Published online Feb 7, 2007. doi: 10.3748/wjg.v13.i5.804
Revised: October 3, 2006
Accepted: October 23, 2006
Published online: February 7, 2007
Percutaneous radiofrequency thermal ablation (RFA) is an effective and safe therapeutic modality in the management of liver malignancies, performed with ultrasound guidance. Potential complications of RFA include liver abscess, ascites, pleural effusion, skin burn, hypoxemia, pneumothorax, subcapsular hematoma, hemoperitoneum, liver failure, tumour seeding, biliary lesions. Here we describe for the first time a case of biliary gastric fistula occurred in a 66-year old man with a Child’s class A alcoholic liver cirrhosis as a complication of RFA of a large hepatocellular carcinoma lesion in the III segment. In the light of this case, RFA with injection of saline between the liver and adjacent gastrointestinal tract, as well as laparoscopic RFA, ethanol injection (PEI), or other techniques such as chemoembolization, appear to be more indicated than percutaneous RFA for large lesions close to the gastrointestinal tract.
- Citation: Falco A, Orlando D, Sciarra R, Sergiacomo L. A case of biliary gastric fistula following percutaneous radiofrequency thermal ablation of hepatocellular carcinoma. World J Gastroenterol 2007; 13(5): 804-805
- URL: https://www.wjgnet.com/1007-9327/full/v13/i5/804.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i5.804
Percutaneous radiofrequency thermal ablation (RFA) is an emerging therapeutic modality in the management of liver malignancies[1], particularly in patients who cannot undergo surgery[2]. The increasing attractiveness of this technique is due to its effectiveness, safety and low morbidity rate[1,2]. Compared with ethanol injection (PEI), the first percutaneous therapy to be introduced, RFA is characterized by the need of a reduced number of treatment sessions. Both therapies are generally performed with ultrasound (US) guidance which allows considerable ease of application, due to their low costs and no X-ray exposure. Nevertheless, a number of potential complications of RFA have been described, occurring with a rate of almost 9%[3], including liver abscess, ascites, pleural effusion, skin burn, hypoxemia, pneumothorax, subcapsular hematoma, hemoperitoneum, liver failure, and tumour seeding. In addition, biliary lesions have been described in 1% of a large number of patients included in a review of the literature in this field[3], and two case reports describing enterobiliary[4] and biliary pleural[5] fistulae have been published so far.
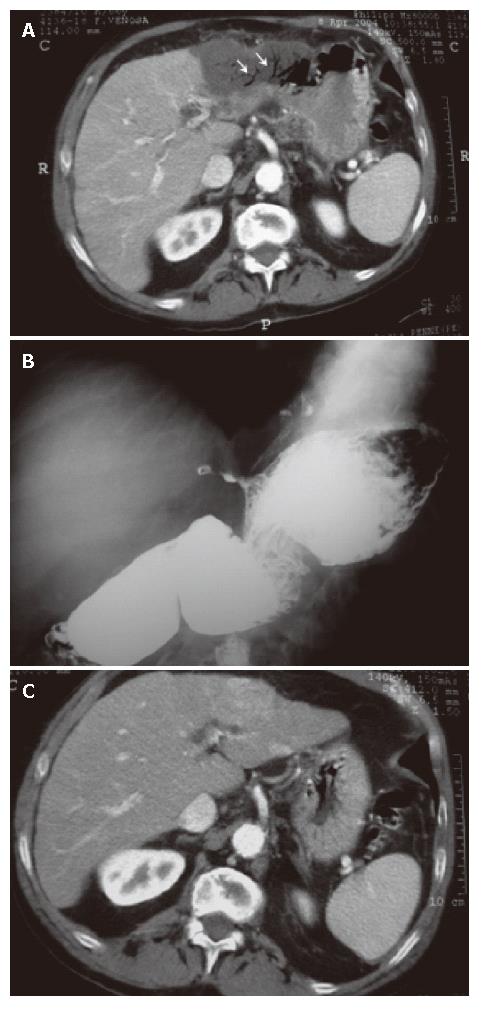
Here we describe a case of biliary gastric fistula occurred in a 66-year old man with a Child’s class A alcoholic liver cirrhosis as a complication of RFA of a large (4.0 cm × 4.5 cm) hepatocellular carcinoma (HCC) lesion in the III segment. Written informed consent was obtained from the patient before treatment. The ablation was performed under US-guidance [Eidos (EUB-525), Esaote, Genova, Italy] using a 3.5 MHz sector probe, with a lateral guide for electrode placement. The treatment was made under general anesthesia using a 20-cm long, 18-gauge electrode to apply the RF current (MIRAS RC, Invatec Italia, Brescia, Italy). The procedure lasted 30 min without apparent complications. In the night following the intervention, the patient experienced transient retching, responsive to metoclopramide administration, and moderate abdominal pain. An enhanced computed axial tomography (CT) scan of the abdomen, performed 22 d after the procedure, showed the presence of aerobilia within the left portion of the liver attributed to a biliary gastric fistula (Figure 1A). A subsequent conventional contrast-enhanced study of the first gastrointestinal tract, showed a fistulous tract starting from the lesser curvature of the stomach with concomitant spasm of the greater curvature, causing a communication with the left portion of the liver (Figure 1B).
Biliary gastric fistulae can be diagnosed on the basis of both direct and indirect radiological signs. The diagnosis with indirect radiological criteria was made by enhanced CT. The presence of aerobilia confined to the left portion of the liver (Figure 1A), in the absence of surgery for biliary-digestive by-pass procedures and the fact that the thermoablative treatment was performed after a previous CT in which the fistula was not present (Figure 1C), led to the hypothesis of a iatrogenic alteration. This was confirmed by a conventional contrast-enhanced study of the first gastrointestinal tract, showing a fistulous tract starting from the lesser curvature of the stomach with concomitant spasm of the greater curvature, causing a communication with the left portion of the liver (Figure 1B).
Perforation of the gastrointestinal tract, a possible major complication of RFA of hepatic nodules, can be difficult to recognize as its clinical manifestations can be attributed to the normal course of the so called “post-ablation syndrome”. Indeed, mild to moderate abdominal pain is not uncommon after RFA of large lesions, particularly when they abut the Glisson’s capsule containing nerve endings.
We describe here for the first time in the literature a case of biliary gastric fistula as a possible complication of thermal ablation of HCC lesions. A recent study has shown the efficacy and safety of percutaneous RFA of HCC abutting the gastrointestinal tract[6]. Nevertheless, in the light of this case and previous descriptions of enterobiliary fistulae occurred following the same therapeutic modality, RFA with injection of saline between the liver and adjacent gastrointestinal tract, as well as laparoscopic RFA, PEI, or other techniques such as chemoembolization, appear to be more indicated than percutaneous RFA for large lesions close to the gastrointestinal tract.
| 1. | Rossi S, Buscarini E, Garbagnati F, Di Stasi M, Quaretti P, Rago M, Zangrandi A, Andreola S, Silverman D, Buscarini L. Percutaneous treatment of small hepatic tumors by an expandable RF needle electrode. AJR Am J Roentgenol. 1998;170:1015-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 397] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 2. | Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Ierace T, Solbiati L, Gazelle GS. Hepatocellular carcinoma: radio-frequency ablation of medium and large lesions. Radiology. 2000;214:761-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 806] [Cited by in RCA: 742] [Article Influence: 28.5] [Reference Citation Analysis (1)] |
| 3. | Mulier S, Mulier P, Ni Y, Miao Y, Dupas B, Marchal G, De Wever I, Michel L. Complications of radiofrequency coagulation of liver tumours. Br J Surg. 2002;89:1206-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 540] [Cited by in RCA: 497] [Article Influence: 20.7] [Reference Citation Analysis (1)] |
| 4. | Bessoud B, Doenz F, Qanadli SD, Nordback P, Schnyder P, Denys A. Enterobiliary fistula after radiofrequency ablation of liver metastases. J Vasc Interv Radiol. 2003;14:1581-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Liberale G, Delhaye M, Ansay J, Houben JJ, Coppens E, Gelin M, Donckier V. Biliary pleural fistula as a complication of radiofrequency ablation for liver metastasis. Acta Chir Belg. 2004;104:448-450. [PubMed] |
| 6. | Choi D, Lim HK, Kim MJ, Kim SH, Lee WJ, Kim SH, Lim JH, Paik SW, Koh KC, Yoo BC. Therapeutic efficacy and safety of percutaneous radiofrequency ablation of hepatocellular carcinoma abutting the gastrointestinal tract. AJR Am J Roentgenol. 2004;183:1417-1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
S- Editor Wang J L- Editor Wang XL E- Editor Liu WF