Published online Sep 7, 2007. doi: 10.3748/wjg.v13.i33.4529
Revised: May 5, 2007
Accepted: May 12, 2007
Published online: September 7, 2007
Patients suffering from hepatocellular carcinoma (HCC) with tumor thrombus in the portal vein generally have a poor prognosis. Portal vein tumor thrombus must be distinguished from portal vein blood thrombus, and this identification plays a very important role in management of HCC. Conventional imaging modalities have limitations in discrimination of portal vein tumor thrombus. The application of positron emission tomography (PET) with 18F-fluorodeoxyglucose (18F-FDG) for discrimination between tumor extension and blood thrombus has been reported in few cases of HCC, while portal tumor thrombosis and portal vein clot identified by 18F-FDG PET/CT in HCC patients has not been reported so far. We present two HCC cases, one with portal vein tumor thrombus and one thrombosis who were identified with 18F-FDG PET/CT. This report illustrates the complimentary value of combining the morphological and functional imaging in achieving a correct diagnosis in such clinical situations.
- Citation: Sun L, Wu H, Pan WM, Guan YS. Positron emission tomography/computed tomography with 18F-fluorodeoxyglucose identifies tumor growth or thrombosis in the portal vein with hepatocellular carcinoma. World J Gastroenterol 2007; 13(33): 4529-4532
- URL: https://www.wjgnet.com/1007-9327/full/v13/i33/4529.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i33.4529
Hepatocellular carcinoma (HCC) has a dismal prognosis and carries a high risk of invasion of the portal vein[1]. Contrast CT and MRI markedly increase the detection rate of portal vein tumor thrombus, especially in small branches of the portal vein by its contrast enhancement features in cross-sectional images. However, all the noninvasive techniques currently used are imperfectly able to differentiate portal vein tumor thrombus from portal vein blood thrombus, and relying exclusively on contrast enhancement characteristics to make a conclusion runs the risk of misdiagnosis due mainly to the intrinsic limitations of the imaging modalities themselves[2]. This pattern of positron emission tomography/computed tomography (PET/CT) has been reported in cases of several types of malignant tumors[3], while portal vein tumor growth and portal vein thrombosis identified by PET/CT in hepatocellular carcinoma patients have not been reported so far. We herein present two cases identified by PET/CT with 18F-fluorodeoxyglucose (18F-FDG), which differentiates portal vein tumor thrombus from blood clot by recognizing different metabolic neoplastic activities and macromorphological characteristics.
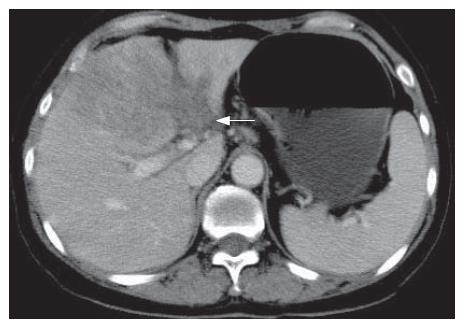
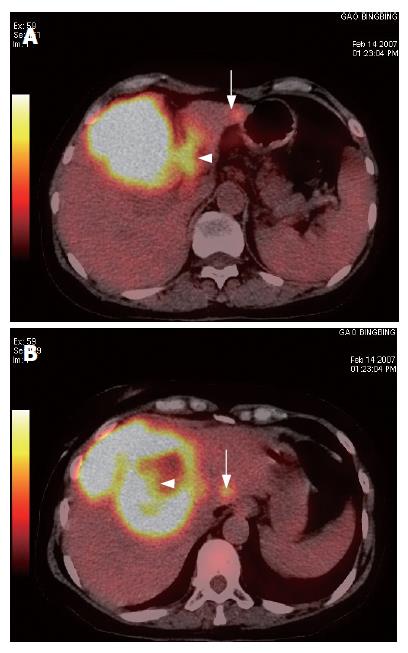
A 60-year-old woman with a five-year history of non-Hodgkin’s lymphoma and hepatitis B virus infection was detected with a liver mass by ultrasound. She reported no vomiting, fever, diarrhea, or weight loss. On physical examination, abdomen was normal except for tender in the left liver area on palpation. Serum alpha fetoprotein (AFP) level was more than 1000 ng/mL, and HBsAg, HBeAb and HBcAb all were positive. Contrast-enhanced CT showed a mass with satellite lesions, and the left portal vein was not revealed clearly on the portal phase (Figure 1). A distinct lesion with high 18F-FDG uptake was demonstrated in the region of the left portal vein (Figure 2A). The 18F-FDG PET/CT showed a mass of high 18F-FDG uptake with satellite lesions and lower metabolism in the central necrotic area (Figure 2B). HCC was confirmed by liver biopsy. It is suggested that 18F-FDG PET/CT may have a great potential value to discriminate tumor thrombus from blood thrombus and to detect satellite or metastatic lesions in patients suffering from HCC. The patient underwent once transcatheter arterial chemoembolization (TACE) and her conditions were relatively stable at the 2-mo follow-up.
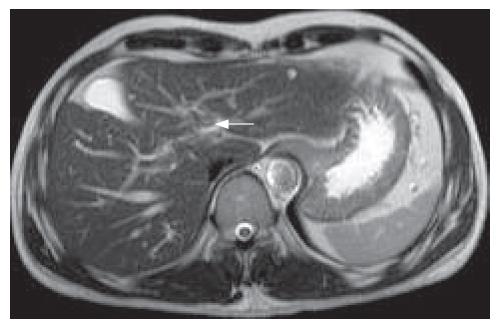
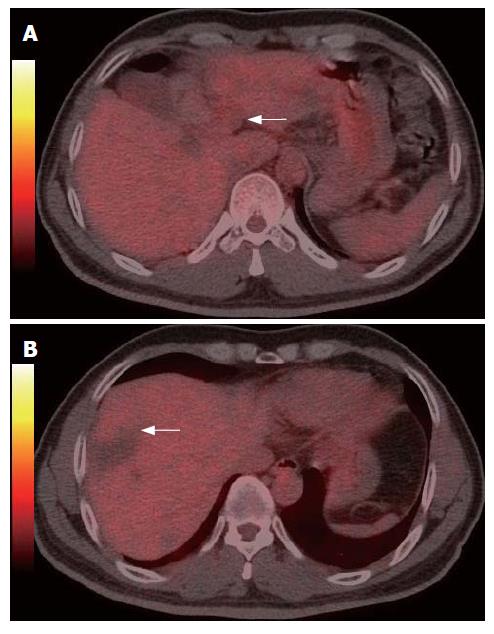
A 50-year-old man with hepatitis B virus infection for 20 years was detected by ultrasound to have a portal block 6 mo after HCC resection. Blood thrombus was suspected on contrast CT and MRI. Physical examination showed no abnormal abdominal findings. AFP level was less than 20 ng/mL and contrast-enhanced MRI demonstrated a thrombus in the left portal vein (Figure 3). Thus a portal vein tumor growth was suspected, with the necessity to differentiate it from portal vein blood thrombosis. Subsequently, the 18F-FDG PET/CT revealed neither a lesion with high FDG uptake in the left portal vein (Figure 4A), nor such a lesion at the margin of previously resected hepatic region (Figure 4B). No distant metastatic lesions were found in the whole-body PET/CT scan. The patient underwent 5-mo follow-up of ultrasound examination, which produced normal results when checking the region for interpretation of the previously abnormal findings. The patient remained well during another 5-mo follow-up period and the thrombus disappeared on the latest ultrasound examination. Thus a diagnosis of the left portal vein blood thrombus was established at last.
Patients suffering from HCC with portal vein tumor thrombus generally have a poor prognosis, as tumor proliferation is often rapid and accompanied by intrahepatic metastases, liver dysfunction, portal hypertension and esophageal varices[4]. Conventional imaging modalities have limitations in discriminating portal vein tumor thrombus. The application of 18F-FDG PET for discrimination between tumor extension and blood thrombus has been reported in few cases of HCC, while portal vein tumor thrombus and portal vein blood clot identified by 18F-FDG PET/CT in HCC patients have not been reported so far. Compared with conventional CT and MRI, PET/CT with 18F-FDG as a radiotracer has some advantages in evaluation of hepatic malignancies, including diagnosing, staging and restaging tumors, evaluating biologic characters, making up treatment plan and monitoring tumor response, early detecting of recurrence and providing prognosis assessment. PET/CT is getting more and more widely applicable in clinical practice with combined functional and anatomical images. With lower false-positive and false-negative rate, it is more sensitive and specific than PET alone[5].
Hanajiri et al[6] and Beadsmooreet et al[7] found that 18F-FDG PET was more sensitive than conventional CT and MRI in detecting suspected vein tumor thrombus in patients with HCC, although portal vein tumor thrombus and portal vein blood thrombus identified by PET/CT in HCC patients have not been reported thus far. Tumor thrombus differentiates itself from blood thrombus by its intense uptake of 18F-FDG as a result of its high metabolic neoplastic activity. Histological grade of differentiation and macroscopic vascular invasion are strong predictors of both survival and recurrence of tumor in patients with cirrhosis who have received transplants because of HCC. Cillo et al[8] reported that using HCC grades (grade 1 and 2) based on preoperative fine-needle aspiration biopsy to select candidates for liver transplantation was associated with an extremely low rate of tumor recurrence which was comparable with that of incidentally detected HCC. Although HCC accumulates 18F-FDG to various degrees, a high positive rate of 18F-FDG accumulation has been reported in patients with high-grade HCC[9] and in those with markedly elevated AFP levels. The standardized uptake value (SUV) ratio is related significantly to disease-related deaths as well as other predictive factors, including the number, size and stage of tumors, involvement of vessels and involvement of the capsule, and provides information about prognostic relevance in patients with HCC before surgery[10].
As to our first case, the PET/CT examination not only confirmed the diagnosis of portal vein tumor thrombus, but also suggested the low grade of cell histology that was confirmed by the results of liver biopsy. Histological examination using percutaneous needle biopsy could be the most definite assessment of HCC grades. However, it is invasive and the specimen retrieved does not always represent the entire lesion owing to sampling errors. Histological grade and vascular invasion cannot be determined preoperatively[11]. Case 1 showed that 18F-FDG PET/CT might have a great potential in discriminating tumor thrombus and blood thrombus and in detecting satellite or metastatic lesions in patients suffering from HCC. It may play an important role in evaluating biologic characters of tumors.
In the second patient, there was no high metabolic lesion in the left portal vein area and in the region of previous hepatic resection. In addition, the whole body PET/CT examination found neither intra-hepatic nor extra-hepatic lesions; an overall 10-mo follow-up confirmed the diagnosis of blood thrombus. 18F-FDG PET has been proved an effective whole-body imaging technique that detects metabolic changes preceding structural findings. Unexplained rise of serum AFP levels in HCC patients after the treatment of their malignancy is an early indicator of tumor recurrence or extra-hepatic metastases[12]. 18F-FDG PET/CT provides fused images that demonstrate the complementary roles of functional and anatomic assessment in the diagnosis of cancer recurrence by the precise localization of suspected foci with 18F-FDG uptake whose characterization can be interpreted as malignant or benign. 18F-FDG PET/CT is better than conventional CT in judging tumor residue of HCC after treatment, and in guiding further treatment of HCC.
We reported two cases of HCC, one with a portal vein tumor thrombus and the other with a portal vein blood thrombus; both were identified by 18F-FDG PET/CT. Thus it demonstrates the complimentary value of morphological and functional imaging in achieving a correct differentiation. PET/CT with 18F-FDG as a radiotracer may further enhance the HCC diagnostic algorithm by accurate diagnosis, staging, restaging and evaluating its biological characters.
| 1. | Ikai I, Hatano E, Hasegawa S, Fujii H, Taura K, Uyama N, Shimahara Y. Prognostic index for patients with hepatocellular carcinoma combined with tumor thrombosis in the major portal vein. J Am Coll Surg. 2006;202:431-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Kurtovic J, Van Der Wall H, Riordan SM. FDG PET for discrimination between tumor extension and blood thrombus as a cause for portal vein thrombosis in hepatocellular carcinoma: important role in exclusion of transplant candidacy. Clin Nucl Med. 2005;30:408-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Lai P, Bomanji JB, Mahmood S, Nagabhushan N, Syed R, Gacinovic S, Lee SM, Ell PJ. Detection of tumour thrombus by 18F-FDG-PET/CT imaging. Eur J Cancer Prev. 2007;16:90-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Schöniger-Hekele M, Müller C, Kutilek M, Oesterreicher C, Ferenci P, Gangl A. Hepatocellular carcinoma in Central Europe: prognostic features and survival. Gut. 2001;48:103-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 171] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | von Schulthess GK, Steinert HC, Hany TF. Integrated PET/CT: current applications and future directions. Radiology. 2006;238:405-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 438] [Cited by in RCA: 394] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 6. | Hanajiri K, Mitsui H, Maruyama T, Kondo Y, Shiina S, Omata M, Nakagawa K. 18F-FDG PET for hepatocellular carcinoma presenting with portal vein tumor thrombus. J Gastroenterol. 2005;40:1005-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Beadsmoore CJ, Cheow HK, Sala E, Lomas DJ, Gibbs P, Save V, Alison ME, Balan KK. Hepatocellular carcinoma tumour thrombus in a re-canalised para-umbilical vein: detection by 18-fluoro-2-deoxyglucose positron emission tomography imaging. Br J Radiol. 2005;78:841-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Cillo U, Vitale A, Bassanello M, Boccagni P, Brolese A, Zanus G, Burra P, Fagiuoli S, Farinati F, Rugge M. Liver transplantation for the treatment of moderately or well-differentiated hepatocellular carcinoma. Ann Surg. 2004;239:150-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 258] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 9. | Hatano E, Ikai I, Higashi T, Teramukai S, Torizuka T, Saga T, Fujii H, Shimahara Y. Preoperative positron emission tomography with fluorine-18-fluorodeoxyglucose is predictive of prognosis in patients with hepatocellular carcinoma after resection. World J Surg. 2006;30:1736-1741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 90] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Seo S, Hatano E, Higashi T, Hara T, Tada M, Tamaki N, Iwaisako K, Ikai I, Uemoto S. Fluorine-18 fluorodeoxyglucose positron emission tomography predicts tumor differentiation, P-glycoprotein expression, and outcome after resection in hepatocellular carcinoma. Clin Cancer Res. 2007;13:427-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 153] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 11. | Yang SH, Suh KS, Lee HW, Cho EH, Cho JY, Cho YB, Yi NJ, Lee KU. The role of (18)F-FDG-PET imaging for the selection of liver transplantation candidates among hepatocellular carcinoma patients. Liver Transpl. 2006;12:1655-1660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 130] [Article Influence: 6.5] [Reference Citation Analysis (1)] |
S- Editor Zhu LH L- Editor Kumar M E- Editor Lu W