Published online Sep 7, 2007. doi: 10.3748/wjg.v13.i33.4520
Revised: June 1, 2007
Accepted: June 9, 2007
Published online: September 7, 2007
A 78-year-old man with liver cirrhosis was found to have multiple hepatocellular carcinomas (HCCs) and underwent 3 sessions of transcatheter arterial chemoembolization. Fourteen months after diagnosis, the patient presented with left hemiparesis. Contrast-enhanced magnetic resonance imaging showed multiple metastases with ring-shaped enhancement in the cerebrum and cerebellum. There were no metastases to other organs. The metastatic lesions almost completely disappeared after whole-brain radiotherapy with a total dose of 50 Gy. Neurologic symptoms decreased, and the patient’s quality of life improved. The patient underwent 2 more sessions of transcatheter arterial chemoembolization. Twelve months after the diagnosis of brain metastasis, the patient remains alive. The present case indicates that radiotherapy can improve quality of life and prolong survival in some patients with brain metastases from HCCs.
- Citation: Toshikuni N, Morii K, Yamamoto M. Radiotherapy for multiple brain metastases from hepatocellular carcinomas. World J Gastroenterol 2007; 13(33): 4520-4522
- URL: https://www.wjgnet.com/1007-9327/full/v13/i33/4520.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i33.4520
Hepatocellular carcinoma (HCC) is one of the most common malignancies in Asian countries, including Japan[1]. Although recent advances in treatment have helped prolong the survival of patients with HCC, they consequently increase the risk of intrahepatic recurrence and extrahepatic metastasis. The most frequent sites of extrahepatic metastasis are the lung, bone, lymph nodes and adrenal glands[2,4]. Brain metastasis is rare: it is found at autopsy in 2.2% of cases of HCC in Japan[5]. The extremely poor prognosis of patients with brain metastasis is a significant problem. A recent study of a large number of patients reported a median survival time of only 1 mo[6]; other studies have reported similar results[7,8]. Furthermore, quality of life (QOL) is decreased because of neurologic symptoms, such as headache, mental change and hemiparesis/hemiplegia, and many patients die of neurologic causes[6,7]. Radiotherapy is a possible treatment for brain metastasis, but its efficacy remains unclear. This paper reports a case of multiple brain metastases from HCCs, for which whole-brain radiotherapy had a dramatic therapeutic effect.
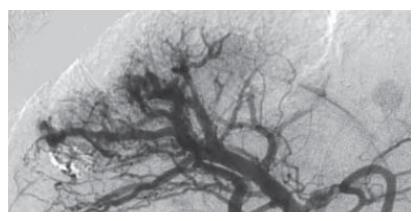
A 78-year-old man had visited a hospital for treatment of liver cirrhosis for more than 10 years. Tests for both hepatitis B surface antigen and antibodies to hepatitis C virus were negative. A routine contrast-enhanced computed tomography (CT) examination revealed multiple HCCs. The patient underwent transcatheter arterial chemoembolization (TACE). Four months later, he visited our hospital. The HCCs were not suitable for resection or ablation because of their number, size and location. Accordingly, the patient underwent 2 more sessions of TACE (Figure 1). Twelve months later, endoscopic sclerotherapy was performed for esophageal varices.
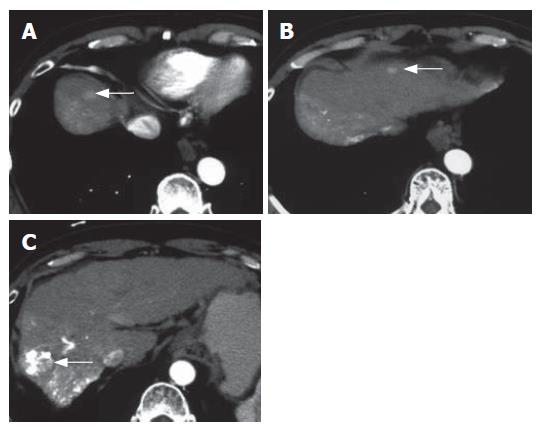
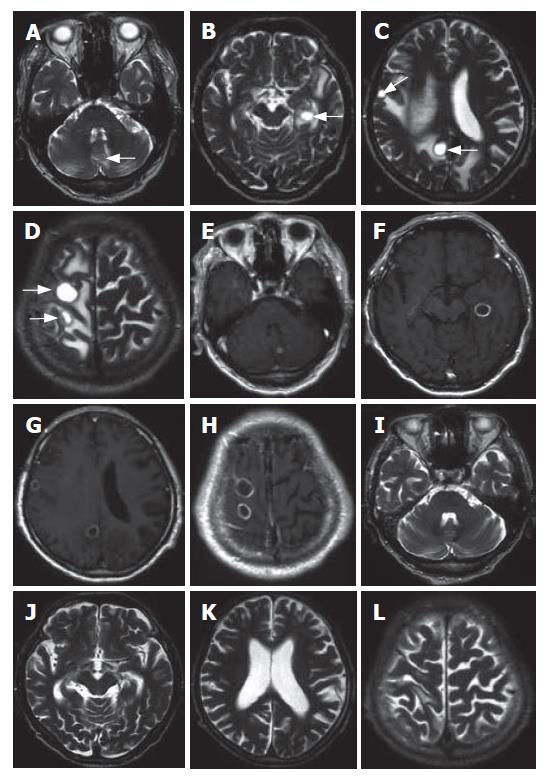
Fourteen months later, contrast-enhanced CT showed multiple enlarged HCCs (Figure 2). Laboratory data were as follows: aspartate aminotransferase, 28 IU/L (normal, 8-35 IU/L); alanine aminotransferase, 15 IU/L (normal, 5-43 IU/L); lactate dehydrogenase, 220 IU/L (normal, 106-211 IU/L); alkaline phosphatase, 191 IU/L (normal, 104-338 IU/L); γ-glutamyl transpeptidase, 35 IU/L (normal, 5-50 IU/L); total bilirubin, 0.8 mg/dL (normal, 0.3-1.1 mg/dL); albumin, 4.1 g/dL (normal, 3.8-5.1 g/dL); prothrombin time, 67% (normal, 70%-130%) (Child-Pugh score 5; class A). The serum levels of alpha-fetoprotein and des-gamma-carboxy prothrombin were 113.7 ng/mL (normal, < 10 ng/mL) and 217 mAU/mL (normal, < 40 mAU/mL), respectively. At that time, the patient was admitted to our hospital for the treatment of HCC. On admission, he complained of gradual and progressive left hemiparesis of 1 mo duration. Unenhanced magnetic resonance (MR) revealed 12 tumors, less than 2 cm in diameter, in the cerebrum and cerebellum; these tumors showed hypointensity on T1-weighted MR images and hyperintensity on T2-weighted MR images (Figure 3A-D). On contrast-enhanced MR with gadolinium-DTPA, the tumors showed ring-shaped enhancement (Figure 3E-H). On the basis of the results of chest and abdominal CT, endoscopic examinations, and bone scintigraphy, the brain tumors were diagnosed as metastases from HCCs; there were no metastases to other organs, including lung, bones, lymph nodes and adrenal glands. The patient received whole-brain radiotherapy with a total dose of 50 Gy in 25 fractions over 5 wk. Most metastatic lesions shrank immediately after radiotherapy. Three months after the completion of radiotherapy, the tumors had almost completely disappeared (Figure 3I-L). Neurologic symptoms had almost completely resolved and the patient’s QOL had improved. No severe acute or late radiologic toxicity was observed. The patient underwent 2 more sessions of TACE. Hepatic functional reserve was good during the clinical course (Child-Pugh score 6 to 7). Twenty-three months after initial diagnosis, the patient stopped attending our hospital. Twenty-six months after the initial diagnosis of HCC, and 12 mo after the diagnosis of brain metastasis, the patient is alive and receiving supportive treatment at the original hospital.
Patients with brain metastasis from HCCs generally have advanced intrahepatic disease[7], and most patients have simultaneous metastases to other sites, usually the lung[7,8]. On the other hand, cases of brain metastasis from early-stage HCCs[9] or without other extrahepatic metastases[9,10] are occasionally reported. Clinicians should consider the possibility of brain metastasis from HCCs whenever neurologic symptoms develop in patients with HCC.
Recent studies have found that brain metastases from HCCs show homogeneous or ring-shaped enhancement on contrast-enhanced imaging[7]. The enhancement pattern of the present case was ring-shaped, which may be due to the central necrosis of tumors[7]. Brain metastases from HCCs tend to bleed in proportion to the size of the tumor[8]. MR is useful for distinguishing such tumoral hemorrhage from nontumoral hemorrhage[8].
Most patients with extrahepatic metastases from HCCs die of primary HCC or hepatic failure rather than the metastases because of the advanced stage of intrahepatic disease or poor hepatic functional reserve, or both[4]. Such outcomes imply that active treatment for metastasis might not prolong survival unless the primary HCC is controlled and the hepatic functional reserve is good. In addition to shortening survival, extrahepatic metastasis often decreases QOL. It is therefore worth considering active treatment for metastasis in such cases regardless of prognosis.
There is no established therapeutic strategy for brain metastasis from HCCs. Craniotomy, radiotherapy or both are commonly performed. Chang et al[6] reported that patients with brain metastases who receive craniotomy, radiotherapy or both survive longer than patients who receive supportive care only (more than 4 mo compared with less than 1 mo). Chen et al[11] reported that clinical improvement associated with a stable lesion is observed in patients with brain metastasis who receive radiotherapy. On the other hand, Kim et al[12] reported that radiotherapy fails to stabilize the condition of patients with brain metastasis: the cause of death in most patients is progressive cachexia or hepatic failure. The applicability of radiotherapy should be carefully determined in each case from the viewpoints of prognosis and QOL. Recently, stereotactic radiosurgery has increasingly been used with or without whole-brain radiotherapy for the treatment of brain metastasis[13]. Future studies will be required to select an appropriate radiation method according to the number and sizes of metastatic lesions in the brain.
Possible reasons why the present patient survived for a long time after the diagnosis of brain metastases are as follows. First, the brain metastases did not cause life-threatening conditions, such as brain herniation or massive cerebral hemorrhage. Second, radiotherapy had a dramatic therapeutic effect on the brain metastases. Third, there were no other life-threatening extrahepatic metastases. Fourth, the primary HCCs could be controlled with repeated TACE, and hepatic functional reserve was good.
In conclusion, radiotherapy can improve QOL and prolong survival in some patients with brain metastases from HCCs. Further studies should be performed to establish a therapeutic strategy using radiotherapy for such patients.
The authors thank Dr. Yoji Shimizu, Dr. Kazuya Takahashi and Dr. Shigeo Nakamura, Department of Neurosurgery, Himeji Red Cross Hospital, for diagnosing the brain metastases and evaluating the therapeutic effects of radiotherapy.
| 1. | McGlynn KA, London WT. Epidemiology and natural history of hepatocellular carcinoma. Best Pract Res Clin Gastroenterol. 2005;19:3-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 250] [Article Influence: 11.9] [Reference Citation Analysis (1)] |
| 2. | Katyal S, Oliver JH, Peterson MS, Ferris JV, Carr BS, Baron RL. Extrahepatic metastases of hepatocellular carcinoma. Radiology. 2000;216:698-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 520] [Article Influence: 20.0] [Reference Citation Analysis (1)] |
| 3. | Natsuizaka M, Omura T, Akaike T, Kuwata Y, Yamazaki K, Sato T, Karino Y, Toyota J, Suga T, Asaka M. Clinical features of hepatocellular carcinoma with extrahepatic metastases. J Gastroenterol Hepatol. 2005;20:1781-1787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 402] [Article Influence: 19.1] [Reference Citation Analysis (1)] |
| 4. | Uka K, Aikata H, Takaki S, Shirakawa H, Jeong SC, Yamashina K, Hiramatsu A, Kodama H, Takahashi S, Chayama K. Clinical features and prognosis of patients with extrahepatic metastases from hepatocellular carcinoma. World J Gastroenterol. 2007;13:414-420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 272] [Cited by in RCA: 353] [Article Influence: 18.6] [Reference Citation Analysis (1)] |
| 5. | Liver Cancer Study Group of Japan. Survey and follow-up study of primary liver cancer in Japan. Report 10. Acta Hepatol Jpn. 1993;34:805-813 DOI : 10.2957/kanzo.34.805. |
| 6. | Chang L, Chen YL, Kao MC. Intracranial metastasis of hepatocellular carcinoma: review of 45 cases. Surg Neurol. 2004;62:172-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Yen FS, Wu JC, Lai CR, Sheng WY, Kuo BI, Chen TZ, Tsay SH, Lee SD. Clinical and radiological pictures of hepatocellular carcinoma with intracranial metastasis. J Gastroenterol Hepatol. 1995;10:413-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Murakami K, Nawano S, Moriyama N, Sekiguchi R, Satake M, Fujimoto H, Ichikawa T. Intracranial metastases of hepatocellular carcinoma: CT and MRI. Neuroradiology. 1996;38 Suppl 1:S31-S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Tunc B, Filik L, Tezer-Filik I, Sahin B. Brain metastasis of hepatocellular carcinoma: A case report and review of the literature. World J Gastroenterol. 2004;10:1688-1689. [PubMed] |
| 10. | Asahara T, Yano M, Fukuda S, Fukuda T, Nakahara H, Katayama K, Itamoto T, Dohi K, Nakanishi T, Kitamoto M. Brain metastasis from hepatocellular carcinoma after radical hepatectomy. Hiroshima J Med Sci. 1999;48:91-94. [PubMed] |
| 11. | Chen SC, Lian SL, Chuang WL, Hsieh MY, Wang LY, Chang WY, Ho YH. Radiotherapy in the treatment of hepatocellular carcinoma and its metastases. Cancer Chemother Pharmacol. 1992;31 Suppl:S103-S105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Kim M, Na DL, Park SH, Jeon BS, Roh JK. Nervous system involvement by metastatic hepatocellular carcinoma. J Neurooncol. 1998;36:85-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA. 2006;295:2483-2491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1613] [Cited by in RCA: 1648] [Article Influence: 82.4] [Reference Citation Analysis (0)] |
S- Editor Liu Y L- Editor McGowan D E- Editor Yin DH