Published online Aug 28, 2007. doi: 10.3748/wjg.v13.i32.4398
Revised: May 15, 2007
Accepted: May 21, 2007
Published online: August 28, 2007
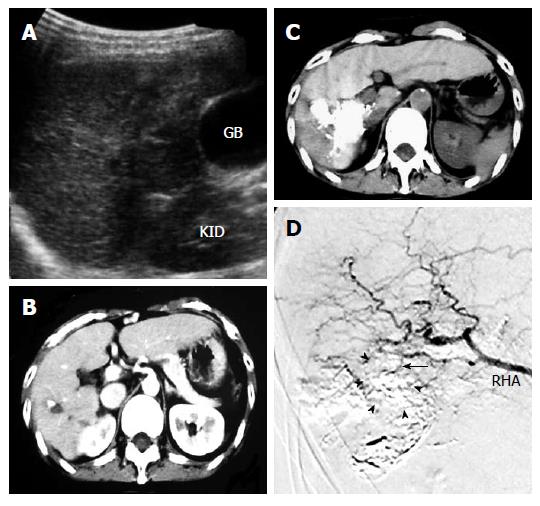
We report a case of hypovascular advanced hepa-tocellular carcinoma (HCC) successfully treated with a novel combination therapy of percutaneous ethanol-lipiodol injection (PELI) and intervention radiology (IVR), lipiodol-targetting IVR (Lipi-IVR). The present case had a hypovascular HCC (3 cm in diameter) located in the S6 region of the liver. Although the tumor was not detectable at all by both of early and late phase of helical dynamic computed tomography (CT), it could be detected by ultrasonography (US) as a low echoic space occupying lesion (SOL) beside the gallbladder and right kidney. Serum levels of alpha fetoprotein (AFP) and AFP-L3 were extremely high. Combination therapy of PELI, firstly reported in our department, and IVR (PELI and IVR, lipiodol-targetting IVR) was performed twice for the treatment. PELI could effectively visualize the location of the tumor for IVR treatment and show the presence of a thin blood vessel branching from the right hepatic artery flowing into the lipiodol deposit. After treatment, the serum levels of AFP and AFP-L3 were rapidly decreased to normal and maintained for more than eight months. Thus, this case expressing the tremendous effect might give us insight into the effectiveness of the novel combination therapy of PELI and IVR for the treatment of hypovascular HCC.
- Citation: Kurokohchi K, Deguchi A, Masaki T, Himoto T, Yoneyama H, Kobayashi M, Maeta T, Kiuchi T, Kohi F, Miyoshi H, Taminato T, Kuriyama S. Successful treatment of hypovascular advanced hepatocellular carcinoma with lipiodol-targetting intervention radiology. World J Gastroenterol 2007; 13(32): 4398-4400
- URL: https://www.wjgnet.com/1007-9327/full/v13/i32/4398.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i32.4398
Hepatocellular carcinoma (HCC) is still one of the most progressive malignancies resistant to treatment[1]. Although several treatment modalities are currently used for the treatment of HCC, radiofrequency ablation (RFA) now plays a central role in local control of hepatic malignancies[2-4]. To improve the therapeutic effects of RFA, we innovated the novel combination therapy of percutaneous ethanol injection and RFA[5-8] and showed that this combination therapy could induce wider coagulated necrosis with smaller energy requirement[9]. Moreover, injection of the mixture of ethanol and lipiodol (PELI) is effective for the treatment of HCC difficult to treat with RFA[10,11]. Although HCC is usually a hypervascular tumor, some HCCs known as hypovascular HCC have no blood vessel. Hypovascular HCC is difficult to treat with intervention radiology (IVR) due to the lack of the feeding artery into the tumor. Here, we report a case of hypovascular HCC totally eliminated with combination therapy of PELI and IVR and normal levels of AFP and AFP-L3 were maintained for a long period of time.
In April, 2006, a 56-year old woman positive for hepatitis B virus was admitted because of a recurrence of HCC. Four years ago, the patient underwent radiofrequency ablation (RFA) therapy for HCC located in the S6 region of the liver. The tumor was eliminated and serum levels of AFP and AFP-L3 were maintained within the normal range over the following four years. However, the levels of AFP and AFP-L3 started to gradually increase at the beginning of 2006. To detect recurrent tumor, helical dynamic computed tomography (CT) and ultrasonography (US) were performed. Although US could detect a low echoic space occupying lesion (SOL) of 3 cm in diameter beside the gallbladder and right kidney (Figure 1A), the tumor was not detectable at all by helical dynamic CT (Figure 1B), indicating that it was not a hypervascular, but a hypovascular HCC. The hypovascularity suggested that the tumor could not be detected by angiography. Consequently, we injected a mixture of ethanol and lipiodol, a technique pioneered in our department in 2004[10,11], by a US-guided approach to mark the main tumor and make it visible in angiography. Plain CT showed a massive lipiodol deposit in the tumor area (Figure 1C). The serum level of of AFP was decreased to 101 ng/mL while the serum level AFP-L3 was unchanged after injection of the mixture of ethanol and lipiodol. An angiogram of the celiac artery, following lipiodol treatment, clearly showed the location of the tumor (Figure 1D, arrow heads) along with a thin vessel branching from the right hepatic artery and flowing into the lipiodol deposit (Figure 1D, arrow). Next, 5-fluorouracil (5-FU) was injected into the thin blood vessel after a super-selective canulation. After 5-FU was injected twice, the serum levels of AFP and AFP-L3 were finally decreased to 2.8 ng/mL and 0%, respectively, in August, 2006. These markers were still within the normal range in April 2007.
Despite intensive efforts to develop treatment modalities for HCC, the prognosis of HCC remains relatively poor[12]. RFA plays a central role in the local control of HCC and a number of attempts have been made to enhance the therapeutic effect of RFA by combining RFA with transcatheter arterial chemoembolization[13,14]. We have recently reported successfully treated HCC cases, of which 1 had diffusely distributed HCC accompanied with tumor thrombus and was treated with combination therapy of 5-FU and pegylated IFN[15]. Another case had a large-size encapsulated lump of HCC and was treated with transarterial chemoembolization followed by the combination of PELI and RFA[16]. The present case had a hypovascular HCC which was different from those previously reported. Although HCC is usually a hypervascular tumor, hypovascular HCC resistant to IVR can still be observed. Logically, administration of anticancer chemical reagents by IVR should not be effective against hypovascular HCC due to a low flow of the arterial blood into the tumor. We modified percutaneous ethanol injection therapy to produce percutaneous ethanol-lipiodol injection therapy (PELIT) for HCC that cannot be imaged by US or CT. By utilizing PELI, the tumor in this patient was made visible by angiography and injection of 5-fluorouracil was sufficient to dramatically decrease both AFP and AFP-L3 levels to the normal range, demonstrating that PELI can reveal the presence of small blood vessels flowing into HCC even though a hypovascular tumor diagnosed by CT and importantly can mark the precise location of the tumor at angiography. Dramatic therapeutic effects seen in this patient may result from the direct tumor targeting by lipiodol or the enhancement of anti-tumor activity of 5-FU by lipiodol. Effect of 5-FU may be enhanced by filling the tumor with lipiodol prior to the injection of 5-FU. Thus, injection of 5-FU after lipiodol injection may open up new avenues for the treatment of advanced HCC. This new technology may be effective for the treatment of both hypovascular and hypervascular HCC. Further study is needed to elucidate it.
S- Editor Zhu LH L- Editor Wang XL E- Editor Ma WH
| 1. | Okuda K. Hepatocellular carcinoma. J Hepatol. 2000;32:225-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 398] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 2. | Curley SA, Izzo F, Ellis LM, Nicolas Vauthey J, Vallone P. Radiofrequency ablation of hepatocellular cancer in 110 patients with cirrhosis. Ann Surg. 2000;232:381-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 574] [Cited by in RCA: 530] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 3. | Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Ierace T, Solbiati L, Gazelle GS. Hepatocellular carcinoma: radio-frequency ablation of medium and large lesions. Radiology. 2000;214:761-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 806] [Cited by in RCA: 742] [Article Influence: 28.5] [Reference Citation Analysis (1)] |
| 4. | Goldberg SN, Gazelle GS, Compton CC, Mueller PR, Tanabe KK. Treatment of intrahepatic malignancy with radiofrequency ablation: radiologic-pathologic correlation. Cancer. 2000;88:2452-2463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Kurokohchi K, Watanabe S, Masaki T, Hosomi N, Funaki T, Arima K, Yoshida S, Miyauchi Y, Kuriyama S. Combined use of percutaneous ethanol injection and radiofrequency ablation for the effective treatment of hepatocelluar carcinoma. Int J Oncol. 2002;21:841-846. [PubMed] |
| 6. | Kurokohchi K, Watanabe S, Masaki T, Hosomi N, Funaki T, Arima K, Yoshida S, Nakai S, Murota M, Miyauchi Y. Combination therapy of percutaneous ethanol injection and radiofrequency ablation against hepatocellular carcinomas difficult to treat. Int J Oncol. 2002;21:611-615. [PubMed] |
| 7. | Kurokohchi K, Masaki T, Watanabe S, Nakai S, Deguchi A, Morishita A, Yoneyama H, Ohgi T, Ono M, Yoshitake A. Time-lag performance of radiofrequency ablation after percutaneous ethanol injection for the treatment of hepatocellular carcinoma. Int J Oncol. 2006;28:971-976. [PubMed] |
| 8. | Kurokohchi K, Hirai S, Ohgi T, Ono M, Yoshitake A, Ebara K, Kitamura Y, Kasai Y, Maeta T, Kiuchi T. Thoracoscopic ethanol injection and radiofrequency ablation for the treatment of hepatocellular carcinoma located immediately under the diaphragm. Int J Oncol. 2006;29:375-380. [PubMed] |
| 9. | Kurokohchi K, Watanabe S, Masaki T, Hosomi N, Miyauchi Y, Himoto T, Kimura Y, Nakai S, Deguchi A, Yoneyama H. Comparison between combination therapy of percutaneous ethanol injection and radiofrequency ablation and radiofrequency ablation alone for patients with hepatocellular carcinoma. World J Gastroenterol. 2005;11:1426-1432. [PubMed] |
| 10. | Kurokohchi K, Masaki T, Miyauchi Y, Hosomi N, Yoneyama H, Yoshida S, Himoto T, Deguchi A, Nakai S, Inoue H. Efficacy of combination therapies of percutaneous or laparoscopic ethanol-lipiodol injection and radiofrequency ablation. Int J Oncol. 2004;25:1737-1743. [PubMed] |
| 11. | Kurokohchi K, Masaki T, Miyauchi Y, Funaki T, Yoneyama H, Miyoshi H, Yoshida S, Himoto T, Morishita A, Uchida N. Percutaneous ethanol and lipiodol injection therapy for hepatocellular carcinoma. Int J Oncol. 2004;24:381-387. [PubMed] |
| 12. | Bruix J, Hessheimer AJ, Forner A, Boix L, Vilana R, Llovet JM. New aspects of diagnosis and therapy of hepatocellular carcinoma. Oncogene. 2006;25:3848-3856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 112] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 13. | Rossi S, Garbagnati F, Lencioni R, Allgaier HP, Marchianò A, Fornari F, Quaretti P, Tolla GD, Ambrosi C, Mazzaferro V. Percutaneous radio-frequency thermal ablation of nonresectable hepatocellular carcinoma after occlusion of tumor blood supply. Radiology. 2000;217:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 346] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 14. | Buscarini L, Buscarini E, Di Stasi M, Quaretti P, Zangrandi A. Percutaneous radiofrequency thermal ablation combined with transcatheter arterial embolization in the treatment of large hepatocellular carcinoma. Ultraschall Med. 1999;20:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 82] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 15. | Kurokohchi K, Takaguchi K, Kita K, Masaki T, Kuriyama S. Successful treatment of advanced hepatocellular carcinoma by combined administration of 5-fluorouracil and pegylated interferon-alpha. World J Gastroenterol. 2005;11:5401-5403. [PubMed] |
| 16. | Kurokohchi K, Hosomi N, Yoshitake A, Ohgi T, Ono M, Maeta T, Kiuchi T, Matsumoto I, Masaki T, Yoneyama H. Successful treatment of large-size advanced hepatocellular carcinoma by transarterial chemoembolization followed by the combination therapy of percutaneous ethanol-lipiodol injection and radiofrequency ablation. Oncol Rep. 2006;16:1067-1070. [PubMed] |