Published online Aug 28, 2007. doi: 10.3748/wjg.v13.i32.4310
Revised: October 2, 2007
Accepted: October 9, 2007
Published online: August 28, 2007
The development of 5-aminosalicylic acid (5-ASA) therapy as a life long treatment for ulcerative colitis is reviewed from its origins in the 1940s to the present day. The drug was designed to treat rheumatoid arthritis, but was found helpful in the management of nine patients with ulcerative colitis. This discovery preceded the emergence of the clinical trial as a tool for assessing a new drug’s efficacy; as a result it lacked scientific rigour and was selective in its presentation of results. Nevertheless it identified the future cornerstone of therapy in ulcerative colitis. In 1962, the first double blind controlled trial of sulphasalazine was conducted on 40 patients. Outcome measures were subjective and included symptoms and an assessment of the rectal mucosa. In 1973, the first two papers on the role of sulphasalazine in maintenance of remission were published. Both used placebo controls and had a stratified design. Outcomes were measured using “an intention to treat” approach. The British study of 64 patients used both subjective and objective criteria to assess outcomes. Patients on placebo had a relapse rate four times patients on active treatment and this founded the basis for a life long approach to therapy with 5-ASA compounds in ulcerative colitis. However, in 1985, a small “on demand” study of 32 patients suggested this approach might be as effective as continuous treatment. Some support for this view came from an Italian study which showed no benefit to continued treatment for those in remission for two years or more. The central problem these studies identify is that of adherence to treatment in the long-term. Few studies have considered patients’ attitudes to continuous therapy and it is an area that needs further investigation.
- Citation: Moshkovska T, Mayberry J. Duration of treatment with 5-aminosalicylic acid compounds. World J Gastroenterol 2007; 13(32): 4310-4315
- URL: https://www.wjgnet.com/1007-9327/full/v13/i32/4310.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i32.4310
Ulcerative colitis is a debilitating disease of young and middle aged people characterised by recurrent attacks of bloody diarrhea. Its cause is unknown and treatment has been aimed at control rather than cure. By the end of the twentieth century most clinicians advised patients to take 5-aminosalicylic (5-ASA) compounds, such as sulphasalazine or mesalazine, on a twice daily basis. This has become embedded in the guidelines put forward by the British Society of Gastroenterology in 2004: “Lifelong maintenance therapy is generally recommended for all patients, especially those with left sided or extensive disease, and those with distal disease who relapse more than once a year”[1].
The purpose of this review is to critically explore the basis for such treatment. Papers were identified through PubMed using the search words: ulcerative colitis, maintenance, trial, long-term, and non-adherence in different combinations. The references in these papers were then explored for further relevant studies. As a result this paper will look at initial case reports which identified a role for sulphasalazine, its subsequent investigation in clinical trials and more recent questioning of the need for regular treatment. During this review an attempt will be made to investigate the myths that developed around its clinical use and the question that will be addressed is: “Do 5-ASA compounds prevent relapse in ulcerative colitis and how frequently are they taken in practice?”
Sulphasalazine was first made in 1940 in Sweden by the pharmaceutical company Pharmacia. It was probably the first designer drug in medical history. Professor Nana Svartz was interested in developing new therapies for the treatment of infective arthritis and speculated that the sulphur component of the molecule would act as an anti-infective agent while the salicylate constituent would have an anti-inflammatory activity. During clinical work at the Karolinska Institute on the role of this new drug in rheumatoid arthritis, Professor Svartz and her colleagues found patients with ulcerative colitis reported a significant improvement in symptoms[2]. This paper preceded the emergence of the clinical trial as a common method for assessing new drugs. The data she presented were based upon: “my material and represent patients who reacted rapidly or favourably to the treatment”. Svartz recognised that such an approach was selective and excluded patients in whom the drug had failed to be effective. In addition diagnosis depended upon history, radiological interpretation of barium enemas or a visual inspection of the rectal mucosa at proctoscopy. No evidence was presented that the diagnosis had been confirmed with a rectal biopsy or infection excluded through faecal culture. The paper reported nine cases of ulcerative colitis of varying degrees of severity and presented data on stool frequency and shape together with temperature charts. These end points largely reflected the patient’s subjective interpretation of progress on treatment. In two cases the rectal mucosa was examined after successful treatment but the interpretation of an improved appearance was subjective. The doctor was aware the patient had received treatment with a new drug and there had been an apparent clinical improvement. However, criticism needs to be tempered by the fact that the randomised controlled trial (RCT) had not been introduced into the assessment of drug treatment in 1942[3]. The study showed a beneficial effect from sulphasalazine in ulcerative colitis. However, it lacked rigor, was selective in the results presented, with poor case definition, a lack of clear and reproducible end-points and no control group. It was an opportunity to record in some depth through structured interviews the views of patients on this new agent, its benefits and side effects. However, the methodology for recording and interpreting such qualitative data did not then exist within clinical practice.
The concept of a “double-blind controlled trial of sulphasalazine against a placebo in mild cases of ulcerative colitis” was not investigated until 1962[4]. Forty patients were randomly allocated to a treatment or placebo group. There was no attempt to stratify the groups so that they contained patients of similar age and extent of disease. Two outcomes were measured-the patients’ symptoms as reported to an observer and a different observer’s assessment of the rectal mucosa at sigmoidoscopy. These again are subjective measures and where there was a discrepancy between symptoms and mucosal appearance “the final assessment was reached by discussion”. Sixteen of the twenty patients in the treatment group improved compared to eight on placebo. This result was statistically significant and launched the widespread use of sulphasalazine to control ulcerative colitis. Although the study was placebo controlled it was small and outcome measures were subjective. In 1964, a second placebo controlled trial of sulphasalazine was reported from a different centre[5]. It was based on 11 pairs of patients, one of whom received active treatment and the other placebo. It had the same limitations of being small, data were open to patient and observer subjectivity. Despite these limitations, such papers helped establish a central role for 5-ASA compounds, such as sulphasalazine, in the prevention of recurrent attacks of ulcerative colitis. They also generated a new research question, namely for how long should this medication be prescribed.
In 1973, two papers were published on the role of sulphasalazine in maintenance of remission. The Danish study was of 50 patients in remission over a 6 mo period[6]. Half continued to receive sulphasalazine, while the rest were given placebo. Selection was random, but with a stratified design so that both groups had patients with disease of comparable extent and severity. Adherence to therapy was checked with a returned tablet count. However, poor adherence did not exclude a patient from the study. Rather an “intention to treat” approach was used. This added strength to the study and addressed any criticism that adherence was not an important factor in the assessment of long-term treatment programs. At the end of the study recurrence rates were comparable at 29% for those on placebo and 24% in the active group. The definition of recurrence chosen was again subjective and based on rectal bleeding for three days or more than three defecations on five successive days. In contrast, the British study of sixty four patients used both subjective and more objective endpoints, including a blinded assessment of sigmoidoscopic appearance and histology[7]. Patients who had been stable on active treatment for one year were entered into a placebo controlled study of the efficacy of sulphasalazine. Patients on placebo had a relapse rate four times greater than those receiving active treatment with sulphasalazine. The relapse rate amongst patients on active treatment was 12% compared to 55% for those on placebo. The study had a stratified design and the outcome for patients who had been on maintenance treatment for at least three years is of particular interest. The relapse rate for those who continued with active treatment was 13% compared with 58% for those on placebo. It was on the basis of these results that the authors considered that there was: “a good case for continuing maintenance treatment with sulphasalazine indefinitely provided there are no harmful side effects” and so the continuous use of sulphasalazine to maintain remission in ulcerative colitis became accepted practice. Riis et al[6]’s study was based on symptoms, while that of Dissanayake & Truelove[7] depended upon both symptoms and histological criteria. As the criteria used for remission in Dissanayake & Truelove’s study[7] were stricter and consistent with current views that histological remission is a more objective measure it is not surprising that life long 5-ASA therapy became the norm.
In 1985, thirty two patients in remission and on continuous treatment with sulphasalazine were randomly allocated to one of two groups[8]. The first continued with sulphasalazine on a daily basis, while the second only took it for a period of fourteen days if they had symptoms of a recurrence. Progress was followed with regular rectal biopsies and these were scored “blind” for evidence of inflammation. At the end of one year there was no statistical difference in the relapse rate between groups. This clearly suggested that “on demand treatment” may be as effective as regular maintenance therapy. This is an important consideration in the management of chronic conditions. Many people find it difficult to take medication daily, especially if they feel well. If treatment is only needed during a flare-up there is no point pressurising people to take it every day. However, the study was small and may have been of inadequate size to demonstrate any true difference in relapse rates between the groups. Indeed up until this point the whole basis for the long-term management of patients with ulcerative colitis had been based on quantitative research on only 146 patients. Minimal attention was given to any qualitative assessment of the impact of medication on quality of life or to develop a better understanding of patients’ views on taking medication regularly whilst well.
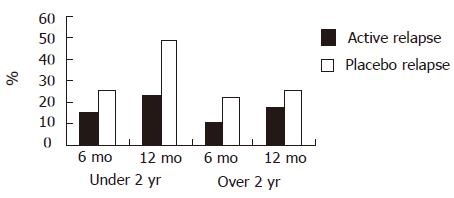
In 2002 Sutherland et al[9] reviewed prospective randomised studies of the effect of oral 5-ASA therapy on maintenance of remission in ulcerative colitis between 1981 and 2002. There were 16 studies which looked at the effectiveness of maintenance therapy for 6 mo or longer. Indeed only one study reviewed a period as long as 18 mo[10]. Based on such studies the current Guidelines of the British Society of Gastroenterology state: “Lifelong maintenance therapy is generally recommended for all patients, especially for those with left sided or extensive disease, and those with distal disease who relapse more than once a year”[1]. Interestingly, until recently there were no studies which used the approach adopted in the investigation of the benefits of long term azathioprine therapy in Crohn’s disease[11,12] and ulcerative colitis[13] (Figure 1).
In 1999, Ardizzone et al[14] conducted such an investigation amongst 112 patients. Patients were stratified into two groups depending upon whether they had been in remission for under two years or over that period. All patients were then randomised to either active treatment with mesalazine or received a placebo. Mesalazine significantly reduced the relapse rate at 12 mo in the group who had been in remission for less than two years. However, active treatment conveyed no advantage to those who had been in remission for more than two years. How much of this effect can be attributed to the high relapse rate of 49% in the placebo group who had been in remission for less than two years is open to some discussion although the difference was not significant. In this study compliance was monitored through use of tablet counts and non-compliance was defined as failing to take less than 80% of the medication. Long duration of treatment is commonly associated with poor adherence to treatment which can at times reach 40%-50%. However, pill counts may fail to detect the true level of lack of adherence to therapy[15]. Indeed the overall relapse rate at 12 mo for patients who had been in remission for less than two years (38%) was not significantly different to that of those in remission for more than two years (22%). Such high rates of relapse certainly raise interesting questions as to patients’ overall adherence to therapy. In view of the fact that maintenance therapy was under investigation the authors used an “intention to treat” approach. This was only the second occasion on which researchers in this field recognised that patient adherence to prolonged therapy could be complicated by their forgetting to take medication or becoming bored or disillusioned with the treatment. Indeed the failure to conduct qualitative research on patients attitude to this therapy meant that the reasons patients might discontinue their treatment were unknown. In this study relapse was defined clinically and based on increased stool frequency and rectal bleeding together with evidence of active disease on sigmoidoscopy. The failure of the investigators to follow the original study plan and recruit eighty six patients compared with the actual sixty one may have led to a falsely significant finding. Indeed, recruitment in the second group was even less near the target size.
Some support for the role of poor adherence comes from a small study of intermittent therapy from Cambridge[8] and the later study of Bardazzi et al[16]. In this twelve month clinical trial in Florence 25 patients received intermittent treatment with 5-ASA tablets for the first week of each month and 25 received continuous treatment. The relapse free rates at 12 mo were 71% in patients on intermittent therapy and 66% in those on continuous treatment. This difference was not significant and suggested that intermittent therapy might be as effective as continuous therapy. However, a particularly interesting aspect of the study is that the overall relapse rate for the 47 patients who completed it was 32%, and this bears direct comparison with the results from Ardizzone[14] and the 36% relapse rate reported by Dickenson et al[8].
In addition to raising questions as to how long and how intensive treatment with 5-ASA compounds should be, these two Italian studies again draw attention to the role of patient adherence. The relapse rates of between 20% and 40% suggest that compliance was probably poor. The Cambridge study of on demand therapy with sulphasalazine showed no difference from regular medication. This tends to suggest that this is how patients on regular treatment use their drugs on demand when symptoms remind them of their need to take treatment.
Clear confirmation of this view comes from Kane et al[17]’s study in Chicago where the prevalence of medication non-adherence was 60% in patients with quiescent ulcerative colitis. Prescription use by three separate populations from a clinic, pharmacy, and telephone callers was investigated. In total, 94 patients were interviewed by a single investigator. No information is given on the type of interview technique used and the only data collected appeared to be demographic. Adherence was defined as “consumption of > 80% of prescribed medication over a six-month period”. This definition was based on the suggestion that loss of more than 20% of patients in a clinical trial makes the results suspect[18]. The choice of this definition for this study was, therefore, arbitrary and not evidence based. Patients who continue to participate in clinical trials may consume less than 80% of prescribed medication. In addition it is “the intention to treat” that is important. Patients may withdraw from a study because an otherwise effective medication has unacceptable side-effects. A better approach would have been to analyse the results at serial levels of consumption e.g. 100%, 90%, 80%, 70% and 60% etc. Univariate analysis was applied to the data and showed non-adherence was significantly associated with male gender, single status, limited disease, and a history of more than four concomitant medications. Of these four factors only the last might be open to clinical alteration. This confirms the limitation of only collecting biodata. No attempt was made to identify those factors which caused men or those with limited disease not to comply with therapy. The simple mantra “Ask the patients” was not utilised by the researchers.
In 2003 a study from Canada again failed to follow this simple mantra[19]. The stated purpose of the study was to investigate determinants of non-adherence amongst 153 patients with inflammatory bowel disease. It used a series of questionnaires to examine whether problems with the therapeutic relationship between these patients and their ten doctors was an important factor. The study was based at one centre in Montreal and data on patient-physician discordance, psychological distress, and social support, as well as non-adherence, were collected using validated questionnaires. No preliminary attempt was made to discover from patients why they might not adhere to treatment plans. Although complete data were only available for 77% of patients the demographic, clinical, and psychosocial characteristics of the non-responders were claimed to be similar. A complex statistical analysis was used to show that 51 of 153 (53%) simply forgot to take their medication, 16 (10%) stopped because they felt better and 13 (8%) worse, with 7% overlap between the groups. Non-adherence was again linked to less active disease and recent diagnosis. Interestingly, for patients who forgot to take their medication there was a link with: “less certainty that medication would positively affect health”.
This again emphasises the generally held belief that patients with ulcerative colitis should take 5-ASA compounds on a regular long-term basis, despite the fact that evidence for this approach is weak. Again, an opportunity was missed for using qualitative techniques, such as in-depth interviews, to investigate patients’ beliefs about 5-ASA compounds, their actual use of them, and reasons for non-adherence. Such a study would have provided an insight into patient practice and helped clarify whether people in the active wing of long-term maintenance studies really take the medication.
Non-adherence has been associated with male gender, being single, and taking multiple concomitant medications. Compliance with an intensive program of medication in ulcerative colitis can prove difficult for a number of patients and several other studies have indicated that pills are often forgotten or taken in a disorganised pattern[19-21]. Studies across a wide range of disciplines have shown that patients who are more satisfied and informed about their care are more likely to be adherent to treatment programs[22].
The level at which patients adhere to their 5-ASA therapy may have particular importance in the reduction of cancer risk in ulcerative colitis. Early work by Jones et al[23] demo-nstrated that the development of colorectal cancer as a complication of long-standing ulcerative colitis might be the result of poor compliance with therapy. Patients who developed cancer in their community based surveillance program were the very patients who failed to attend for their regular colonoscopy. In a 10 year study of 175 patients Moody et al[24] found that the crude proportions developing cancer were 5/152 (3%) in the group who took long-term sulphasalazine but 5/16 (31%) in the those who had had their treatment stopped or who did not comply with therapy. Further support for the value of 5-ASA compounds in cancer prevention comes from the work of Eaden et al[25]. In her study of 102 cases of colorectal cancer complicating ulcerative colitis regular 5-ASA therapy reduced cancer risk by 75% (OR 0.25, 95% CI: 0.13-0.48, P < 0.00001). Adjusting for other variables, taking mesalazine regularly was shown to reduce the risk by 81% (OR 0.19, 95% CI: 0.06-0.61, P = 0.006). These studies emphasise the need for adherence to therapy, but how close and how long must that adherence be? In Pinczowski et al[26]’s study from Sweden of 3012 patients with ulcerative colitis, pharmacological therapy, especially sulfasalazine, lasting at least 3 mo was associated with a significant protective effect (RR, 0.38; 95% CI: 0.20-0.69) independent of disease activity.
The current evidence is that patients with ulcerative colitis are poorly adherent to 5-ASA therapy and that this situation probably worsens with time. Only limited work has been done on those factors which are associated with lack of adherence but male gender and multiple therapies seem to be important. General work on compliance has suggested that education about the role of drugs may lead to greater adherence. Apart from a reduction in morbidity through reduced frequency of flare-ups greater adherence to 5-ASA therapy is likely to reduce the incidence of colorectal cancer as a complication of long term ulcerative colitis. Greater attention to strategies which are associated with higher adherence would therefore seem worthwhile and it may be that in order to achieve this effect it will not be necessary to make certain that their impact is life-long. Any research on adherence will therefore also need to address the issue of the optimum duration and pattern of treatment.
The generally held belief that 5-ASA compounds should be taken regularly and life long is based on a small number of small quantitative studies. In early trials stratification of the active and control groups for severity, extent, and duration of disease was often omitted from the design. End points have usually been subjective and there was often a failure to adequately blind observers. However, the core issue as to whether these medications are actually taken long term has never been investigated directly with patients. Substitute markers, such as returned pill counts, are inaccurate. There have been no in-depth interviews with patients and we have little knowledge about their attitude towards this form of treatment. This should have been the obvious foundation for research on maintenance therapy in ulcerative colitis and its absence calls into question most of the work done on this topic.
Ulcerative colitis is a life long condition characterised by recurrent attacks of diarrhoea, rectal bleeding and abdominal pain. It predisposes the patient to colorectal cancer. Current therapy suggests that treatment should be continuous and throughout life. This review explores the research background to this clinical approach. It identifies the fact that most clinical trials are for short periods and none have exceeded a period of two years. It investigates the basis for continuous therapy and raises questions as to patients compliance with such a regimen.
This review draws attention to the need to explore the effectiveness of long term therapy with 5-ASA compounds and to consider alternatives such as intermittent treatment. This work will need to be linked to a better understanding of what motivates patients’ adherence to such a program and the identification of what patients consider important triggers in ensuring good compliance.
In the 21st century it will be increasingly important to build a therapeutic partnership between patients and their clinicians. This requires good communication and means that the information given to patients must be clearly understood. In the field of gastroenterology, especially amongst patients with chronic disease, there has been limited work in this area. It needs a well structured and rigorous research base. This paper has emphasised the fact that the basis for long term use of 5-ASA compounds is weak. Studies have been over relatively short terms and suggest that adherence in the long term is poor. This review has focused on these weaknesses and will hopefully ensure that a broader approach to adherence is now developed. Although once daily preparations may play a part in better compliance with treatment, they are only one element in the approaches we need to consider and evaluate.
The need to consider the most effective approach to controlling flare-ups and reducing cancer risk in ulcerative colitis is of relevance to all clinicians working in this field and to all patients with this disease. This review draws attention to the need to consider how frequently this medication needs to be taken and to whether adherence can be improved
Ulcerative colitis is an inflammatory condition of the colon. 5-ASA or 5-aminosalicylic acid is a drug which reduces the occurrence of flare-ups and cancer risk. Adherence, congruence, and compliance are terms which describe patients approach to taking medication.
This paper critically investigates the criteria of guidelines for lifelong maintenance therapy with 5-ASA compounds in ulcerative colitis. It is interesting, well written and the criticism raised by the authors is stimulating both for clinical practice and future research.
S- Editor Ma N L- Editor Mihm S E- Editor Li JL
| 1. | Carter MJ, Lobo AJ, Travis SP. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53 Suppl 5:V1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 746] [Cited by in RCA: 774] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 2. | Svartz N. Salazopyrin, a new Sulfanilamide preparation. A. Therapeutic results in rheumatic polyarthritis. B. Therapeutic results in ulcerative colitis. C. Toxic manifestations in treatment with sulphanilamide preparations. Acta.Med Scand. 1942;110:577-598. [RCA] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 155] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 3. | Cochrane AL. Effectiveness and Efficiency. Random Reflections on Health Services. 1st ed. London Nuffield Provincial Hospitals Trust. 1972;21-25. |
| 4. | BARON JH, Connel AM, Lennard-Jones JE, Jones FA. Sulphasalazine and salicylazosulphadimidine in ulcerative colitis. Lancet. 1962;1:1094-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 174] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Dick AP, Grayson MJ, Carpenter RG, Petrie A. Controlled trial of sulphasalazine in the treatment of ulcerative colitis. Gut. 1964;5:437-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 180] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Riis P, Anthonisen P, Wulff HR, Folkenborg O, Bonnevie O, Binder V. The prophylactic effect of salazosulphapyridine in ulcerative colitis during long-term treatment. A double-blind trial on patients asymptomatic for one year. Scand J Gastroenterol. 1973;8:71-74. [PubMed] |
| 7. | Dissanayake AS, Truelove SC. A controlled therapeutic trial of long-term maintenance treatment of ulcerative colitis with sulphazalazine (Salazopyrin). Gut. 1973;14:923-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 245] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Dickinson RJ, King A, Wight DG, Hunter JO, Neale G. Is continuous sulfasalazine necessary in the management of patients with ulcerative colitis? Results of a preliminary study. Dis Colon Rectum. 1985;28:929-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Sutherland L, Roth D, Beck P, May G, Makiyama K. Oral 5-aminosalicylic acid for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2002;CD000544. [PubMed] |
| 10. | Nilsson A, Danielsson A, Löfberg R, Benno P, Bergman L, Fausa O, Florholmen J, Karvonen AL, Kildebo S, Kollberg B. Olsalazine versus sulphasalazine for relapse prevention in ulcerative colitis: a multicenter study. Am J Gastroenterol. 1995;90:381-387. [PubMed] |
| 11. | O'Donoghue DP, Dawson AM, Powell-Tuck J, Bown RL, Lennard-Jones JE. Double-blind withdrawal trial of azathioprine as maintenance treatment for Crohn's disease. Lancet. 1978;2:955-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 203] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Vilien M, Dahlerup JF, Munck LK, Nørregaard P, Grønbaek K, Fallingborg J. Randomized controlled azathioprine withdrawal after more than two years treatment in Crohn's disease: increased relapse rate the following year. Aliment Pharmacol Ther. 2004;19:1147-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Hawthorne AB, Logan RF, Hawkey CJ, Foster PN, Axon AT, Swarbrick ET, Scott BB, Lennard-Jones JE. Randomised controlled trial of azathioprine withdrawal in ulcerative colitis. BMJ. 1992;305:20-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 319] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 14. | Ardizzone S, Petrillo M, Imbesi V, Cerutti R, Bollani S, Bianchi Porro G. Is maintenance therapy always necessary for patients with ulcerative colitis in remission? Aliment Pharmacol Ther. 1999;13:373-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Ley P. Communicating with Patients. Improving Communication Satisfaction and Compliance. 1st ed. London: Routledge 1988; 59-61. |
| 16. | Bardazzi G, d'Albasio G, Bonanomi AG, Trallori G, Messori A, Amorosi A, Bartoletti L, Morettini A, Pacini F. Intermittent versus continuous 5-aminosalicylic acid treatment for maintaining remission in ulcerative colitis. Ital J Gastroenterol. 1994;26:334-337. [PubMed] |
| 17. | Kane SV, Cohen RD, Aikens JE, Hanauer SB. Prevalence of nonadherence with maintenance mesalamine in quiescent ulcerative colitis. Am J Gastroenterol. 2001;96:2929-2933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 318] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 18. | Guyatt GH, Sackett DL, Cook DJ. Users' guides to the medical literature. II. How to use an article about therapy or prevention. B. What were the results and will they help me in caring for my patients? Evidence-Based Medicine Working Group. JAMA. 1994;271:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 341] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 19. | Sewitch MJ, Abrahamowicz M, Barkun A, Bitton A, Wild GE, Cohen A, Dobkin PL. Patient nonadherence to medication in inflammatory bowel disease. Am J Gastroenterol. 2003;98:1535-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 223] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 20. | Rubin GP, Hungin AP, Chinn DJ, Dwarakanath D. Quality of life in patients with established inflammatory bowel disease: a UK general practice survey. Aliment Pharmacol Ther. 2004;19:529-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Stone MA, Mayberry JF, Baker R. Prevalence and management of inflammatory bowel disease: a cross-sectional study from central England. Eur J Gastroenterol Hepatol. 2003;15:1275-1280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 78] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Horne R. Adherence to medication: a review of existing research. Midence K Adherence to Treatment in Medical Conditions. Amsterdam: Taylor and Francis 1998; 285-310. |
| 23. | Jones HW, Grogono J, Hoare AM. Acute colitis in a district general hospital. Br Med J (Clin Res Ed). 1987;294:683-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Moody GA, Jayanthi V, Probert CS, Mac Kay H, Mayberry JF. Long-term therapy with sulphasalazine protects against colorectal cancer in ulcerative colitis: a retrospective study of colorectal cancer risk and compliance with treatment in Leicestershire. Eur J Gastroenterol Hepatol. 1996;8:1179-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 162] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 25. | Eaden J, Abrams K, Ekbom A, Jackson E, Mayberry J. Colorectal cancer prevention in ulcerative colitis: a case-control study. Aliment Pharmacol Ther. 2000;14:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 382] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 26. | Pinczowski D, Ekbom A, Baron J, Yuen J, Adami HO. Risk factors for colorectal cancer in patients with ulcerative colitis: a case-control study. Gastroenterology. 1994;107:117-120. [PubMed] |