Published online May 14, 2007. doi: 10.3748/wjg.v13.i18.2619
Revised: January 10, 2007
Accepted: January 31, 2007
Published online: May 14, 2007
AIM: To analyze the surgical management of adult primary retroperitoneal tumors (APRT) and the factors influencing the outcome after operation.
METHODS: Data of 143 cases of APRT from 1990 to 2003 in the First Affiliated Hospital of China Medical University were evaluated retrospectively.
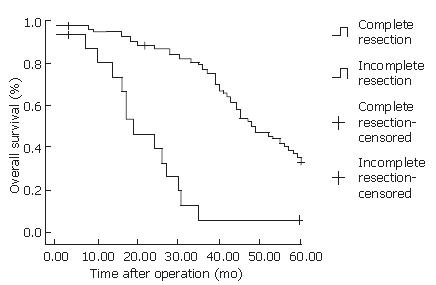
RESULTS: A total of 143 cases of APRT were treated surgically. Among them, 122 (85.3%) underwent complete resection, 16 (11.2%) incomplete resection, and 3 (3%) surgical biopsies. Twenty-nine (20.2%) underwent tumor resection plus multiple organ resections. Ninety-five malignant cases were followed up for 1 mo to 5 years. The 1-year, 3-year, and 5-year survival rates of the patients subject to complete resection was 94.9%, 76.6% and 34.3% and that of patients with incomplete resection was 80.4%, 6.7%, and 0%, respectively (P < 0.001). The Cox multi-various regression analysis showed the completeness of tumor, sex and histological type were associated closely with local recurrence.
CONCLUSION: Sufficient preoperative preparation and complete tumor resection play important roles in reducing recurrence and improving survival.
- Citation: Xu YH, Guo KJ, Guo RX, Ge CL, Tian YL, He SG. Surgical management of 143 patients with adult primary retroperitoneal tumor. World J Gastroenterol 2007; 13(18): 2619-2621
- URL: https://www.wjgnet.com/1007-9327/full/v13/i18/2619.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i18.2619
Adult primary retroperitoneal tumor (APRT) is a rare but diverse group of neoplasms that arise within the retroperitoneal space. It comprises about 0.2%-0.5% of all malignant tumors. Surgical resection is difficult because of the proximity of vital structures of the retroperitoneal and adjacent vascularities. These affect local recurrence, postoperative outcomes and long-term survival rates[1,2]. A retrospective review of 143 cases of APRT in the First Affiliated Hospital of China Medical University was performed to analyze the factors influencing postoperative outcomes and optimize treatment strategies.
From January 1990 to April 2003, 143 patients (89 males and 54 females) with APRT were treated in the First Affiliated Hospital of CMU. The mean age was 52 years (19-81 years). The clinical course range from 1 mo to 12 years, averaging 12 mo. The mean course of benign cases was 20 mo while malignant ones was 9 mo. The tumors were 6-32 cm in diameter with a mean of 13 cm. Mean diameter of benign tumors was 7 cm while it was 15 cm for malignant ones. Four patients had no symptoms when taking physical examinations, while 139 had clinical manifestations (Table 1). All patients underwent ultrasonography, computerized tomography (CT) and/or magnetic resonance imaging (MRI). A total of 122 (85.3%) patients underwent DSA. All patients with APRT received surgical therapy and pathological evaluation.
| Clinical manifestations | n (%) | |
| Abdominal mass | 84 | (60.4) |
| Abdominal pain | 72 | (51.8) |
| Abdominal distension | 26 | (18.7) |
| Lumbar region pain | 23 | (16.5) |
| Fever | 11 | (8.0) |
| Constipation | 11 | (8.0) |
| Lower extremity edema | 9 | (6.5) |
| Weight loss | 7 | (5.0) |
| Lower limb pain | 7 | (5.0) |
| Dysuria | 6 | (4.3) |
| Lower limb numbness | 5 | (3.6) |
| Loss of appetite | 5 | (3.6) |
Of the 143 patients, 122 underwent complete resection (85.5%), 43 (95.6%) of 45 benign cases and 79 (80.6%) of 98 malignant cases underwent complete resection. Sixteen (11.3%) of 143 underwent incomplete resection. Three (3%) of 143 had surgical biopsies. Twenty-nine (20.2%) patients underwent tumor resection plus multiple organ resections (Table 2). During operations, the mean amount of blood transfusion was 1150 mL, 800 mL for benign cases and 1356 mL for malignant ones. All had postoperative pathological diagnosis.
| Surgery | n |
| Nephrectomy | 16 |
| Partial colorectomy | 15 |
| Splenectomy | 11 |
| Distal Panctratectomy | 8 |
| Artificial blood vessel transplantation | 7 |
| Partial small intestine resection | 6 |
| Partial ureterectomy | 6 |
| Partial duodenectomy | 4 |
| Partial gastrectomy | 4 |
| Uterectomy | 3 |
The comparison of survival rate between complete and incomplete resection groups was performed by χ2 test. COX regression analysis was performed using an independent variable (male, malignant tumor, completeness of tumor resection, histological types) and dependent variable (recurrence, survival rate). Statistical software SPSS 13.0 version was used.
The tumor histological types of 143 patients are summarized in Table 3.
| Tissue source | Benign | n | Malignant | n |
| Mesenchymal | Lipoma | 5 | Liposarcoma | 21 |
| tissue | Leiomyoma | 4 | Leiomyosarcoma | 16 |
| Lymphangioma | 3 | Rhabdomyosarcoma | 11 | |
| Fibroma | 4 | Malignant fibrous histiocytoma | 8 | |
| Hemangioma | 5 | Malignant mesenchymoma | 6 | |
| Mesenchymoma | 4 | Malignant lymphoma | 5 | |
| Malignant hemangioendothelioma | 6 | |||
| Scirrhous fibroma | 2 | |||
| Neurogenous | Neurofibroma | 5 | Malignant neurofibroma | 9 |
| tissue | Paraganglioma | 2 | Malignant Paraganglioma | 3 |
| Schwannnoma | 4 | Malignant schwannoma | 4 | |
| Geitoembryotissue | Teratoma | 5 | Malignant teratoma | 6 |
| Unclassified tumor | Retroperitoneal cyst | 4 | Undifferentiated sarcoma | 1 |
| Total | 45 | 98 |
Ninety-five malignant patients were followed up, including 79 complete resection cases and 16 incomplete resection cases. The cut-off time was 5 years. Four patients were lost to follow-up. By the method of Kaplan-Meier survival analysis for statistical significance, the means and medians for survival time in the complete resection group was 49 mo, and that in the incomplete resection group was 19 mo. The 1-year, 3-year and 5-year survival rates was 94.9%, 76.6% and 34.3% in the complete resection group and 80.4%, 6.7%, and 0% in the incomplete resection group (Figure 1, P < 0.001). Local recurrence occurred in 28 malignant patients. Among them, 26 were subjected to re-operation or multiple surgical resection. COX regression analysis showed that completeness of tumor resection, sex and histological types were associated closely with local recurrence. Liposarcoma, leiomyosarcoma and malignant hemangioendothelioma were the 3 main histological types that tended to recur (Table 4).
| B | SE | P | RR | RR95%CI | |
| Male | 0.346 | 0.176 | 0.049 | 1.413 | 1.001-1.996 |
| Malignant tumor | 2.865 | 0.841 | 0.000 | 17.549 | 3.376-91.228 |
| Completeness of tumor resection | -0.493 | 0.182 | 0.007 | 0.611 | 0.427-0.873 |
| Leiomyosarcoma | 0.849 | 0.333 | 0.011 | 2.338 | 1.217-4.493 |
| Liposarcoma | 0.806 | 0.287 | 0.005 | 2.239 | 1.276-3.929 |
| Malignant hemangioendothelioma | 0.817 | 0.446 | 0.067 | 2.264 | 0.944-5.426 |
Surgical strategy remains the mainstay for the treatment of ARPT, because of the lack of effective adjuvant therapies[3]. The source of APRT is different and usually deep. The symptoms are not typical. It always has a long time of growth before discovery. All of these factors contribute to great difficulties for treatment.
Sufficient preoperative preparation is the key to successful operations. Preoperative ultrasonography, CT, MRI and DSA can clearly demonstrate the localization of tumors and the close proximity of organs and adjacent vascularities. These would be helpful in making precise surgical plans. Meanwhile, renal function should be examined and the preparation of intestinal canal should be done in case of combined resection. Sufficient blood should be prepared according to the size and localization of the tumor, and also prepared for vessel resection and reconstruction[4]. In our report, all patients underwent ultrasonography, CT and/or MRI. One-hundred and twenty-two (85.3%) underwent DSA, which can clearly show the location, size, appearance of the tumor and invasion tissues and organs, especially its association with main blood vessel[4]. All these examinations mentioned above provided more accurate information for further surgical procedures. In our report, 29 patients (20.2%) underwent multiple organ resections and 7 underwent vessel reconstruction. One-hundred and twenty-two patients (85.3%) were subjected to complete tumor resection. Previous reports showed the most important reason for incomplete resection was vascular invasion. In our experience, if the inferior vena cava was obstructed or had collateral circulation, reconstruction was not necessary after resection, otherwise the reconstruction needed to be performed. As a result, sufficient preoperative preparation, positive multiple organ resections, vessel reconstruction all contributed to a higher complete resection rate.
The retroperitoneal space is deep with sufficient blood circulation, and the tumors are complicated. Thus, the operative field should be completely exposed, easy to anatomize and easy to perform hemostasis. Large surgical incision, sufficient exposure and favorable surgical visual field are important for successful operation, reduction of complications and higher safety. The pseudomembrane of the tumor should be identified before the anatomy of the tumor. Separating along the pseudomembrane provides less bleeding and prevents accidental injury. Operation of the tumor should be performed gradually, which means easier parts should be dealt with first. Surgeons should control proximal blood flow before separating the tumor, and they should have the techniques to handle injured vessels and to reconstruct after vascular resection.
Complete resection of retroperitoneal tumors refers to the complete resection of a tumor which can be seen by the naked eye, including the pseudomembrane of the tumor. This does not include the incisal margin or tumor residue of the tumor bed under microscopy[5,6]. This is the best condition for surgical therapy of a retroperitoneal tumor. If necessary, resection of the whole mass of the retroperitoneal tumor can be performed. This includes the resection of the tumor and the organ tissue that can not be separated because of tumor invasion. This can assure complete resection of the tumor with a sufficient amount of normal tissue.
Incomplete resection of PRT is proper for those patients who have widespread metastasis in the abdominal cavity or whose tumors can not be completely excised even with great efforts because of invasion to vessels and/or multiple organs. The purpose of this operation is to reduce the tumor burden and relieve pressing symptoms. Complete resection was not available in some cases in this group. Five cases were because of vascular invasion, 6 cases due to metastasis in the abdominal cavity and 5 cases because of adjacent organ invasion.
It was reported that local recurrence varies from 40% to 82% and the median recurrence time ranges from 15 to 44 mo[7,8]. The recurrent rate of tumors is high for malignant tumors. Until now, operations are still the best treatment. Re-operations are needed when constitution is good and resection is effective. Among the 95 cases followed up, 28 cases (29.47%) had local recurrence, 26 cases of which underwent re-operation. In these cases, the results showed longer survival time and improved quality of life. We suggest that post-operative ARPT patients should have a physical examination every 3 mo. CT and MRI should be done as soon as abdominal mass, abdominal pain and other symptoms are found. To those without symptoms, follow-up by CT scans or MRI at 6-mo intervals can be valuable for early diagnosis to improve survival.
Postoperative follow-up ranged from 1 mo to 5 years. The 1-year, 3-year and 5-year survival rates were obviously higher than those in incomplete resection patients. COX multi-various regression analysis revealed that completeness of tumor resection, sex and histologic types were associated with local recurrence. This is similar with other reports[9]. In summary, the steps to improve therapeutic effectiveness include: (1) Complete resection; (2) early finding, early diagnosis, and early surgical intervention.
| 1. | Chiappa A, Zbar AP, Bertani E, Biffi R, Luca F, Crotti C, Testori A, Lazzaro G, De Pas T, Pace U. Primary and recurrent retroperitoneal soft tissue sarcoma: prognostic factors affecting survival. J Surg Oncol. 2006;93:456-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Wendtner CM, Abdel-Rahman S, Krych M, Baumert J, Lindner LH, Baur A, Hiddemann W, Issels RD. Response to neoadjuvant chemotherapy combined with regional hyperthermia predicts long-term survival for adult patients with retroperitoneal and visceral high-risk soft tissue sarcomas. J Clin Oncol. 2002;20:3156-3164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Scibè R, Massa M, Verdolini R, Marmorale C, Landi E. Retroperitoneal tumors. Ann Ital Chir. 1999;70:731-736; discussion 736-738. [PubMed] |
| 4. | Schwarzbach MH, Hormann Y, Hinz U, Leowardi C, Böckler D, Mechtersheimer G, Friess H, Büchler MW, Allenberg JR. Clinical results of surgery for retroperitoneal sarcoma with major blood vessel involvement. J Vasc Surg. 2006;44:46-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 122] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Stojadinovic A, Yeh A, Brennan MF. Completely resected recurrent soft tissue sarcoma: primary anatomic site governs outcomes. J Am Coll Surg. 2002;194:436-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Neuhaus SJ, Barry P, Clark MA, Hayes AJ, Fisher C, Thomas JM. Surgical management of primary and recurrent retroperitoneal liposarcoma. Br J Surg. 2005;92:246-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 125] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Heslin MJ, Lewis JJ, Nadler E, Newman E, Woodruff JM, Casper ES, Leung D, Brennan MF. Prognostic factors associated with long-term survival for retroperitoneal sarcoma: implications for management. J Clin Oncol. 1997;15:2832-2839. [PubMed] |
| 8. | Bautista N, Su W, O'Connell TX. Retroperitoneal soft-tissue sarcomas: prognosis and treatment of primary and recurrent disease. Am Surg. 2000;66:832-836. [PubMed] |
| 9. | Ouyang XH, Kong GC. Clinical study of primary retroperitoneal tumor in 66 cases. Zhongguo Putong Waike Zazhi. 1996;5:327-328. |
S- Editor Wang J L- Editor Ma JY E- Editor Wang HF