symptoms duration | -2.71 | 0.007 | 1.08 |
| Presence of symptoms | -5.99 | < 0.001 | 1.40 |
| Associated diseases | -2.50 | 0.013 | 1.17 |
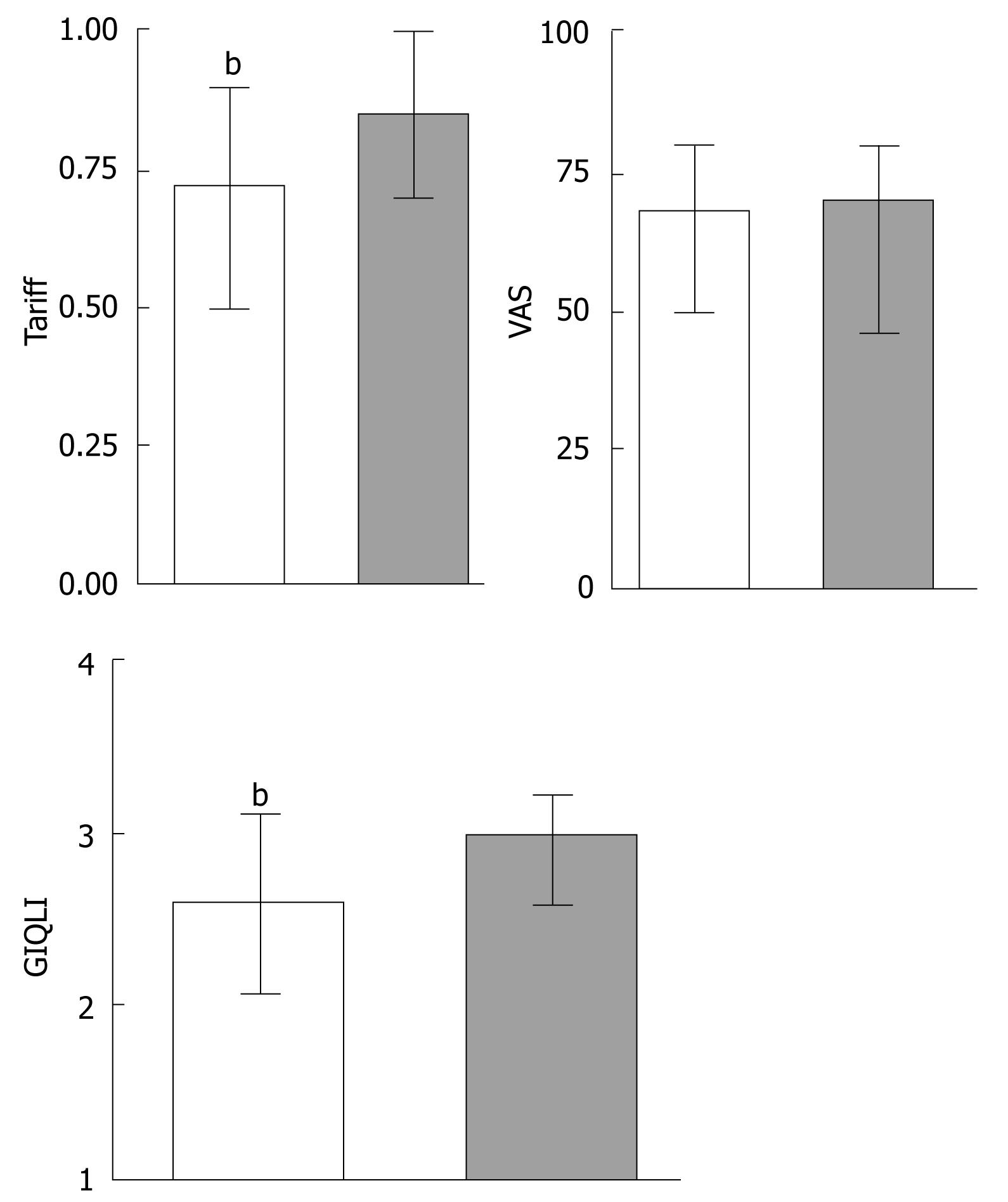
In the pre-treated normal diet group, results of the comparison of patients diagnosed according to the presence of symptoms or a positive serology (n = 26) are shown in Figure 3. HRQOL was significantly worse in patients diagnosed through symptoms rather than through serologic tests without observable symptoms. The worst HRQOL was, therefore, found in women who had been recently diagnosed due to the presence of symptoms, who were in the normal diet group, and who had associated diseases.
In the GFD group, specific potential factors that may be related to HRQOL, such as compliance or response to diet, were assessed. There were no statistically significant differences in median overall GIQLI score between patients classified as good compliers (n = 117), and those who involuntarily neglected or forgot their diet (n = 36), and those who had voluntarily interrupted their diet (n = 8) [median GIQLI (IQR) scores, 3.3 (2.8-3.5), 3.2 (2.8-3.4), and 2.9 (2.6-3.3), respectively]. In contrast, GIQLI scores were significantly higher (better HRQOL) in the 73 patients who reported achieving complete control of symptoms with the GFD, than in patients reporting a partial or non-response (n = 84) [3.4 (3.1-3.6)] vs [3.0 (2.7-3.4), P < 0.001]. With reference to the potential effect of GFD duration on HRQOL, the duration of treatment and GIQLI overall score were slightly correlated (r = 0.19, P < 0.05) according to the Spearman rank correlation test. Similar correlation was observed with the EQ preference value index and the EQ VAS (r = 0.20, P < 0.05 and r = 0.15, P = NS).
Although statistical comparisons between CD patients’ EQ scores and those described for the Spanish general population (median preference value of 1.0 and VAS score of 80) were not performed, it seems apparent that treated patients do not have different preference values and VAS scores to the Spanish general population. In contrast, preferences and VAS scores of the normal diet group were worse than those of the general population. According to the distribution of EQ VAS scores in the Spanish general population (21), CD patients perceive their health as good to excellent (VAS scores between 70 and 100), while untreated patients with newly diagnosed CD have VAS scores corresponding to fair health.
Seventeen newly diagnosed patients [11 women, six men, median age 48 (34-60) years] completed the HRQOL questionnaire before initiating treatment and after 6-23 mo with GFD. Paired comparisons using the Wilcoxon signed rank test showed that treatment improved significantly the GIQLI overall score [from a median of 2.6 (2.3-3.0) to 2.9 (2.7-3.4), P <0.001] and the VAS score [from 70 (55-70) to 77 (70-87) respectively, P < 0.01]. However, the median EQ preference value increase after treatment did not reach statistical significance [0.85 (0.69-1.0) to 0.87 (0.71-1.0), P = NS].
To analyze how CD affects HRQOL and to determine which factors are associated, we administered two generic instruments to measure HRQOL in two groups of CD patients: 163 patients following a GFD and 177 newly diagnosed patients who were on a normal diet. A potential limitation of the study is a selection bias for patients because we only included hospital-controlled patients. Results on the GIQLI and EQ questionnaires suggest that the HRQOL of untreated recently diagnosed CD patients is significantly impaired, on almost all of the dimensions on both instruments and on the overall score. It is not surprising then that these patients’ assessment of their overall health on the EQ should be equivalent to a rating of only fair health. Patients before starting a GFD only scored well on the treatment effects dimension on the GIQLI questionnaire. Although these patients have not initiated the GFD, the highly-scored dimension was treatment, probably because this item refers to “feeling let down by treatment effects” and most patients have received prior diet or drug recommendations, or because patients tend to respond neutrally to items in this domain. By contrast, CD patients controlled with a GFD reported significantly better HRQOL, and in fact had EQ scores that were very similar to those of a representative sample of the Spanish general population[2122]. These results study are in line with those reported very recently by the Canadian Celiac Association[23]. In that study, it was found that SF-12 summary scores for CD patients were similar to the normative Canadian data, except for females and newly diagnosed patients.
The importance of adequate compliance with a GFD is confirmed by the multivariate analysis, in which it was shown that GFD exerted a major influence on HRQOL, whether using the condition-specific GIQLI or the generic EQ instrument. To avoid the problem of between-person variability in the determination of the effect of GFD on HRQOL, in a subgroup of newly diagnosed patients, the HRQOL was re-measured after at least 6 mo on GFD. Results of that ancillary study confirmed that treatment of CD improves HRQOL. The multivariate analysis also indicated that the presence of symptoms and comorbidity were other independent variables that significantly influenced HRQOL in CD patients. These results suggest that compliance with GFD and adequate control of symptoms are decisive, in terms that CD patients may recover to satisfactory levels of self-perceived health. The duration of improvements in HRQOL in CD patients following a GFD could not be deduced from our study, but it has been suggested that such improvements may be maintained for as long as 20 years[14].
Although our study confirmed that a GFD improves symptoms, with 90% of patients reporting a clinically significant improvement, as well as raising CD patients’ levels of HRQOL to those reported by the general population, other studies, such as that by the Westchester Celiac Sprue Support Group have observed negative effects of a GFD on HRQOL in areas such as dining out, travel and family life[24]. These aspects were not covered in depth by either of the HRQOL instruments included here, and they should be considered for inclusion in future studies.
Advances in the serologic diagnosis of CD mean that the disease is recognized at increasingly early times, even in asymptomatic patients. Presumably as a result of the absence of symptoms in patients diagnosed by serologic screening, as opposed to patients diagnosed by clinical symptoms, it has been suggested that screening-detected CD patients have better HRQOL than those diagnosed based on symptoms[1025]. There is no agreement as to whether a GFD improves HRQOL independently of whether diagnosis was based on serologic screening or on symptoms, with some evidence suggesting that improvements in HRQOL occur in both types of patients[25], and other evidence pointing out that they are only found in symptom-detected patients[10]. Our study also provides some evidence that symptom-detected patients have significantly lower overall scores on the GIQLI and on the EQ preference index than serologic-detected patients, which suggests that the former have better self-perceived health on diagnosis. However, the nature of the present study meant that it was not possible to determine whether diet-induced improvements in HRQOL were related or not to the type of diagnosis.
The only non-disease-related variable that had a significant influence on HRQOL was gender, with women scoring significantly poorer on the GIQLI questionnaire. It has been suggested that in treated CD patients, low scoring of SF-36 is confined to female patients[15]. However, in our study, the influence of gender on HRQOL was less clear because, although female sex was a significant independent variable for poorer perception of HRQOL as measured by the GIQLI, the effect was not seen on either the EQ preference value index or on the EQ VAS.
Our results suggest that untreated newly diagnosed CD has a significant negative impact on several domains of HRQOL, and that HRQOL is more impaired in symptomatic patients and in those with CD-associated diseases. On the other hand, HRQOL improves to levels observed in the general population when CD is controlled with a GFD. From our observations, it can be concluded that the assessment of HRQOL in CD patients is relevant because it improves physicians’ knowledge of the implications of the disease, and helps patients to recognize the general impact of the disease. Additionally, the fact that patients following a GFD report similar levels of HRQOL as members of the general population should encourage patients to adhere to the GFD.
Celiac disease (CD) is a chronic immuno-inflammatory enteropathy that appears in genetically predisposed patients, who develop characteristic small-intestinal-mucosal changes, due to hypersensitivity to gluten. The chronic nature of the condition, together with the limitations imposed by the need to follow a permanent restrictive diet, substantial numbers of physician visits, the risk of associated diseases and potential complications, mean that CD can have a considerable negative impact on health-related quality of life (HRQOL). The impairment of HRQOL in untreated CD and its improvement after treatment with a gluten-free diet (GFD), has been suggested using generic multidimensional HRQOL measures.
There is a lack of information relative to some areas in the research of HRQOL in CD. There is no agreement as to whether the HRQOL of treated CD patients reaches that of the general population, the factors involved in HRQOL impairment, and in the use of more specific instruments to measure the HRQOL of CD patients.
Two instruments to measure HRQOL in two groups of CD patients: 163 patients following a GFD and 177 newly diagnosed patients who were on a normal diet containing gluten. Results on the gastrointestinal quality of life index GIQLI and EuroQol-5D EQ questionnaires suggested that the HRQOL of untreated, recently diagnosed CD patients was significantly impaired, on almost all of the dimensions on both instruments and on the overall score. Patients, before starting a GFD, considered their overall health equivalent to a rating of only fair. CD patients controlled with a GFD reported significantly better HRQOL, and in fact had EQ scores that were very similar to those of a representative sample of the Spanish general population. The importance of diet on CD was confirmed in an ancillary study in which HRQOL was re-measured after at least 6 mo on GFD. Results of that ancillary study confirm that treatment of CD improves HRQOL. Our study also provided some evidence that symptom-detected patients had significantly lower overall scores on the GIQLI and on the EQ preference index than serologic-detected patients, which suggested that the former had better self-perceived health on diagnosis. To determine the factors involved in HRQOL impairment in CD, a multivariate analysis using the condition-specific GIQLI or the generic EQ instrument was performed. Results of that analysis suggested that the variables significantly associated with a worse HRQOL were female gender, failure to follow a GFD, and symptomatic status.
The results of the present study suggest that compliance with a GFD and adequate control of symptoms are decisive in terms that CD patients may recover to satisfactory levels of self-perceived health. The assessment of HRQOL in CD patients is relevant because it improves physicians’ knowledge of the implications of the disease and helps patients to recognize the general impact of the disease. The fact that patients following a GFD reached similar levels of HRQOL as members of the general population should encourage patients to adhere to a GFD.
HRQOL has a recognized importance to evaluate, manage and follow patients with chronic diseases, such as CD. Different types of instruments for measuring HRQOL have been introduced, with the most important being the questionnaires. There are generic questionnaires and disease-specific questionnaires. Although a specific questionnaire for CD has recently been published, the most widely used instruments to measure HRQOL in CD are the generic questionnaires. GIQLI is a self-administered questionnaire designed to assess HRQOL in patients with gastrointestinal diseases. The GIQLI consists of 36 items grouped into five domains of health (gastrointestinal symptoms, physical dysfunction, social dysfunction, emotional dysfunction and treatment effects). Responses are scored on a 4-point Likert scale, in which 4 corresponds to the highest level of functioning. EQ is a self-administered generic utility measure that provides both a descriptive profile and an overall index for HRQOL. The EQ includes five dimensions (mobility, personal care, daily activities, pain and anxiety–depression) answered on a 3-point scale ranging from no problems (level 1) to extreme problems (level 3). Combining one level of severity from each of the five dimensions generates a number of discrete health states that can be assigned preference values ranging from 0, which represents worst health status, to 1 (best health status). The EQ also includes a VAS that ranges from 0 (worst imaginable health status) to 100.
This is a well designed study addressing an important aspect of celiac disease which adds considerably to what is already known.
| 1. | Fasano A, Catassi C. Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology. 2001;120:636-651. |
| 2. | Casellas F, Lopez Vivancos J, Malagelada JR. Current epidemiology and accessibility to diet compliance in adult celiac disease. Rev Esp Enferm Dig. 2006;98:408-419. |
| 3. | West J, Logan RF, Hill PG, Lloyd A, Lewis S, Hubbard R, Reader R, Holmes GK, Khaw KT. Seroprevalence, correlates, and characteristics of undetected coeliac disease in England. Gut. 2003;52:960-965. |
| 4. | Shan L, Qiao SW, Arentz-Hansen H, Molberg O, Gray GM, Sollid LM, Khosla C. Identification and analysis of multivalent proteolytically resistant peptides from gluten: implications for celiac sprue. J Proteome Res. 2005;4:1732-1741. |
| 5. | Kagnoff MF. Overview and pathogenesis of celiac disease. Gastroenterology. 2005;128:S10-S18. |
| 6. | Green PHR, Stavropoulos SN, Panagi SG, Goldstein SL, Mcmahon DJ, Absan H, Neugut AI. Characteristics of adult celiac disease in the USA: results of a national survey. Am J Gastroenterol. 2001;96:126-131. |
| 7. | Ciacci C, D'Agate C, De Rosa A, Franzese C, Errichiello S, Gasperi V, Pardi A, Quagliata D, Visentini S, Greco L. Self-rated quality of life in celiac disease. Dig Dis Sci. 2003;48:2216-2220. |
| 8. | Usai P, Minerba L, Marini B, Cossu R, Spada S, Carpiniello B, Cuomo R, Boy MF. Case control study on health-related quality of life in adult coeliac disease. Dig Liver Dis. 2002;34:547-552. |
| 9. | Hallert C, Granno C, Hulten S, Midhagen G, Strom M, Svensson H, Valdimarsson T. Living with coeliac disease: controlled study of the burden of illness. Scand J Gastroenterol. 2002;37:39-42. |
| 10. | Johnston SD, Rodgers C, Watson RG. Quality of life in screen-detected and typical coeliac disease and the effect of excluding dietary gluten. Eur J Gastroenterol Hepatol. 2004;16:1281-1286. |
| 11. | Casellas F, Lopez-Vivancos J, Casado A, Malagelada JR. Factors affecting health related quality of life of patients with inflammatory bowel disease. Qual Life Res. 2002;11:775-781. |
| 12. | Casellas F, Lopez Vivancos J, Malagelada JR. Perceived health status in celiac disease. Rev Esp Enferm Dig. 2005;97:794-804. |
| 13. | Cranney A, Zarkadas M, Graham ID, Switzer C. The Canadian celiac health survey-the Ottawa chapter pilot. BMC Gastroenterol. 2003;3:8. |
| 14. | O'Leary C, Wieneke P, Healy M, Cronin C, O'Regan P, Shanahan F. Celiac disease and the transition from childhood to adulthood: a 28-year follow-up. Am J Gastroenterol. 2004;99:2437-2441. |
| 15. | Hallert C, Granno C, Grant C, Hulten S, Midhagen G, Strom M, Svensson H, Valdimarsson T, Wickstrom T. Quality of life of adult coeliac patients treated for 10 years. Scand J Gastroenterol. 1998;33:933-938. |
| 16. | Fera T, Cascio B, Angelini G, Martini S, Guidetti CS. Affective disorders and quality of life in adult coeliac disease patients on a gluten-free diet. Eur J Gastroenterol Hepatol. 2003;15:1287-1292. |
| 17. | World Gastroenterology Organisation. WGO-OMGE Practice Guideline: Celiac Disease. World Gastroenterol News. 2005;10:1-8. |
| 18. | Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67-74. |
| 19. | Quintana JM, Cabriada J, Lopez de Tejada I, Varona M, Oribe V, Barrios B, Perdigo L, Bilbao A. Translation and validation of the gastrointestinal Quality of Life Index (GIQLI). Rev Esp Enferm Dig. 2001;93:693-706. |
| 20. | Badia X, Fernández E, Segura A. Influence of socio-demographic and health status variables on evaluation of health states in a Spanish population. Eur J Public Health. 1995;5:87-93. |
| 21. | Badia X, Roset M, Montserrat S, Herdman M, Segura A. The Spanish version of EuroQol: a description and its applications. European Quality of Life scale. Med Clin (Barc). 1999;112 Suppl 1:79-85. |
| 22. | Badia Llach X, Herdman M, Schiaffino A. Determining correspondence between scores on the EQ-5D'; thermometer'; and a 5-point categorical rating scale. Med Care. 1999;37:671-677. |
| 23. | Zarkadas M, Cranney A, Case S, Molloy M, Switzer C, Graham ID, Butzner JD, Rashid M, Warren RE, Burrows V. The impact of a gluten-free diet on adults with coeliac disease: results of a national survey. J Hum Nutr Diet. 2006;19:41-49. |
| 24. | Lee A, Newman JM. Celiac diet: its impact on quality of life. J Am Diet Assoc. 2003;103:1533-1535. |
| 25. | Mustalahti K, Lohiniemi S, Collin P, Vuolteenaho N, Laippala P, Maki M. Gluten-free diet and quality of life in patients with screen-detected celiac disease. Eff Clin Pract. 2002;5:105-113. |