Published online Mar 7, 2007. doi: 10.3748/wjg.v13.i9.1458
Revised: January 20, 2007
Accepted: February 5, 2007
Published online: March 7, 2007
Perforation of the gallbladder with cholecystohepatic communication is a rare cause of liver abscess. Because it is a rare entity, the treatment modality has not been fully established. We report for the first time a patient with an intrahepatic abscess due to gallbladder perforation successfully treated by endoscopic stent placement into the gallbladder who had a poor response to continuous percutaneous drainage.
- Citation: Kang MS, Park DH, Kwon KD, Park JH, Lee SH, Kim HS, Park SH, Kim SJ. Endoscopic transcystic stent placement for an intrahepatic abscess due to gallbladder perforation. World J Gastroenterol 2007; 13(9): 1458-1459
- URL: https://www.wjgnet.com/1007-9327/full/v13/i9/1458.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i9.1458
Perforation of the gallbladder with cholecystohepatic communication is a rare cause of liver abscess[1-3]. Percutaneous drainage with systemic antibiotics is the initial treatment for these conditions[2]. However, the presence of a biliary communication is associated with significantly longer periods of catheter drainage, because continuous bile flow into the abscess cavity through the communicating tract hindered the natural healing course, resulting in prolonged healing time[4]. Moreover, continuous catheter drainage has its drawbacks, including discomfort in the patient, the nuisance of catheter maintenance, and accidental catheter dislodgement[5,6].
To our knowledge, this is the first case of an intrahepatic abscess due to gallbladder perforation successfully treated by endoscopic transcystic stent placement to the gallbladder who had a poor response to continuous percutaneous drainage.
A 70-year-old man was hospitalized for fever, right upper quadrant pain, and general weakness due to a poor appetite.
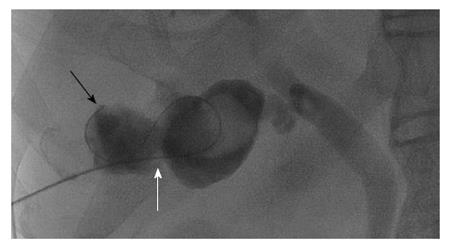
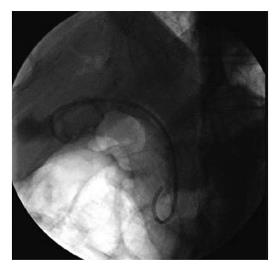
Abdominal computed tomography (CT) was performed to clarify the origin of fever. A 5-cm hepatic abscess was found in the right lobe adjacent to the gallbladder (Figure 1A). An 8-Fr pigtail catheter was percutaneously inserted into the abscess pocket, and purulent pus was drained. Following catheter insertion, we discovered a communication between the abscess and the gallbladder with a large stone (Figure 2). Systemic antibiotics were administered. Although elective cholecystectomy was considered, his poor general condition which was associated with uncontrolled dementia and hemiparesis due to a previous stroke contraindicated surgery. Two weeks after percutaneous drainage, the patient unintentionally removed the inserted pigtail catheter. We decided to attempt internal drainage to prevent the patient from self-removing the percutaneous catheter repeatedly. There was no change in the size of the hepatic abscess on follow-up CT (Figure 1B). Therefore, endoscopic transcystic stent (a 7-Fr 10-cm-long double pigtail biliary stent, Zimmon; Wilson-Cook, Winston-Salem, N.C.) was placed into the gallbladder (Figure 3). There were no procedure-related complications such as bile leak, peroration, or bleeding.
Ten days after the insertion of the double pigtail biliary stent, the patient’s general condition improved, and a follow-up abdominal CT showed that the size of abscess pocket decreased markedly measuring approximately 0.5 cm (Figure 1C). The patient was discharged after an uneventful recovery and has remained in good condition with the stent in place during the 7-mo follow-up.
Because liver abscesses associated with gallbladder perforation with cholecystohepatic communication is rare, the treatment modality has not been fully established[1-3].
In this case, surgical management was not considered because of the patient’s poor general condition. Although percutaneous drainage was maintained for the liver abscess, there was no clinical or radiological improvement. In addition, percutaneous drainage could not be kept for a long period, because the patient was demented. Some liver abscesses with biliary communication are refractory to percutaneous drainage alone. For such abscesses, endoscopic drainage including papillotomy, nasobiliary drainage, or biliary stenting may be an effective treatment[4,7]. We believe that a large gallstone may provoke bile flow of the gallbladder to the communicating tract, resulting in a poor response to percutaneous drainage for the intrahepatic abscess, and if the bile was diverted away from the communicating tract, the bile flow into the abscess cavity would cease, thereby enhancing the healing of both the tract and abscess[4]. Therefore, endoscopic transcystic biliary drainage of gallbladder was designed as an alternative management. To date, the stent has remained in situ without any complications for 7 mo of follow-up in this case. Because the patency results of the endoscopic gallbladder stent placement vary[8,9], regular evaluation of stent patency may be also required in this particular case.
In conclusion, the endoscopic transcystic placement of a biliary stent to the gallbladder may be effective as an alternative management for patients with hepatic abscesses caused by a perforated gallbladder with cholecystohepatic communication, who have poor responses to continuous percutaneous drainage.
| 1. | Bakalakos EA, Melvin WS, Kirkpatrick R. Liver abscess secondary to intrahepatic perforation of the gallbladder, presenting as a liver mass. Am J Gastroenterol. 1996;91:1644-1646. [PubMed] |
| 2. | Peer A, Witz E, Manor H, Strauss S. Intrahepatic abscess due to gallbladder perforation. Abdom Imaging. 1995;20:452-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Chen JJ, Lin HH, Chiu CT, Lin DY. Gallbladder perforation with intrahepatic abscess formation. J Clin Ultrasound. 1990;18:43-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Sharma BC, Agarwal N, Garg S, Kumar R, Sarin SK. Endoscopic management of liver abscesses and cysts that communicate with intrahepatic bile ducts. Endoscopy. 2006;38:249-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Miller FJ, Ahola DT, Bretzman PA, Fillmore DJ. Percutaneous management of hepatic abscess: a perspective by interventional radiologists. J Vasc Interv Radiol. 1997;8:241-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Yu SC, Ho SS, Lau WY, Yeung DT, Yuen EH, Lee PS, Metreweli C. Treatment of pyogenic liver abscess: prospective randomized comparison of catheter drainage and needle aspiration. Hepatology. 2004;39:932-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 144] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Sugiyama M, Atomi Y. Pyogenic hepatic abscess with biliary communication. Am J Surg. 2002;183:205-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Schlenker C, Trotter JF, Shah RJ, Everson G, Chen YK, Antillon D, Antillon MR. Endoscopic gallbladder stent placement for treatment of symptomatic cholelithiasis in patients with end-stage liver disease. Am J Gastroenterol. 2006;101:278-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Conway JD, Russo MW, Shrestha R. Endoscopic stent insertion into the gallbladder for symptomatic gallbladder disease in patients with end-stage liver disease. Gastrointest Endosc. 2005;61:32-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
S- Editor Liu Y L- Editor Ma JY E- Editor Ma WH