Published online Jul 7, 2007. doi: 10.3748/wjg.v13.i25.3523
Revised: March 18, 2007
Accepted: April 11, 2007
Published online: July 7, 2007
Clinical severity of scrub typhus ranges from mild to fatal. Acute pancreatitis with abscess formation is a rare complication among patients with scrub typhus. This paper reports a case of scrub typhus in a 75 years old man with acute pancreatitis with abscess formation and multiorgan failure. Abdominal computed tomography showed multiple infected pancreatic pseudocysts with peri-pancreatic infiltration. Multiorgan failure was successfully treated with doxycycline, ceftriaxone, and supportive management. The pancreatic abscess was successfully drained percutaneously and the sizes of pseudocysts decreased remarkably.
- Citation: Yi SY, Tae JH. Pancreatic abscess following scrub typhus associated with multiorgan failure. World J Gastroenterol 2007; 13(25): 3523-3525
- URL: https://www.wjgnet.com/1007-9327/full/v13/i25/3523.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i25.3523
Scrub typhus is a widespread Asian zoonotic disease that is caused by infection with Orientia tsutsugamrushi (Rickettsial disease) transmitted by the bite of larval trombiculid mites (chiggers)[1]. It starts to grow at the location of the bite and a characteristic skin lesion known as an 'eschar' is formed. The rickettsia then spreads systemically via the hematogenous and lymphogenous routes. The infected patient develops various systemic symptoms and reaction including fever, exanthomatous rash, myalgia, and diffuse lymphadenopathy[2]. Clinical severity of the scrub typhus ranges from inappreciable, mild, to severe or fatal. Reported severe complications of scrub typhus include pneumonitis, acute renal failure (ARF), acute respiratory distress syndrome (ARDS), myocarditis, and septic shock[3-5]. Acute pancreatitis is, however, very rarely developed in the scrub typhus[6]. And pancreatic abscess formation as a complication of the acute pancreatitis has not been previously reported.
We reported a case of scrub typhus with unusual and serious multiorgan involvement, including ARF, interstitial pneumonitis with ARDS and acute pancreatitis with pancreatic abscess formation.
A 75-year-old man who is a farmer in the rural area was admitted because of high fever, myalgia, dyspnea and rash in the chest wall and lower extremities. On the admission, he was in acute distress with body temperature of 39°C, pulse rate of 117 beats/min, respiratory rate of 38/min and blood pressure 90/60 mmHg. Diffuse erythematous rashes over the anterior chest, lower extremities, and eschar over the left axilla were observed. The sclera was icteric and the abdomen was ovoid in shape. Bowel sound was hypoactive and the liver and the spleen were not palpable. The leukocyte count was 11900/mm3, with 92.6% neutrophil and 9% lymphocyte. The level of hemoglobin, hematocrit, platelet and CRP were 14.2 g/dL, 38.2%, 36000/mm3, and 15.0 mg/dL (normally 0-0.4 mg/dL), respectively. Prothrombin and partial thromboplastin time were prolonged to 17.3 s (42.8%) and 44.4 s, respectively. Fibrinogen was 144 mg/dL (normally 196-391 mg/dL), FDP over 20 μg/mL (normally less than 5 μg/mL), D-Dimer 677 μg/mL (normally less than 246 μg/mL). Serum liver, renal and pancreatic profiles were as follow: total bilirubin 9.4 mg/dL (normally 0.2-1.3 mg/dL); alkaline phosphatase 614 U/L (normally less than 250 U/L); aspartate aminotransferase 619 U/L (normally less than 40 U/L); alanine aminotransferase 163 U/L (normally less than 40 U/L); albumin 2.4 g/dL (normally 3.5-5.1 g/dL); amylase 241 U/L (normally 28-160 U/L); lipase 145 U/L (normally 0-60 U/L); BUN 59 mg/dL (normally 5-23 mg/dL); creatinine 1.7 mg/dL (normally 0.5-1.4 mg/dL). Serologic test for Orienta tsutsugamushi turned out positive on the second day (Ig M titer, 1:2048).
Chest radiography showed a massive alveolar infiltrate and effusion in the both lung fields (Figure 1). Abdominal computed tomogram (CT) showed mild edematous pancreas with peri-panceratic infiltration, thickened wall of gallbladder and peri-renal fluid collection.
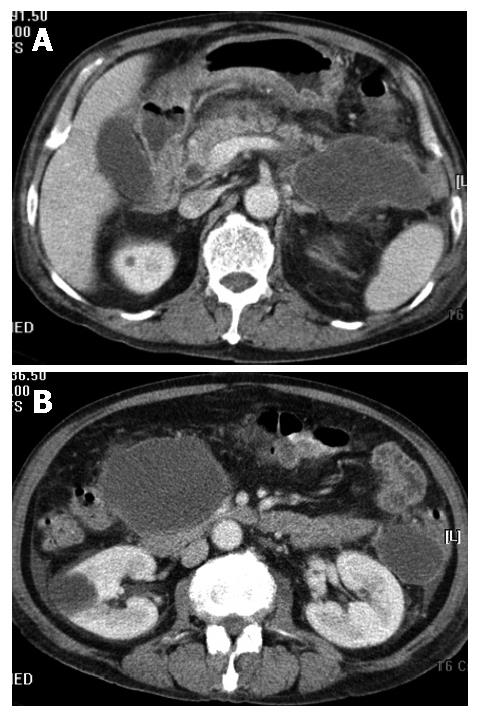
Based on the confirmation of scrub typhus with ARF, ARDS, and pancreatitis, doxycycline and ceftriaxone were daily administerd intravenously in the amount of 200 mg/d and 2 g/d, respectively. The patients' lung and kidney conditions improved markedly four weeks later, but severe abdominal pain and high fever reappeared. And the levels of amylase and lipase were elevated more than previous levels, to amylase 598 U/L and lipase 696 U/L, respectively. Follow up abdominal CT showed newly-developed large and multiple pancreatic pseudocysts on the head and the tail (Figure 2A and B). It was suspected that pancreatic abscess formed due to secondary infection. Percutaneous pancreatic abscess drainage was carried out. On the fifth day, after the drain, the abdominal pain and fever disappeared, and the general condition was also improved. The patient recovered completely and the serum level of amylase decreased to normal level. He was discharged on the 57th d. On the 14th d after the discharge, follow-up abdominal CT scan showed markedly decreased size of the pseudocysts and completely resolved pancreatic edema and peri-pancreatic infiltrations.
Scrub typhus is one of the most common infectious disease of rural south and south-eastern Asia and the western Pacific where an estimated 1 million cases occur each year, mainly among people of engaged in logging, clearing of land, and working in rice field. More than 80% of the patients accompanied with fever, rash, myalgia and generalized lymphadenitis, and 50%-80% have an inoculation eschar[7]. The cases are often mild, but if pneumonitis, menigo-encephalitis, disseminated intravascular coagulation, or renal failure is commonly observed if left untreated. Scrub typhus can be considered the most likely etiologic diagnosis. In the case presented here, the patient had symptoms such as fever, rash, myalgia and eschar, and strongly positive serologic test for rickettsial infection. He had also severe pneumonitis with ARDS, ARF, and septic shock. Pneumonia is a well-documented serious complication of the rickettsial disease, but ARDS is rare[8].
Pancreatitis has also been reported in patient with concomitant leptospirosis and scrub typhus[6]. Elevated serum pancreatic enzymes including amylase and lipase have been reported, but they were associated with renal failure. Acute pancreatitis associated with pancreatic abscess, with detectable change in the pancreatic image, reported in this case, is extremely rare in the patient with solitary scrub typhus, and has not been previously reported. The mechanism responsible of the development of the acute pancreatitis may involve and intrinsic inflammatory process via vasculitis, but the precise nature of this mechanism is not well known. The pancreatic abscess is a consequence of severe acute pancreatitis and is a circumscribed intra-abdominal collection of pus containing little or no pancreatic necrosis, usually in the proximity of the pancreas. It is likely that pancreatic abscesses are a consequence of limited necrosis, with subsequent liquefaction and secondary infection during the course of severe acute pancreatitis[9]. Overall frequency of bacterial infection of necrotic areas in the natural course of the severe acute pancreatitis is about 30% to 40%[10]. In our case, the infected pancreatic abscess was successfully drained via percutaneous approach. The patients' pain and fever disappeared and the size of cysts decreased gradually.
Fatality rate of the scrub typhus ranges from 1% to 35%, depending on the infecting strain, host factors, and treatment[11]. Although scrub typhus with mutliorgan failure is a life-threatening disease, a favorable outcome can be expected if treated with appropriate antibiotics. Use of tetracycline for populations at risk of scrub typhus has dramatically reduced the associated mortality rate and probably explains the decrease in severe complications[12].
Acute pancreatitis and pancreatic abscess with multiorgan failure is rare, but might be very important manifestation of the scrub typhus. Appropriate antibiotic treatment and interventional approach can help the patient and result in a good outcome.
| 1. | Tamura A, Ohashi N, Urakami H, Miyamura S. Classification of Rickettsia tsutsugamushi in a new genus, Orientia gen. nov., as Orientia tsutsugamushi comb. nov. Int J Syst Bacteriol. 1995;45:589-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 228] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 2. | Cracco C, Delafosse C, Baril L, Lefort Y, Morelot C, Derenne JP, Bricaire F, Similowski T. Multiple organ failure complicating probable scrub typhus. Clin Infect Dis. 2000;31:191-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Tsay RW, Chang FY. Serious complications in scrub typhus. J Microbiol Immunol Infect. 1998;31:240-244. [PubMed] |
| 4. | Chi WC, Huang JJ, Sung JM, Lan RR, Ko WC, Chen FF. Scrub typhus associated with multiorgan failure: a case report. Scand J Infect Dis. 1997;29:634-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Thap LC, Supanaranond W, Treeprasertsuk S, Kitvatanachai S, Chinprasatsak S, Phonrat B. Septic shock secondary to scrub typhus: characteristics and complications. Southeast Asian J Trop Med Public Health. 2002;33:780-786. [PubMed] |
| 6. | Wang NC, Ni YH, Peng MY, Chang FY. Acute acalculous cholecystitis and pancreatitis in a patient with concomitant leptospirosis and scrub typhus. J Microbiol Immunol Infect. 2003;36:285-287. [PubMed] |
| 7. | Ogawa M, Hagiwara T, Kishimoto T, Shiga S, Yoshida Y, Furuya Y, Kaiho I, Ito T, Nemoto H, Yamamoto N. Scrub typhus in Japan: epidemiology and clinical features of cases reported in 1998. Am J Trop Med Hyg. 2002;67:162-165. [PubMed] |
| 8. | Lee WS, Wang FD, Wang LS, Wong WW, Young D, Fung CP, Liu CY. Scrub typhus complicating acute respiratory distress syndrome: a report of two cases. Zhonghua YiXue ZaZhi (Taipei). 1995;56:205-210. [PubMed] |
| 9. | Schmid SW, Uhl W, Friess H, Malfertheiner P, Büchler MW. The role of infection in acute pancreatitis. Gut. 1999;45:311-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 144] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Beger HG, Bittner R, Block S, Büchler M. Bacterial contamination of pancreatic necrosis. A prospective clinical study. Gastroenterology. 1986;91:433-438. [PubMed] |
| 11. | Jensenius M, Fournier PE, Raoult D. Rickettsioses and the international traveler. Clin Infect Dis. 2004;39:1493-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 161] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 12. | Eaton M, Cohen MT, Shlim DR, Innes B. Ciprofloxacin treatment of typhus. JAMA. 1989;262:772-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
S- Editor Liu Y L- Editor Rippe RA E- Editor Lu W