Published online Jul 14, 2007. doi: 10.3748/wjg.v13.i26.3610
Revised: April 2, 2007
Accepted: April 18, 2007
Published online: July 14, 2007
AIM: To assess persistent symptoms and mortality in a cohort of patients with severe (grade 3-4) radiation enteropathy, 59 patients were followed up after 15-18 years.
METHODS: Fifty-nine patients were prospectively enrolled by twelve surgical departments. Primary malignant disease, radiation therapy and surgical management were recorded at inclusion. The cause of death or persistence of symptoms was examined in public death records or by interview of survivors.
RESULTS: Thirty-nine patients had received radiation therapy for gynaecological cancers, twelve for urological cancers, four for gastrointestinal cancers and four for other malignancies. Forty-five patients (76%) required surgical intervention. Complications occurred in 11 (25%) operated patients. Forty-seven patients had died at the time of follow-up, seven (12%) died as a direct result of radiation enteropathy, while radiation enteropathy contributed to death in an additional seven patients. Four of the twelve surviving patients suffered from chronic debilitating symptoms of radiation enteropathy, while three had moderate symptoms.
CONCLUSION: Patients with severe delayed radiation enteropathy have a high risk of persistence of symptoms after surgery. At least one in ten patients dies from radiation-induced bowel injury.
- Citation: Larsen A, Reitan JB, Aase ST, Hauer-Jensen M. Long-term prognosis in patients with severe late radiation enteropathy: A prospective cohort study. World J Gastroenterol 2007; 13(26): 3610-3613
- URL: https://www.wjgnet.com/1007-9327/full/v13/i26/3610.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i26.3610
The long-term prognosis of patients with severe intestinal radiation injury (radiation enteropathy) is not well described. Many patients receive symptomatic treatment of malabsorption, diarrhoea and abdominal pain, whereas severe complications like bleeding, fistulas and obstruction may require surgical intervention. Compromised vascularisation of fibrotic tissues contributes to an adverse post-operative outcome and symptoms of radiation enteropathy frequently persist after surgery. In this multi-centre study, 59 patients with a diagnosis of severe (EORTC/RTOG grade 3-4) radiation enteropathy were prospectively enrolled on admission to surgical wards. Details regarding primary tumor site, radiation therapy, gastrointestinal symptoms, initial hospitalization, and subsequent clinical outcome are described.
During the period 1983-1987 the Norwegian Study Group for Gastrointestinal Surgery (NORGAS) prospectively enrolled 59 patients admitted to twelve surgical departments because of severe radiation enteropathy. The primary malignant disease, radiation treatment (RT) and symptoms during RT, risk factors for delayed radiation side effects, and the time from RT to clinical presentation of enteropathy were recorded. At discharge from the hospital, details regarding the surgical treatment, complications and histopathological diagnosis were recorded. Follow-up after 15-18 years consisted of a review of the original prospective data, patient charts, as well as records from the National Public Statistical Services about main and contributing causes of death. The twelve surviving patients were invited to a telephone interview by letter, to be returned with their written consent. Their evaluation of quality of life, health and everyday life consisted of direct questions (e.g., how do you assess your health compared with the time before RT?) to be answered by categories (worse, unchanged, better, much better). Symptoms were graded according to EORTC/RTOG[1]. The study was approved by the Regional Committee for Research Ethics.
Fifty-nine patients (46 women, 13 men), mean age 63 years (range 17-86), were enrolled during the period 1983-1987. The primary malignant diagnoses for which the patients had received radiation therapy were gynaecological cancer (21 cervical cancers, 12 ovarian cancers and 6 endometrial cancers), urological cancer (eight urinary bladder cancers, two prostate cancers and two testicular cancers) and other cancers (two colon cancers, two rectal cancers, two cancers of unknown origin, one Ewings tumour and one Wilms tumour). Possible risk factors for delayed radiation enteropathy included hypertension and diabetes mellitus (one or both) in six patients or a history of abdominal surgery prior to the radiation therapy (36 patients). No risk factor for radiation enteropathy was identified for eighteen of the patients. Smoking history was not recorded. RT had been given at four different hospital facilities up to 30 years previously (mean time between RT and admission 6 years, range 0-30). Twenty-two patients recalled having had severe acute gastrointestinal symptoms during RT. The latency period from RT to clinical presentation of the symptoms that eventually led to hospitalisation was 3.5 years (mean), with a range from no symptom-free interval to 29 years.
Twenty-two patients had been treated with external RT alone, doses ranged from 36 Gy to 72 Gy (mean: 50.5 Gy). Combination of external beam therapy and brachytherapy had been used in 12 patients, and brachytherapy alone in one patient. Four patients with ovarian cancers were treated with intraabdominal instillation of radioactive isotopes of colloidal gold (three patients) or phosphorous (one patient). Three of these patients also received external RT (two patients) or vaginal brachytherapy (one patient). Detailed information about RT was missing in 20 patients. The external RT was typically delivered with 2 Gy fractions, five days a week, treatment duration in the range of 4-7 wk.
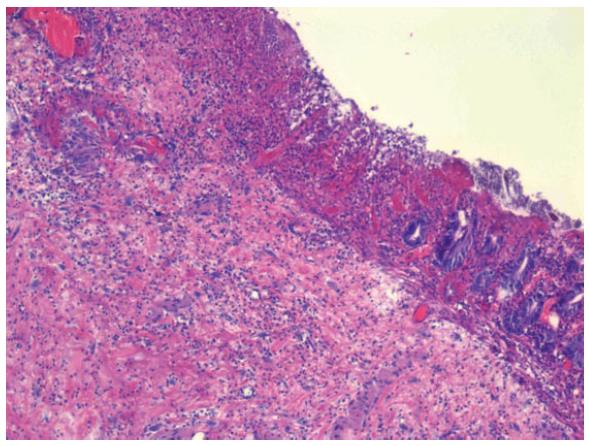
The most frequent admitting diagnoses were bowel obstruction (36 patients) or fistula (13 patients). Other admitting diagnoses included free intestinal perforation (five patients), bleeding (three patients), diarrhoea or malabsorption (one patient each). The median length of hospitalization was 19 d (range 2-67 d). Surgical intervention was required during the initial hospitalization in 45 patients (76%). The operations performed were: resection (17 patients), Hartmanns' procedure (four patients), bypass (seven patients), sigmoidostomy (six patients), transversostomy (four patients), two other enterostomas, three adhesiolysis, and two "other" procedures. Fourteen patients were discharged without surgery. Thirty-seven patients had the diagnosis of radiation enteropathy confirmed by histopathological examination (Figure 1). Histopathologic examination revealed chronic radiation damage in the form of mucosal congestion and oedema, erosions or ulcerations, sometimes necrosis of large areas of mucosa, chronic transmural inflammation, or fibrosis. These alterations often appeared in combination. Fibrosis typically was most pronounced in the submucosa. The types of chronic changes were similar in the small and the large intestine. When no microscopic evaluation had been done, typical features of macroscopic fibrosis and strictures were described by the surgeon. Postoperative complications occurred in eleven patients (24%). One patient died as a consequence of surgery after two months of hospitalization. In this patient, necrosis of a stoma necessitated two reoperations, followed by bronchopneumonia (autopsy diagnosis). Other complications were severe diarrhoea (three patients), wound infection (two patients), delayed recovery (two patients) or fistula, anastomotic leakage or wound dehiscence (one patient each). Seven patients died within six months after the operation; three due to radiation enteropathy, two due to recurrence of the original malignancy (gynaecological cancers), one of pneumonia and one of stroke. The 14 patients that were discharged without surgery were hospitalized because of partial bowel obstruction (five patients), diarrhoea (five patients), fistula (two patients) or gastrointestinal bleeding (two patients).
At the time of follow-up, 47 patients had died with a mean observation time of 6 years (range 0-16). Main causes of death according to the charts are shown in Table 1. Radiation enteropathy was the direct cause of death in seven patients. Modes of impact were short-bowel syndrome, malnutrition and fistula, or not further described. Radiation enteropathy was listed as a contributing cause of death in another seven patients (six of whom had recurrent cancer).
| Causes of death | n |
| Cancer | 21 |
| Radiation enteropathy | 7 |
| Cardiovascular disease | 7 |
| Pneumonia | 3 |
| Other | 6 |
| Lost to follow-up | 3 |
Of the 12 long-time survivors, seven patients accepted the invitation for a telephone interview. During the 15-18 years since being included in the prospective registry, five had had one or more operations because of bowel symptoms. Six had several hospital stays due to fistulas, bowel obstruction, or other problems related to radiation enteropathy. Two had permanent enterostomas, three felt restricted in daily life because of frequent and urgent diarrhoea (grade 2-3), two had moderate defecation problems and the one with normal defecations had severe problems due to persistent fistulas (grade 4). Half of the patients had changed their diet, avoiding fiber-rich food (cabbage, citrus), six used dietary supplements and three had a lower body weight than desired. All patients were able to take a daily walk and did not spend daytime in bed. Five assessed their health, total life situation or quality of life as "worse" than before the RT while two answered "unchanged". No patient chose the category "better". Three patients frequently had worries due to their health situation; e.g. stoma bags falling off fistula openings, urgent need for a toilet or new hospital stays.
This study demonstrates unequivocally that severe delayed radiation enteropathy continues to be a hazard to the patients during their lifetime. Our findings that 7 of 59 patients eventually died as a direct cause of radiation enteropathy, i.e., 12% mortality, is consistent with other reports[2,3] and is likely an underestimate. Moreover, radiation enteropathy was considered a contributing factor in the deaths of another seven patients.
Radiation therapy, alone or combined with other types of treatment, is given to 70% of all cancer patients. Cancer specific survival is improved with higher radiation dose[4], and technical improvements limit exposure of normal tissues like the bowel. Nevertheless, delayed radiation enteropathy continues to be a dose-limiting factor for long-term uncomplicated cancer cure. Prevalence estimates of moderate and severe late bowel effects varies from 5%-30%[5-9].
Reporting the extent of treatment related morbidity and mortality is essential for the progress of RT. Commonly applied reporting systems for the side effects of RT are RTOG/EORTC[1], and the Common Toxicity Criteria version 2.0[10]. According to these systems, four of our patients had severe or invalidating symptoms (grade 3-4) while three suffered from moderate problems 15-27 years after RT. With respect to the influence of symptoms on patients' self-rated quality of life (QOL), our study did not include baseline assessment or a validated instrument to evaluate health-related QOL. The majority of patients selected to enter our study had initially recovered uneventfully from the RT, similarly to most patients undergoing RT. However, when diagnosed with severe radiation enteropathy, the unfavourable prospect of 12% treatment-related mortality applies to this special group of patients.
Predicting the risk of delayed radiation enteropathy was one of the aims at inclusion of this study, focusing on three proposed factors: surgery before RT, preexisting cardiovascular disease, and severe acute GI symptoms during RT. Previous surgery has been shown to increase the risk of late GI toxicity, for example, after RT for prostate cancer[8]. In a study comprising almost 3500 patients irradiated for advanced uterine cervical carcinomas, smoking status was found to be a strong predictor for delayed radiation effects of the intestines, whereas hypertensive disease and diabetes were not[5]. Diabetes mellitus was not associated with late GI toxicity following RT for prostate cancer[11]. Despite recall bias due to a long time from RT to admission to surgical ward, 37% of our patients confirmed having had severe GI symptoms during RT. Clinical studies show increased risk of delayed radiation enteropathy in patients who experience severe acute GI symptoms during RT[6,9,11-15]. Preventing acute symptoms could be a strategy to help reduce the risk of delayed radiation effects, as, for example, attempted by use of prostaglandin analogues or probiotics[16,17].
Radiation enteropathy can be eradicated by surgery in some cases, but palliative surgical or medical interventions are the option of choice for the majority of patients. Both minimal and more extensive surgical interventions carry a high risk of complications because of frequent widespread enteropathy, poor healing, and nutritional derangement. Anastomotic dehiscence and fistula formation are common complications. Adequate resection of affected intestines is recommended whenever possible[3,18]. However, an atraumatic surgical technique and antibiotic prophylaxis are strongly recommended to obtain successful healing of previously irradiated tissues[19].
In conclusion, our study demonstrates that, while operative intervention can cure selected patients with delayed radiation enteropathy, surgery is associated with a significant risk of complications and the long term prognosis remains poor. At least 10% of patients with a diagnosis of severe (grade 3-4) delayed radiation enteropathy die as a direct result of the disorder and most surviving patients suffer from chronic debilitating symptoms that negatively influence their quality of life for decades after RT. There is a need for continued efforts to develop strategies to minimize the incidence and severity of radiation-induced bowel injury.
We thank the Norwegian Study Group for Gastrointestinal Surgery (NORGAS) which made this study possible by recruiting patients and providing part of the information presented here.
| 1. | Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995;31:1341-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3186] [Cited by in RCA: 3584] [Article Influence: 115.6] [Reference Citation Analysis (0)] |
| 2. | Galland RB, Spencer J. Natural history and surgical management of radiation enteritis. Br J Surg. 1987;74:742-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 54] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Regimbeau JM, Panis Y, Gouzi JL, Fagniez PL. Operative and long term results after surgery for chronic radiation enteritis. Am J Surg. 2001;182:237-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 57] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Karlsdottir A, Muren PL, Wentzel-Larsen T, Johannessen DC, Bakke A, Ogreid P, Johan Halvorsen O, Dahl O. Radiation dose escalation combined with hormone therapy improves outcome in localised prostate cancer. Acta Oncol. 2006;45:454-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Eifel PJ, Jhingran A, Bodurka DC, Levenback C, Thames H. Correlation of smoking history and other patient characteristics with major complications of pelvic radiation therapy for cervical cancer. J Clin Oncol. 2002;20:3651-3657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 143] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Jereczek-Fossa BA, Jassem J, Badzio A. Relationship between acute and late normal tissue injury after postoperative radiotherapy in endometrial cancer. Int J Radiat Oncol Biol Phys. 2002;52:476-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Lilleby W, Fosså SD, Waehre HR, Olsen DR. Long-term morbidity and quality of life in patients with localized prostate cancer undergoing definitive radiotherapy or radical prostatectomy. Int J Radiat Oncol Biol Phys. 1999;43:735-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 131] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Peeters ST, Heemsbergen WD, van Putten WL, Slot A, Tabak H, Mens JW, Lebesque JV, Koper PC. Acute and late complications after radiotherapy for prostate cancer: results of a multicenter randomized trial comparing 68 Gy to 78 Gy. Int J Radiat Oncol Biol Phys. 2005;61:1019-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 343] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 9. | Schultheiss TE, Lee WR, Hunt MA, Hanlon AL, Peter RS, Hanks GE. Late GI and GU complications in the treatment of prostate cancer. Int J Radiat Oncol Biol Phys. 1997;37:3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 278] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 10. | Trotti A, Byhardt R, Stetz J, Gwede C, Corn B, Fu K, Gunderson L, McCormick B, Morrisintegral M, Rich T. Common toxicity criteria: version 2.0. an improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys. 2000;47:13-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 600] [Cited by in RCA: 615] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 11. | Geinitz H, Zimmermann FB, Thamm R, Schumertl A, Busch R, Molls M. 3D conformal radiation therapy for prostate cancer in elderly patients. Radiother Oncol. 2005;76:27-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Bourne RG, Kearsley JH, Grove WD, Roberts SJ. The relationship between early and late gastrointestinal complications of radiation therapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 1983;9:1445-1450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 87] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | O'Brien PC, Franklin CI, Poulsen MG, Joseph DJ, Spry NS, Denham JW. Acute symptoms, not rectally administered sucralfate, predict for late radiation proctitis: longer term follow-up of a phase III trial--Trans-Tasman Radiation Oncology Group. Int J Radiat Oncol Biol Phys. 2002;54:442-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Wang CJ, Leung SW, Chen HC, Sun LM, Fang FM, Huang EY, Hsiung CY, Changchien CC. The correlation of acute toxicity and late rectal injury in radiotherapy for cervical carcinoma: evidence suggestive of consequential late effect (CQLE). Int J Radiat Oncol Biol Phys. 1998;40:85-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 118] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Weiss E, Hirnle P, Arnold-Bofinger H, Hess CF, Bamberg M. Therapeutic outcome and relation of acute and late side effects in the adjuvant radiotherapy of endometrial carcinoma stage I and II. Radiother Oncol. 1999;53:37-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Khan AM, Birk JW, Anderson JC, Georgsson M, Park TL, Smith CJ, Comer GM. A prospective randomized placebo-controlled double-blinded pilot study of misoprostol rectal suppositories in the prevention of acute and chronic radiation proctitis symptoms in prostate cancer patients. Am J Gastroenterol. 2000;95:1961-1966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Salminen E, Elomaa I, Minkkinen J, Vapaatalo H, Salminen S. Preservation of intestinal integrity during radiotherapy using live Lactobacillus acidophilus cultures. Clin Radiol. 1988;39:435-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 116] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Hauer-Jensen M, Wang J, Denham JW. Bowel injury: current and evolving management strategies. Semin Radiat Oncol. 2003;13:357-371. [PubMed] |
| 19. | Wang J, Boerma M, Fu Q, Hauer-Jensen M. Radiation responses in skin and connective tissues: effect on wound healing and surgical outcome. Hernia. 2006;10:502-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 75] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
S- Editor Liu Y L- Editor Kremer M E- Editor Lu W