Published online May 14, 2007. doi: 10.3748/wjg.v13.i18.2541
Revised: March 30, 2007
Accepted: March 31, 2007
Published online: May 14, 2007
Glycogen storage diseases (GSD) are inherited metabolic disorders of glycogen metabolism. Different hormones, including insulin, glucagon, and cortisol regulate the relationship of glycolysis, gluconeogenesis and glycogen synthesis. The overall GSD incidence is estimated 1 case per 20000-43000 live births. There are over 12 types and they are classified based on the enzyme deficiency and the affected tissue. Disorders of glycogen degradation may affect primarily the liver, the muscle, or both. Type Ia involves the liver, kidney and intestine (and Ib also leukocytes), and the clinical manifestations are hepatomegaly, failure to thrive, hypoglycemia, hyperlactatemia, hyperuricemia and hyperlipidemia. Type IIIa involves both the liver and muscle, and IIIb solely the liver. The liver symptoms generally improve with age. Type IV usually presents in the first year of life, with hepatomegaly and growth retardation. The disease in general is progressive to cirrhosis. Type VI and IX are a heterogeneous group of diseases caused by a deficiency of the liver phosphorylase and phosphorylase kinase system. There is no hyperuricemia or hyperlactatemia. Type XI is characterized by hepatic glycogenosis and renal Fanconi syndrome. Type II is a prototype of inborn lysosomal storage diseases and involves many organs but primarily the muscle. Types V and VII involve only the muscle.
- Citation: Özen H. Glycogen storage diseases: New perspectives. World J Gastroenterol 2007; 13(18): 2541-2553
- URL: https://www.wjgnet.com/1007-9327/full/v13/i18/2541.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i18.2541
Glycogen storage diseases (GSD) are inherited metabolic disorders of glycogen metabolism (Figure 1)[1,2]. In postprandial period, blood glucose level increases and endogenous glucose production is suppressed. Exogenous glucose is either metabolized to pyruvate or stored as glycogen in the liver and skeletal muscle[1]. Under aerobic conditions, pyruvate is converted to acetyl coenzyme A (acetyl-CoA), which enters the citric acid cycle, the products of which are water, carbon dioxide and adenosine triphosphate (ATP) or used for the synthesis of fatty acids. In contrast, under anaerobic conditions, pyruvate is converted to lactate, which is an important alternative fuel during episodes of hypoglycemia. Different hormones, including insulin, glucagon, cortisol and others regulate the relationship of glycolysis, gluconeogenesis and glycogen synthesis[1].
Although it is hard to estimate accurately, based on several studies, the overall GSD incidence is approximately 1 case per 20000-43000 live births and the most common one is type IX[3,4]. They are classified based on the enzyme deficiency and the affected tissue. Disorders of glycogen degradation may affect primarily the liver, the muscle, or both. In this review, GSD affecting the liver are discussed mainly and the others briefly. Episodes of hypoglycemia and enlargement of the liver are the main findings in all hepatic GSD, but apart from this the heterogeneity of their presentation is considerable. Eighty percent of hepatic GSD is formed by types I, III, and IX[2].
Glycogen storage disease type 0 (GSD-0; Glycogen synthase deficiency) was first described in 1963 as glycogen synthethase deficiency in the liver[5]. Because there is a marked decrease in liver glycogen content, in fact, GSD-0 is not a true GSD. Its gene locus is at 12p12.2 and inherited as autosomal recessive[6].
There are wide phenotypical variations. The symptoms are due to hypoglycemia and include lethargy, pallor, nausea, vomiting, and sometimes seizures in the morning before breakfast. Although developmental delay may develop in some children, most children are cognitively and developmentally normal. Some patients may survive without symptoms or with very mild symptoms[7]. The liver is not enlarged in GSD-0. Short stature and osteopenia are common features, but other long-term complications, common in other types of GSD, have not been reported in GSD-0[8]. Rarely, GSD-0 may present with hyperglycemia and glucosuria which may cause diagnostic problems[9].
Symptoms rapidly relieve by serving frequent protein-rich meals and nighttime feedings of uncooked cornstarch (UCCS) (a slow release glucose preparation). Gluconeogenesis and fatty acid oxidation are intact and this explains a milder course of the disease than the other hepatic glycogenoses. With more prolonged fasting, however, severe hyperketonemia and high free fatty acid level inhibit release of alanine from skeletal muscle leading to decreased gluconeogenic precursors and worsening hypoglycemia[8].
Elevation of blood lactate and lipid after administration of glucose or galactose is a useful diagnostic test[1,9]. Demonstration of decreased hepatic glycogen on a liver biopsy for the definitive diagnosis of GSD-0 has been replaced by mutation analysis of the gene, which is a non-invasive method for making diagnosis[6].
The deficiency of the glucose-6 phosphatase (G6Pase) activity causes glycogen storage disease type I(GSD-I; Von Gierke disease; Glucose-6-phosphatase deficiency; Hepatorenal glycogenosis). Both glycogenolysis and gluconeogenesis are affected. G6Pase, the most important role of which is to provide glucose during starvation, is found mainly in the liver and the kidneys. It is associated with the endoplasmic reticulum (ER) and functions as a multicomponent system[10]. There are 4 subtypes depending on the abnormality in G6Pase system. The catalytic subunit of the system is located inside the ER and its defect causes type Ia (GSD-Ia). Additionally, there are transporters for the entry of substrate glucose-6-phosphate (G6P) into the ER and for the exit of the products, phosphate and glucose. The defect in the transporter of G6P (G6PT) causes type Ib (GSD-Ib). The presence of further subtypes (1c and 1d) has also been postulated.
The disease has an autosomal recessive transmission. Its incidence is 1/100000 to 1/400000 births in the general Caucasian population, with types 1b and 1c being much less frequent than type 1a, whereas its prevalence is 1 in 20000 Ashkenazi Jews population[11]. Both the enzyme and G6PT are already known at the molecular level.
GSD type Ia
Demonstration of the deficiency of G6Pase in GSD-Iin 1952 by Cori and Cori is the first specific enzymopathy identified in a hereditary disorder[12]. In 1993, the gene encoding the catalytic unit of the G6Pase complex was identified to be located on chromosome 17[13]. Later on its molecular and biochemical characteristics and the expressed protein were reported[13-15].
Initial symptoms are due to hypoglycemia and occur shortly after birth, and episodes do not respond to glucagon administration. Main symptoms are tremors, irritability, hyperventilation, cyanosis, apnea, convulsions, paleness, sweating, cerebral edema/dysfunction, coma and death, particularly in the morning or before feedings. Older infants may present with a doll-like facial appearance, frequent lethargy, difficult arousal from sleep, tremors, overwhelming hunger, growth retardation, protuberant abdomen, relatively thin extremities. There is a tendency to nose bleeding due to impaired platelet function, particularly in those with insufficient metabolic control. During infectious diseases symptoms of severe hypoglycemia are more frequent due to decreased appetite. In middle childhood, affected patients may manifest evidence of rickets and anemia[2,16,17]. Patients with GSD Ia as well as patients with GSD Ib may suffer from intermittent diarrhea, which seems to worsen with age. The cause of this diarrhea is unknown[18].
On physical examination the liver may be enlarged at birth or it becomes enlarged in a very short time[2]. There is abdominal protuberance because of massive hepatomegaly. With ageing, the patient may present with poor growth, short stature, and rachitic changes[2]. Rarely, xanthoma may be found on extensor surfaces, such as the elbows and knees.
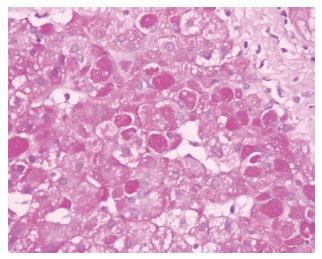
Most striking laboratory abnormalities, in addition to hypoglycemia, are lactic acidosis, hyperlipidemia (particularly hypertriglyceridemia), and hyperuricemia[2,16]. Transaminase levels usually increase slightly[2]. Kidneys may be enlarged on ultrasonographic examination in affected patients of all ages. Although there is controversial report[19], serum biotinidase activity increased in GSD-Ia patients[20,21]. There may be hypercalciuria[2]. Histopathological findings of the liver include mosaic pattern with pale-staining, swollen hepatocytes, steatosis, and nuclear hyperglycogenation (Figure 2). Although it is not as prominent as that of GSD type III, IV and VI, fibrosis is also present in some patients[2,22]. And although triglyceride and cholesterol levels decreased in the majority of the patients, they did not normalize[2].
In children, growth retardation is a remarkable finding in the majority of the patients[2,23] and short stature is common among adult patients[24]. In addition, without effective treatment, long-term complications occur, namely hepatic adenomas, renal dysfunction and urolithiasis, osteoporosis, and gout. Hyperlipidemia may cause xanthomas, pancreatitis, and cholelithiasis[17].
With ageing the prevalence of renal involvement increases[25]. The first manifestation of renal involvement is glomerular hyperfiltration, the mechanism of which is still obscure. Renal disorder may progress to microalbuminuria, proteinuria, hypertension and end-stage renal disease. Hypercalciuria and hypocitraturia cause nephrocalcinosis and/or urolithiasis[26]. Hypertension and hematuria are the other findings[27,28]. The earliest pathological finding is focal segmental glomerulosclerosis. Renal disease may progress to chronic renal disease in adult patients[24,28]. Gout, anemia, osteopenia and/or fractures, increased alkaline phosphatase and gamma-glutamyltransferase are common. Osteoporosis may be due to poor nutrition, the effects of lactic acidosis and hypogonadism[29].
Hepatic adenoma may develop at any age[30] and may undergo malignant transformation within a period as long as 28 years[31-34]. Alpha fetoprotein levels may be normal with malignant transformation or may be high without malignant transformation although current guidelines recommend abdominal ultrasonography with alpha fetoprotein and carcinoembryonic antigen levels every 3 mo once patients develop hepatic lesions[34]. The reported prevalence of hepatic adenoma ranges from 22% to 75% and they mostly appear during or after puberty. Hepatic adenoma and hepatocellular carcinoma (HCC) may be seen in children younger than 1 year of age[35]. Abdominal CT or magnetic resonance imaging (MRI) is advised when the lesions are large or poorly defined or are growing larger[34]. A high glucagon/insulin ratio, glycogen accumulation in cells and protooncogene/oncogene activation or mutation has been proposed as pathogenesis.
Despite increased levels of triglyceride, VLDL and LDL in GSD-Ia patients, endothelial vascular dysfunction and atherosclerosis are rare. It has been postulated that the raised apoE levels in the serum could play an important role in counterbalancing the increased atherosclerosis risk associated with the lipid profile of patients with GSD-Ia[36]. In 60% of GSD Ia patients von Willebrand factor (vWF) antigen (vWF:Ag) and intensity of individual oligomers are reduced[37]. This situation may also have a potential role in the protection from vascular complications. This result may also explain the bleeding tendency in GSD type I patients. It has also been speculated that platelet dysfunction in GSD Ia is caused by chronic hypoglycemia leading to diminished glucose uptake into platelets and eventually intracellular ATP deficiency[38]. In addition to an increase of protective antioxidative factors recently detected in this patient group[39,40], this could be due to changes in coagulation factors.
Brain damage, probably caused by recurrent severe hypoglycemia, may be present in patients with GSD-I[41]. Both results of tests of performance ability and brain-stem auditory evoked potentials abnormalities significantly correlated with the frequency of admissions for hypoglycemia, whereas EEG abnormalities correlated with dietary compliance. The MRIabnormalities were characterized by dilatation of occipital horns and/or hyperintensity of subcortical white matter in the occipital lobes in all patients. Women with GSD-Ia may have pregnancies and deliveries without any problem[42].
GSD-Ia is usually suspected on the basis of a set of clinical and biochemical features, the definitive diagnosis being confirmed by a liver biopsy and enzyme assay or, more recently, by mutation analysis. Therefore, the development of rapid and minimally invasive diagnostic methods continues to be a challenge. In GSD-Ia R83C and Q347X are the most prevalent mutations in Caucasians, 130X and R83 C in Hispanics, and R83H in Chinese[43-45]. As plasma from healthy people do not contain it, plasma α-hydroxyisobutyrate detected by 1H NMR spectroscopy may be used as a possible biomarker for the diagnosis of GSD1a[46]. Prenatal diagnosis by chorionic villus sampling is possible when the mutation in index case is known[47].
The mainstay of treatment is to prevent hypoglycemia either by continuously providing a dietary supply of glucose, or by frequent ingestion of UCCS during day and night or nocturnal intragastric feeding[48]. The use of UCCS in adult patients with GSD-I has been shown to be simple and effective for long-term treatment. UCCS administration achieves satisfactory glycemia lasting a median of 4.25 (range 2.5-6) h[49]. Good dietary management minimizes the metabolic abnormalities of the disease and decreases the risk of long-term complications[17]. By controlling hypoglycemia the severity of renal involvement may regress. Although there are studies suggesting that intestinal glucose absorption may be impaired in vitro and in vivo in subjects with GSD-Ia and GSD-Ib[50,51], in a recent study it has been shown that starch digestion and absorption are not impaired in GSD-Ia[52]. However, overall utilization of UCCS appears to be lower in GSD-Ia, which is most likely secondary to perturbed intermediary metabolism. Lactose, fructose and sucrose should be restricted except for fruits, vegetables and small amounts of milk products. Enough essential nutrients, vitamins and minerals should be given. If there is anemia, the causes must be evaluated and appropriate treatment should be started (for a comprehensive dietary therapy of GSD-I, see reference No 18).
Allopurinol (10 mg/kg per day, divided into 3 dosages) should be given if hyperuricemia is present. If acidosis is present (blood base excess < 5 mmol/L or blood bicarbonate < 20 mmol/L), bicarbonate (1-2 mmol/kg per day in 4 doses) or potassium citrate (5-10 mEq every 8-12 h) should be prescribed[17]. It has been shown that angiotensin converting enzyme inhibitors (captopril, ramipril) are useful for preventing deterioration of renal function and for decreasing albuminuria[53-55]. If serum triglyceride levels remain above 10.0 mmol/L despite optimizing dietary treatment, triglyceride-lowering drugs (nicotinic acid, fibrates) should be recommended to reduce the risk of cholelithiasis and pancreatitis. In adult patients, statins may be given if cholesterol levels are persistently elevated (> 8-10 mmol/L)[17].
Prior to elective surgery, bleeding time (platelet aggregation) should be normalized by continuous gastric drip feeding during 24 h for 1 wk or by intravenous glucose infusion over 24-48 h[17]. Close peri-operative monitoring of blood glucose and lactate concentration is essential. Low-dose diazoxide may prolong normoglycemia after meals, may reduce fasting lactic acidosis, and may help catch-up growth[56]. The mode of action of diazoxide seems to be linked to K [+]-ATP channel activation.
Despite improved survival and growth, long-term complications of GSD-I have not responded completely to dietary therapy with UCCS or continuous gastric feeding. Administration of G6Pase in a viral vector and hepatocyte transplantation are under investigation for treatment of GSD-I[57].
Liver transplantation corrects all liver related bioche-mical abnormalities but its effect on reversal and/or prevention of renal disease remains unclear[58-60]. Renal transplantation corrects only renal abnormalities[61].
GSD type Ib
In 1968, a second type of GSD-I, GSD type Ib (GSD-Ib; Glucose-6-phosphate translocase deficiency), was proposed after recognizing that in vitro G6Pase activity was normal despite that glucose was not liberated from G6P in vivo[62]. It was explained, in 1975, that there is a G6P specific transport system that transports G6P from the cytoplasm to the lumen of the endoplasmic reticulum[63]. Recently, the gene encoding G6PT has been identified on chromosome 11q23, and sequenced[64,65].
In addition to clinical symptoms and findings seen in GSD-Ia, recurrent infections, neutropenia, and neutrophil dysfunction are recognized as distinctive features of GSD-Ib. Most but not all GSD-Ib patients have neutropenia and neutrophil dysfunction that predispose to severe infections and to inflammatory bowel disease[66]. Different from G6Pase gene, G6PT gene is also expressed in hematopoietic progenitor cells, which might explain major clinical symptoms such as neutropenia and frequent infections[67]. In GSD-Ib, neutrophils are defective in both motility and respiratory burst[68]. This situation may be due to the impaired glucose transport across the cell membrane of polymorphonuclear leukocytes. It has been suggested that microsomal G6P transport has a role in the antioxidant protection of neutrophils, and that the genetic defect of the transporter leads to the impairment of cellular functions and apoptosis, which may be a potential explanation for neutrophil dysfunction in GSD-Ib[69]. There are GSD-Ib patients without neutropenia and it has been proposed that it could be due to G6PT mutations with residual transporter activity[70].
Another distinctive feature of GSD-Ib is the observation of inflammatory bowel disease (Crohn)-like colitis[71,72]. All have absolute neutrophil count less than 1000 cells/mL. Fever, diarrhea, and perioral and anal ulcers are the accompanying findings and symptoms. The severity of the primary disorder is not correlated with the intestinal symptoms.
There is no correlation between genotype and the presence of neutropenia, bacterial infections and systemic complications in GSD-Ib[73].
They may have severe infectious complications due to both neutropenia and functional defects of PMNs and monocytes. Young children with GSD-Ib may have frequent otitis, gingivitis, and boils. Like GSD Ia patients, patients with GSD Ib may suffer from intermittent diarrhea. Inflamed intestinal mucosa, documented by increased fecal α1-antitrypsin excretion and inflammation in the colonic biopsies, seems to be the main cause[66].
Although it is rare, terminal kidney disease may develop in patients with GSD-Ib and kidney transplantation may be necessary[74]. Patients with GSD-Ib have an increased prevalence of thyroid autoimmunity and hypothyroidism, although patients with GSD-Ia have little evidence of thyroid abnormalities[75]. Concomitant damage at the level of the hypothalamus or pituitary gland might be hypothesized on the basis of the slightly elevated thyrotropin levels, even in patients with overt hypothyroidism[75].
In the case of GSD-Ia, G6Pase activity is deficient in both intact and disrupted microsomes; in that of GSD-Ib, a combination of deficient G6Pase activity in intact microsomes and (sub)normal G6Pase activity in disrupted microsomes is observed[17,76]. Normoglycemia even after a 24 h-fasting period does not exclude the diagnosis of GSD-Ib in a patient with hepatomegaly[77].
The current treatment for GSD-Ib consists of a dietary therapy, including continuous nasogastric infusion of glucose[78] or frequent oral administration of UCCS[49]. Additionally, granulocyte colony-stimulating factor (G-CSF) therapy may restore myeloid functions[79,80]. The combined dietary and G-CSF therapies significantly alleviate the metabolic and myeloid abnormalities of GSD-Ib patients and greatly improve their prognosis. However, the underlying pathological process remains untreated and as a result, long-term complications, such as kidney disease in the form of renal calculi and progressive renal disease, inflammatory bowel disease, hepatic adenomas and following G-CSF therapy, splenomegaly, develop in a significant portion of adult patients. Moreover, the efficacy of dietary treatment is frequently limited due to poor compliance. The patients with GSD-Ib may require liver transplantation to prevent malignant transformation of hepatic adenomas and for refractory hypoglycemia. Although hypoglycemia improves after liver transplantation, neutropenia generally continues to be present[60,74].
After infusion of adenoviral vectors containing human G6PT into G6PT-deficient mice that manifested symptoms characteristic of the human disorder, levels of G6PT mRNA expression in the liver, bone marrow and spleen were restored, and metabolic as well as myeloid abnormalities were corrected[81]. The therapy also corrects neutropenia and lowers the elevated serum levels of granulocyte colony-stimulating factor. This effective use of gene therapy to correct metabolic imbalances and myeloid dysfunctions in GSD-Ib mice holds promise for the future of gene therapy in humans.
GSD type Ic and Id
Liver microsomal transport of phosphate and glucose is deficient in GSD-Ic and Id (GSD-Ic and GSD-Id), respectively. Molecular analyses showed that clinically and biochemically diagnosed type Ic and Id patients had mutations not different from those of the GSD-Ib patients[82,83]. The fact that the same mutations were found in GSD types Ib and Ic could indicate either that Pi and G6P are transported in microsomes by the same transporter or that the biochemical assays used to differentiate Pi transpoter defect from G6P transport defects are not reliable. It has also been shown that there is no correlation between the mutation and the severity of the disease, including the presence of neutropenia[84].
Recent data indicates that mutations in the G6Pase gene and in the G6PT gene account for most, if not all, typical cases of GSD type I and it has been stated that in practice there are only 2 subtypes of GSD-I( Ia and Ib) and the existence of other forms of GSD-I remains to be substantiated[10]. However, patients with kinetic and enzymatic pattern indicative of GSD Ic and with no mutations in both the G6Pase enzyme and the G6PT have been reported recently[85]. This raised the question of the existence of a separate locus for GSD Ic. Na/phosphate co-transporter 4, expressed in the liver and kidney, is localized to the ER membrane and is a candidate for GSD Ic[85].
Glycogen storage disease type III(GSD-III; Cori disease; Forbes disease; Amylo-1,6-glucosidase deficiency; Glycogen debrancher deficiency) results from deficient glycogen debrancher enzyme activity, which has two independent catalytic activities; oligo-1,4-1,4-glucantransferase and amylo-1,6-glucosidase. Both catalytic activities are required for normal full debranching enzyme activity[86]. Deficiency in the enzyme results in an excessive accumulation of abnormal glycogen, which is harmful for hepatocytes. The enzyme gene was isolated on 1p21, and nucleotide sequence and multiple tissue-specific isoforms have been identified[87,88].
GSD-III accounts for approximately 24% of all GSD cases, and its estimated incidence in Europe is 1 case per 83000 live births, and 1 in 100000 live births in North America[89]. The highest known GSD-III prevalence occurs in the Faroese population of the Faroe Islands, where the estimated incidence is 1:3600 due to a founder effect[90]. There is no genotype and clinical phenotype correlation. The variable phenotype of GSD-III patients is explain-ed by differences in tissue expression of the deficient enzyme[86].
There are two major GSD-III subtypes; GSD IIIa, which affects both the liver and muscle, accounts for 80% of the cases and IIIb, which affects only the liver, comprises approximately 15% of all GSD-III patients[24,91]. In rare cases, selective loss of glucosidase activity (GSD-IIIc) or transferase activity (GSD-IIId) has been demonstrated[92,93].
Hepatomegaly, hypoglycemia, short stature, dyslipide-mia, and in a few cases, slight mental retardation are seen in both subtypes. Muscle symptoms can start together with liver disorders or long after hepatic disorders or after liver symptoms disappeared in childhood. In a small group of the patients there are only muscle symptoms as adults without any sign or history of liver dysfunction after childhood[94,95]. Liver symptoms improve with age and usually disappear after puberty. Overt liver cirrhosis occurs rarely[86,95]. Muscle weakness, although minimal during childhood, may become the predominant feature in adults with type IIIa disease[96]. In these patients, slowly progressive weakness and distal muscle wasting are observed. In the majority of IIIa patients there is cardiac involvement with different severity ranging from ventricular hypertrophy on ECG to clinically evident cardiomegaly[97].
Facial abnormalities (depressed nasal bridge and a broad upturned nasal tip, indistinct philtral pillars, bow-shaped lips with a thin vermillion border, and deep-set eyes in younger patients) may be present in the patients[98]. Children may complain of persistent otitis media or recurrent sinusitis.
During infancy serum AST, ALT, LDH, and ALP levels are markedly elevated. Their levels decrease around puberty concomitantly with a decrease in liver size. Creatine kinase level is increased in patients with muscle involvement and can be used to determine muscle involvement[96]. However, a normal level does not rule out the presence of muscle enzyme deficiency[99,100].
Some GSD-III patients may be at an increased risk of osteoporosis[29], which, in part, may be due to poor nutrition, the effects of lactic acidosis and hypogonadism. Although hepatic involvement is considered mild, with increased survival, a few cases of liver cirrhosis and HCC have been reported[101]. There are no reliable biomarkers to monitor for HCC in GSD-III. Development of guidelines to allow for systematic review and microarray studies are needed to better delineate the etiology of the HCC in patients with GSD-III.
There are usually periportal fibrosis, and sometimes progress to micronodular cirrhosis. Liver histology shows distension of hepatocytes by glycogen accumulation, and presence of periportal septal fibrosis, early in the disease process, perhaps related to the accumulation of abnormally short-branched glycogen[95].
The diagnosis of GSD-III is made by demonstrating enzyme deficiency in the liver or muscle. Where it is possible, mutation analysis serves a non-invasive and easy method for diagnosis[96]. Deficient enzyme activity can be demonstrated in these patients not only in the liver and muscle but also in other tissues, such as the heart, erythrocytes, and cultured fibroblasts.
Treatment for GSD-III is primarily dietary and is aimed at maintaining normoglycemia. This is achieved by frequent meals high in carbohydrates and cornstarch supplements alone or with gastric tube feedings. For patients with myopathy, in addition to management of hypoglycemia, a high protein diet is recommended[60,101]. Liver transplantation corrects all liver related biochemical abnormalities but the long-term success with regard to myopathy/cardiomyopathy is not known[60].
Glycogen storage disease type IV (GSD-IV; Andersen disease; Brancher deficiency; Amylopectinosis; Glycogen branching enzyme deficiency) was first described by Andersen[102] in 1956 as "familial cirrhosis of the liver with storage of abnormal glycogen" and, in 1966, a deficiency of amylo-1, 4 to 1, 6-transglucosidase (glycogen branching enzyme) was reported[103]. Without glycogen branching enzyme, the glycogen cannot be branched and abnormal glycogens resembling an amylopectin-like structure (polyglucosan), which is harmful for cells, accumulate in various tissues including hepatocytes and myocytes[104,105]. The gene of the enzyme was mapped to chromosome 3p12 in 1993[105]. Mutation in the same gene causes adult polyglucosan body disease. It represents 0.3% of all glycogen storage diseases, and is transmitted as an autosomal recessive trait[106].
GSD-IV is clinically extremely heterogeneous, owing in part to variation in tissue involvement[104,106]. The existence of tissue specific isozymes may be responsible for remarkable phenotypic variability of the disease. In the classical hepatic form, the patient appears normal at birth. But the disease rapidly progresses, early in life, to cirrhosis, and causes death due to liver failure between 3 and 5 years of age[102]. Affected children present with failure to thrive, hepatosplenomegaly and cirrhosis in the first 18 mo of age. Rarely, the hepatic disease is non-progressive or slowly progressive[107]. In non-progressive hepatic form patients may present with hepatosplenomegaly and a mild elevation of serum transaminases. Generally patients do not show any further progression of disease and growth is normal and liver enzymes may return to normal[107].
In multiple system involvement, the deficiency of the enzyme was detected in both muscle and the liver[108]. This includes peripheral myopathy with or without cardiomyopathy, neuropathy, and liver cirrhosis. The age of onset ranges from neonatal to adult age[109]. The neuromuscular presentation is divided into 4 groups according to age at onset[110]. In perinatal (fetal) form, which may cause hydrops fetalis and polyhydroamnios, the affected baby shows arthrogryposis of the limbs due to akinesia[111]. The presence of cervical cystic hygroma during pregnancy may be a warning sign of the disease[106]. Prenatal diagnosis is possible by determining enzyme activity or chorionic villi sampling. Death is inevitable in the neonatal period. Liver cirrhosis and hepatic failure have not been described. In congenital form, the patients have severe hypotonia, hyporeflexia, cardiomyopathy, depressed respiration and neuronal involvement[104,112-114]. Liver involvement is not severe and the child dies in early infancy. Childhood neuromuscular form presents with myopathy or cardiopathy starting at any age[110,115]. The main presenting symptoms are exercise intolerance, exertional dyspnea and congestive heart failure in progressed cases. The disorder may be limited to muscle tissue and serum creatine kinase may be normal. In adult form, there is isolated myopathy or polyglucosan body disease. The symptoms begin at any age in adulthood and may resemble muscular dystrophies; progressive difficulty in walking, and proximal limb weakness which was greater in the arms than the legs. Upper and lower motor neurons are involved. The disease may present as pyramidal tetraparesis, peripheral neuropathy, early neurogenic bladder, extrapyramidal symptoms and seizures, and cognitive impairment terminating in dementia[111]. The diagnosis can be made by studying enzyme activity in erythrocytes[116,117]. Ultrastructural examination of the central nervous system and skeletal muscle reveals amylopectin-like inclusions both in neurons and muscular fibers. MRIshows white matter abnormalities[118].
Histological examination of the liver shows hepatocellular periodic-acid Schiff positive, diastase-resistant inclusions of the abnormal glycogen deposits (Figure 3). The enzyme deficiency can usually be demonstrated in the liver, leukocytes, erythrocytes and fibroblasts although normal leukocyte enzyme activity may be detected in patients with cardioskeletal myopathy[104]. Microscopic examination of tissues, demonstration of enzyme deficiency and mutation analysis confirm the diagnosis of GSD-IV[104,112].
The only effective therapeutic approach presently available for GSD-IV patients with progressive liver disease is liver transplantation. Liver transplantation may be helpful not only for liver disease but also for muscular involvement[60,119,120]. This may be due to systemic microchimerism after liver allotransplantation and amelioration of pancellular enzyme deficiencies.
Glycogen storage disease type VI(GSD-VI; Hers disease; Liver glycogen phosphorylase deficiency) is a rare form of GSD. Enzyme deficiency is only in the liver. The gene encoding liver phosphorylase was mapped to chromosome 14q21-q22 in 1987[121].
Phosphorylase deficiency in the liver manifests in infants, primarily with hepatomegaly and growth retardation. It typically takes a benign course, with remission of symptoms as the children grow up[122]. The clinical picture changes from mild to moderate hypoglycemia. Despite gross hepatomegaly patient is largely asymptomatic without hypoglycemia. Some mutations permit residual enzyme activity and the disease is less severe in the patients with these mutations[123]. There are generally mild ketosis, growth retardation, prominent hepatomegaly and elevated levels of serum transaminases, triglycerides and cholesterol[124], although biochemical investigations are normal in patients with high residual enzyme activity[123].
In some patients, high in vitro residual enzyme activities may be unfavorable for the establishment of a definitive diagnosis by an enzymology alone and mutation analysis of the genes encoding for the responsible enzymes may help in these situations[123,124].
Phosphorylase kinase (PhK) activates glycogen phos-phorylases in muscle, the liver, and other tissues. The numbering of PhK deficiency (Phosphorylase kinase system defects; GSD VIa, IX, X, or VIII) is confusing, ranging from type VIa to VIII to IX. PhK consists of 4 different subunits (α, β, γ, δ), each encoded by different genes on different chromosomes and differentially expressed in various tissues[125]. α and β subunits have regulatory functions, γ subunit has catalytic function, and δ Ca2+ binding function. The α subunit has two isoforms, a muscle isoform and a liver isoform, which are encoded by two different genes on X chromosome[125]. The genes for other subunits are located on autosomal chromosomes. The types involving the liver are mainly classified into 2 forms; the X-linked liver form (there are 2 subtypes; XLG-Iand XLG-II) and autosomal recessive form. The four main clinical variants, in order of decreasing incidence, affect the liver, liver and muscle, muscle only, and heart only[126,127].
X-linked liver phosphorylase kinase deficiency
X-linked liver phosphorylase kinase deficiency (XLG; X-linked liver glycogenosis type I and type II, formerly GSD-VIII or GSD-VIa) is one of the mildest of GSD and is similar to GSD-VI in that both have low phosphorylase activity in the absence of adenosine monophosphate. The cause of approximately 25% of all cases of GSD can be ascribed to a deficiency of PhK, among which XLG is the most common type[128]. There are 2 enzyme loci on the X chromosome: one for the alpha subunit of muscle PhK, and one for the alpha subunit of liver PhK. The gene of liver PhK was mapped to Xp22.2-p22.1 in 1992[125].
The common symptoms and findings are hepatomegaly, growth retardation, delay in motor development, hypotonia, elevation of ALT, AST, cholesterol and triglyceride, and fasting hyperketosis and hypoglycemia[129-132]. Splenomegaly, liver cirrhosis, doll facies, osteoporosis, neurologic disease, elevated serum lactate, metabolic acidosis and renal tubular acidosis have been described very rarely. The clinical course is benign and most adult patients are asymptomatic[130]. With ageing, clinical and biochemical abnormalities gradually disappear.
There are 2 types of the disease; classic type (type I) and the variant type (type II)[133]. Type IIis characterized by enlarged liver and growth retardation and does not show enzymatic deficiency of phosphorylase kinase in blood cells different from type I[128].
The disorder is caused by mutations in the gene, localized on 16q12-q13, encoding the beta subunit of phosphorylase kinase[134]. The disease is characterized by a distended abdomen due to marked hepatomegaly, marked accumulation of glycogens in both the liver and muscles, and hypoglycemic symptoms after several hours of fasting or physical activity[134,135]. The symptoms are generally mild or absent, affecting virtually only the liver. Growth is also mildly impaired.
There are two isoforms, encoded by separate genes, for the gamma subunits; the muscle form and the testis/liver form. It has been reported that autosomal liver-specific PhK deficiency is associated with mutations in the gene encoding the testis/liver isoform of the catalytic gamma subunit[136]. The gene for liver form has been mapped to 16p12.1-p11.2. Mutations in this gene are particularly associated with an increased risk of cirrhosis[137].
The primary defect is defective transport of monosaccharide across the membranes. Utilization of glucose and galactose is impaired[138]. Glycogen storage disease type XI(GSD-XI; Fanconi-Bickel Syndrome, FBS) is rare and characterized by hepatorenal glycogen accumulation and proximal renal tubular dysfunction[139,140]. It is inherited in an autosomal recessive mode and the responsible gene, glucose transport 2 gene (GLUT2), was localized to 3q26.1-q26.3 in 1988[141,142].
Patients usually first present at an age of 3 to 10 mo. The desease is characterized by hepatorenal glycogen accumulation, fasting hypoglycemia as well as postprandial hyperglycemia and hypergalactosemia, proximal renal tubular dysfunction, rickets and marked stunted growth retardation. The most striking finding is dwarfism in older patients. Puber-ty is severely retarded. Protuberant abdomen due to hepatomegaly, moon-shaped face, and fat deposition in the shoulders and abdomen are the other striking findings. Hepatomegaly may be absent in some patients[140,143]. Hypercholesterolemia and hyperlipidemia are pronounced and may cause pancreatitis. Generalized osteopenia develops early and may lead to fractures. Hypophosphatemic rickets and osteoporosis later in life are constant features. Tubular nephropathy was characterized by excessive glucosuria, and moderate hyperphosphaturia in the presence of constant hypophosphatemia, hyperuricemia, hyperaminoaciduria, and intermittent albuminuria (renal Fanconi syndrome)[138,139]. Progression to renal failure is not the case. There may be mild metabolic acidosis due to renal bicarbonate loss[138]. Cataracts, a consequence of frequently documented hypergalactosemia, are only seen in a few cases.
Laboratory findings are fasting hypoglycemia and ketonuria, hyperglycemia and hypergalactosemia in the postabsorptive state, hypercholesterolemia and hyper-lipidemia, moderately elevated ALP, hypophosphatemia, hyperaminoaciduria, glucosuria, galactosuria, and proteinuria, normal enzymes of galactose and glycogen metabolism, normal fructose metabolism, and normal endocrinologic results[138]. Liver biopsy reveals excessive glycogen accumulation with steatosis. Because of galactose intolerance, patients with FBS can be detected by neonatal screening for galactose[138,143,144].
Symptomatic treatment is directed towards a stabi-lization of glucose homeostasis and compensation for renal losses of various solutes, which include replacement of water, electrolytes, and vitamin D, restriction of galactose, and a diabetes mellitus-like diet, presented in frequent small meals with adequate caloric intake, the administration of UCCS[138,143,145]. Because fructose metabolism is not affected in FBS patients[146], it can be used as an alternate carbohydrate source in the therapy of FBS. Liver size and glycogen content reduce after antiketogenic diet[138].
Acid maltase deficiency (GSD-II, Pompe disease; Acid alpha-glucosidase deficiency; Acid maltase deficiency; Alpha-1, 4-glucosidase deficiency) is the prototypic lysosomal storage disease. The clinical presentation is heterogeneous, largely due to the varied of residual enzyme activity, which is associated with different mutations in the responsible gene, which is mapped to chromosome 17q25.2-q25.3[147].
There are 4 types of GSD-II. The combined frequency of infantile and adult GSD-II is around 1/40000 in Caucasians[148]. In the classic infantile form (Pompe disease), cardiomyopathy and muscular hypotonia are the cardinal features; in juvenile and adult forms, involvement of skeletal muscles dominates the clinical picture[149]. There is an inverse correlation between the severity of clinical manifestations and the level of residual enzyme activity in fibroblasts[150]. The mutation may, therefore, affect the production or degradation of the enzyme rather than its catalytic function.
In classic form, the enzyme is deficient in all tissues, but the liver is rarely enlarged, except as a result of heart failure. Hypoglycemia and acidosis do not occur. Death usually occurs in the first year of life. In the second type, the infantile form, there are traces of acid maltase activity, cardiomyopathy is less severe and there is no left ventricular outflow obstruction[151,152]. In juvenile and adult forms disease severity increases with disease duration, but is not related to the age of the patients. However, there is a subset of patients under age 15 years with a more severe disease, requiring increased use of ventilatory support, wheelchair support, and nutritional support. Wolff-Parkinson-Syndrome and second degree atrioventricular block may be due to GSD type II[153]. Accumulation of glycogen in vascular smooth muscle may cause the development and rupture of aneurysm[154]. Severe infantile and asymptomatic adult forms have been reported in 2 generations of the same family[155].
Laboratory testing reveals elevations in CK, aldolase, ALT, AST, and lactate dehydrogenase. ALT and AST usually represent the muscle fraction. CK elevation is a sensitive test for diagnosis[156]. It is abnormal in more than 95% of the patients. The final diagnosis is established after measuring the enzyme activity in skin fibroblasts or muscle or demonstrating the mutation.
A high-protein, low-carbohydrate diet is beneficial in adult patients[157,158]. In 2001, recombinant alpha-glucosidase infusion improved cardiac function and skeletal muscle functions[159]. This resulted in approval of enzyme replacement therapy for Pompe disease in 2006. Furthermore, the development of experimental therapies, such as adeno-associated virus vector-mediated gene therapy, holds promise for the availability of curative therapy in GSD I and GSD II/Pompe disease in the future[57].
Glycogen storage disease subtypes V (GSD-V; McArdle disease; Myophosphorylase deficiency; Muscle glycogen phosphorylase deficiency) is caused by mutation in the gene encoding muscle glycogen phosphorylase, localized to 11q13 by fluorescence in situ hybridization[160]. The clinical symptoms usually begin in young adulthood with exercise intolerance and muscle cramps. Transient myoglobinuria due to rhabdomyolysis may occur after exercise and may cause acute renal failure. Patients may report progressive muscle weakness, myalgia, and lack of endurance since childhood or adolescence[161].
The gene responsible for glycogen storage disease type VII(GSD-VII; Tarui disease; Muscle phosphofructokinase deficiency; Glycogen storage disease of muscle) is on chromosome 12q13.3[162]. Muscle cramps and myoglobinuria with exercise are features of glycogen storage disease type VII as in McArdle disease. At rest no abnormalities are found on neurologic examination. Weakness and stiffness invariably appear in muscle groups subjected to vigorous or prolonged exertion. Upon ischemic exercise test, venous lactate fails to rise. Myoglobinuria may occur after exercise[163].
| 1. | Roach PJ. Glycogen and its metabolism. Curr Mol Med. 2002;2:101-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 347] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 2. | Saltik IN, Ozen H, Ciliv G, Koçak N, Yüce A, Gürakan F, Dinler G. Glycogen storage disease type Ia: frequency and clinical course in Turkish children. Indian J Pediatr. 2000;67:497-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Applegarth DA, Toone JR, Lowry RB. Incidence of inborn errors of metabolism in British Columbia, 1969-1996. Pediatrics. 2000;105:e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 279] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 4. | Chen YT. Glycogen storage diseases. The metabolic & molecular basis of inherited diseases. New York: McGraw-Hill 2001; 1521-1552. |
| 5. | Lewis GM, Spencer-Peet J, Stewart KM. Infantile hypoglycaemia due to inherited deficiency of glycogen synthetase in liver. Arch Dis Child. 1963;38:40-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 50] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Orho M, Bosshard NU, Buist NR, Gitzelmann R, Aynsley-Green A, Blümel P, Gannon MC, Nuttall FQ, Groop LC. Mutations in the liver glycogen synthase gene in children with hypoglycemia due to glycogen storage disease type 0. J Clin Invest. 1998;102:507-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Laberge AM, Mitchell GA, van de Werve G, Lambert M. Long-term follow-up of a new case of liver glycogen synthase deficiency. Am J Med Genet A. 2003;120A:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Weinstein DA, Correia CE, Saunders AC, Wolfsdorf JI. Hepatic glycogen synthase deficiency: an infrequently recognized cause of ketotic hypoglycemia. Mol Genet Metab. 2006;87:284-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Bachrach BE, Weinstein DA, Orho-Melander M, Burgess A, Wolfsdorf JI. Glycogen synthase deficiency (glycogen storage disease type 0) presenting with hyperglycemia and glucosuria: report of three new mutations. J Pediatr. 2002;140:781-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | van Schaftingen E, Gerin I. The glucose-6-phosphatase system. Biochem J. 2002;362:513-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 183] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 11. | Ekstein J, Rubin BY, Anderson SL, Weinstein DA, Bach G, Abeliovich D, Webb M, Risch N. Mutation frequencies for glycogen storage disease Ia in the Ashkenazi Jewish population. Am J Med Genet A. 2004;129A:162-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 12. | CORIGT , CORICF . Glucose-6-phosphatase of the liver in glycogen storage disease. J Biol Chem. 1952;199:661-667. [PubMed] |
| 13. | Brody LC, Abel KJ, Castilla LH, Couch FJ, McKinley DR, Yin G, Ho PP, Merajver S, Chandrasekharappa SC, Xu J. Construction of a transcription map surrounding the BRCA1 locus of human chromosome 17. Genomics. 1995;25:238-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Lei KJ, Pan CJ, Shelly LL, Liu JL, Chou JY. Identification of mutations in the gene for glucose-6-phosphatase, the enzyme deficient in glycogen storage disease type 1a. J Clin Invest. 1994;93:1994-1999. [PubMed] |
| 15. | Yang Chou J BC. Molecular Genetics of Type 1 Glycogen Storage Diseases. Trends Endocrinol Metab. 1999;10:104-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Rake JP, Visser G, Labrune P, Leonard JV, Ullrich K, Smit GP. Glycogen storage disease type I: diagnosis, management, clinical course and outcome. Results of the European Study on Glycogen Storage Disease Type I(ESGSD I). Eur J Pediatr. 2002;161 Suppl 1:S20-S34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 189] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 17. | Rake JP, Visser G, Labrune P, Leonard JV, Ullrich K, Smit GP. Guidelines for management of glycogen storage disease type I- European Study on Glycogen Storage Disease Type I(ESGSD I). Eur J Pediatr. 2002;161 Suppl 1:S112-S119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 109] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Visser G, Rake JP, Kokke FT, Nikkels PG, Sauer PJ, Smit GP. Intestinal function in glycogen storage disease type I. J Inherit Metab Dis. 2002;25:261-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Pabuçcuoğlu A, Aydoğdu S, Baş M. Serum biotinidase activity in children with chronic liver disease and its clinical significance. J Pediatr Gastroenterol Nutr. 2002;34:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Saltik IN, Ozen H, Koçak N, Yüce A, Gürakan F. High biotinidase activity in type Ia glycogen storage disease. Am J Gastroenterol. 2000;95:2144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Burlina AB, Dermikol M, Mantau A, Piovan S, Grazian L, Zacchello F, Shin Y. Increased plasma biotinidase activity in patients with glycogen storage disease type Ia: effect of biotin supplementation. J Inherit Metab Dis. 1996;19:209-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Göğüş S, Koçak N, Ciliv G, Karabulut E, Akçören Z, Kale G, Cağlar M. Histologic features of the liver in type Ia glycogen storage disease: comparative study between different age groups and consecutive biopsies. Pediatr Dev Pathol. 2002;5:299-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 23. | Smit GP. The long-term outcome of patients with glycogen storage disease type Ia. Eur J Pediatr. 1993;152 Suppl 1:S52-S55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Talente GM, Coleman RA, Alter C, Baker L, Brown BI, Cannon RA, Chen YT, Crigler JF, Ferreira P, Haworth JC. Glycogen storage disease in adults. Ann Intern Med. 1994;120:218-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 141] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 25. | Chen YT, Coleman RA, Scheinman JI, Kolbeck PC, Sidbury JB. Renal disease in type Iglycogen storage disease. N Engl J Med. 1988;318:7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 118] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Lin CC, Tsai JD, Lin SP, Lee HC. Renal sonographic findings of type Iglycogen storage disease in infancy and early childhood. Pediatr Radiol. 2005;35:786-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Restaino I, Kaplan BS, Stanley C, Baker L. Nephrolithiasis, hypocitraturia, and a distal renal tubular acidification defect in type 1 glycogen storage disease. J Pediatr. 1993;122:392-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Reitsma-Bierens WC. Renal complications in glycogen storage disease type I. Eur J Pediatr. 1993;152 Suppl 1:S60-S62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Cabrera-Abreu J, Crabtree NJ, Elias E, Fraser W, Cramb R, Alger S. Bone mineral density and markers of bone turnover in patients with glycogen storage disease types I, IIIand IX. J Inherit Metab Dis. 2004;27:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Miller JH, Gates GF, Landing BH, Kogut MD, Roe TF. Scintigraphic abnormalities in glycogen storage disease. J Nucl Med. 1978;19:354-358. [PubMed] |
| 31. | Zangeneh F, Limbeck GA, Brown BI, Emch JR, Arcasoy MM, Goldenberg VE, Kelley VC. Hepatorenal glycogenosis (type Iglycogenosis) and carcinoma of the liver. J Pediatr. 1969;74:73-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 42] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Fraumeni JF, Rosen PJ, Hull EW, Barth RF, Shapiro SR, O'Connor JF. Hepatoblastoma in infant sisters. Cancer. 1969;24:1086-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 33. | Lee P, Mather S, Owens C, Leonard J, Dicks-Mireaux C. Hepatic ultrasound findings in the glycogen storage diseases. Br J Radiol. 1994;67:1062-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Franco LM, Krishnamurthy V, Bali D, Weinstein DA, Arn P, Clary B, Boney A, Sullivan J, Frush DP, Chen YT. Hepatocellular carcinoma in glycogen storage disease type Ia: a case series. J Inherit Metab Dis. 2005;28:153-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 146] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 35. | Bianchi L. Glycogen storage disease Iand hepatocellular tumours. Eur J Pediatr. 1993;152 Suppl 1:S63-S70. [PubMed] |
| 36. | Trioche P, Francoual J, Capel L, Odièvre M, Lindenbaum A, Labrune P. Apolipoprotein E polymorphism and serum concentrations in patients with glycogen storage disease type Ia. J Inherit Metab Dis. 2000;23:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Mühlhausen C, Schneppenheim R, Budde U, Merkel M, Muschol N, Ullrich K, Santer R. Decreased plasma concentration of von Willebrand factor antigen (VWF: Ag) in patients with glycogen storage disease type Ia. J Inherit Metab Dis. 2005;28:945-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 38. | Hutton RA, Macnab AJ, Rivers RP. Defect of platelet function associated with chronic hypoglycaemia. Arch Dis Child. 1976;51:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 39. | Wittenstein B, Klein M, Finckh B, Ullrich K, Kohlschütter A. Radical trapping in glycogen storage disease 1a. Eur J Pediatr. 2002;161 Suppl 1:S70-S74. [PubMed] |
| 40. | Wittenstein B, Klein M, Finckh B, Ullrich K, Kohlschütter A. Plasma antioxidants in pediatric patients with glycogen storage disease, diabetes mellitus, and hypercholesterolemia. Free Radic Biol Med. 2002;33:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 41. | Melis D, Parenti G, Della Casa R, Sibilio M, Romano A, Di Salle F, Elefante R, Mansi G, Santoro L, Perretti A. Brain damage in glycogen storage disease type I. J Pediatr. 2004;144:637-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 42. | Ryan IP, Havel RJ, Laros RK. Three consecutive pregnancies in a patient with glycogen storage disease type IA (von Gierke's disease). Am J Obstet Gynecol. 1994;170:1687-1690; discussion 1690-1691. [PubMed] |
| 43. | Lei KJ, Chen YT, Chen H, Wong LJ, Liu JL, McConkie-Rosell A, Van Hove JL, Ou HC, Yeh NJ, Pan LY. Genetic basis of glycogen storage disease type 1a: prevalent mutations at the glucose-6-phosphatase locus. Am J Hum Genet. 1995;57:766-771. [PubMed] |
| 44. | Hüner G, Podskarbi T, Schütz M, Baykal T, Sarbat G, Shin YS, Demirkol M. Molecular aspects of glycogen storage disease type Ia in Turkish patients: a novel mutation in the glucose-6-phosphatase gene. J Inherit Metab Dis. 1998;21:445-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 45. | Terzioglu M, Emre S, Ozen H, Saltik IN, Koçak N, Ciliv G, Yüce A, Gürakan F. Glucose-6-phosphatase gene mutations in Turkish patients with glycogen storage disease type Ia. J Inherit Metab Dis. 2001;24:881-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 46. | Duarte IF, Goodfellow BJ, Barros A, Jones JG, Barosa C, Diogo L, Garcia P, Gil AM. Metabolic characterisation of plasma in juveniles with glycogen storage disease type 1a (GSD1a) by high-resolution (1)H NMR spectroscopy. NMR Biomed. 2007;20:401-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 47. | Qu Y, Abdenur JE, Eng CM, Desnick RJ. Molecular prenatal diagnosis of glycogen storage disease type Ia. Prenat Diagn. 1996;16:333-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 48. | Chen YT, Cornblath M, Sidbury JB. Cornstarch therapy in type Iglycogen-storage disease. N Engl J Med. 1984;310:171-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 184] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 49. | Lee PJ, Dixon MA, Leonard JV. Uncooked cornstarch--efficacy in type Iglycogenosis. Arch Dis Child. 1996;74:546-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 50. | Milla PJ, Atherton DA, Leonard JV, Wolff OH, Lake BD. Disordered intestinal function in glycogen storage disease. J Inherit Metab Dis. 1978;1:155-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Pears J, Jung RT, Jankowski J, Waddell ID, Burchell A. Glucose-6-phosphatase in normal adult human intestinal mucosa. Clin Sci (Lond). 1992;83:683-687. [PubMed] |
| 52. | Bodamer OA, Feillet F, Lane RE, Lee PJ, Dixon MA, Halliday D, Leonard JV. Utilization of cornstarch in glycogen storage disease type Ia. Eur J Gastroenterol Hepatol. 2002;14:1251-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 53. | Ozen H, Ciliv G, Koçak N, Saltik IN, Yüce A, Gürakan F. Short-term effect of captopril on microalbuminuria in children with glycogen storage disease type Ia. J Inherit Metab Dis. 2000;23:459-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 54. | Giannì ML, Bonvissuto M, Gallieni M, Testolin C, Racchi E, Riva E. Ramipril treatment in a patient with glycogen storage disease Inon-A. J Inherit Metab Dis. 2002;25:515-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 55. | Baker L, Kern EFO, Olshan J, Goldfarb S, Dahlem ST. Pilot study of captopril in patients with renal disease associated with glycogen storage disease type I(GSDI). Pediatr Res. 1988;23:388A. |
| 56. | Nuoffer JM, Mullis PE, Wiesmann UN. Treatment with low-dose diazoxide in two growth-retarded prepubertal girls with glycogen storage disease type Ia resulted in catch-up growth. J Inherit Metab Dis. 1997;20:790-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 57. | Koeberl DD, Kishnani PS, Chen YT. Glycogen storage disease types Iand II: treatment updates. J Inherit Metab Dis. 2007;30:159-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 58. | Faivre L, Houssin D, Valayer J, Brouard J, Hadchouel M, Bernard O. Long-term outcome of liver transplantation in patients with glycogen storage disease type Ia. J Inherit Metab Dis. 1999;22:723-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 53] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 59. | Liu PP, de Villa VH, Chen YS, Wang CC, Wang SH, Chiang YC, Jawan B, Cheung HK, Cheng YF, Huang TL. Outcome of living donor liver transplantation for glycogen storage disease. Transplant Proc. 2003;35:366-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 60. | Matern D, Starzl TE, Arnaout W, Barnard J, Bynon JS, Dhawan A, Emond J, Haagsma EB, Hug G, Lachaux A. Liver transplantation for glycogen storage disease types I, III, and IV. Eur J Pediatr. 1999;158 Suppl 2:S43-S48. [PubMed] |
| 61. | Emmett M, Narins RG. Renal tranplantation in type 1 glycogenosis. Failure to improve glucose metabolism. JAMA. 1978;239:1642-1644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 62. | Senior B, Loridan L. Functional differentiation of glycogenoses of the liver with respect to the use of glycerol. N Engl J Med. 1968;279:965-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 63. | Arion WJ, Wallin BK, Lange AJ, Ballas LM. On the involvement of a glucose 6-phosphate transport system in the function of microsomal glucose 6-phosphatase. Mol Cell Biochem. 1975;6:75-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 187] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 64. | Annabi B, Hiraiwa H, Mansfield BC, Lei KJ, Ubagai T, Polymeropoulos MH, Moses SW, Parvari R, Hershkovitz E, Mandel H. The gene for glycogen-storage disease type 1b maps to chromosome 11q23. Am J Hum Genet. 1998;62:400-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 85] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 65. | Ihara K, Kuromaru R, Hara T. Genomic structure of the human glucose 6-phosphate translocase gene and novel mutations in the gene of a Japanese patient with glycogen storage disease type Ib. Hum Genet. 1998;103:493-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 66. | Visser G, Rake JP, Fernandes J, Labrune P, Leonard JV, Moses S, Ullrich K, Smit GP. Neutropenia, neutrophil dysfunction, and inflammatory bowel disease in glycogen storage disease type Ib: results of the European Study on Glycogen Storage Disease type I. J Pediatr. 2000;137:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 165] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 67. | Ihara K, Nomura A, Hikino S, Takada H, Hara T. Quantitative analysis of glucose-6-phosphate translocase gene expression in various human tissues and haematopoietic progenitor cells. J Inherit Metab Dis. 2000;23:583-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 68. | Ueno N, Tomita M, Ariga T, Ohkawa M, Nagano S, Takahashi Y, Arashima S, Matsumoto S. Impaired monocyte function in glycogen storage disease type Ib. Eur J Pediatr. 1986;145:312-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 69. | Leuzzi R, Bánhegyi G, Kardon T, Marcolongo P, Capecchi PL, Burger HJ, Benedetti A, Fulceri R. Inhibition of microsomal glucose-6-phosphate transport in human neutrophils results in apoptosis: a potential explanation for neutrophil dysfunction in glycogen storage disease type 1b. Blood. 2003;101:2381-2387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 70. | Kure S, Hou DC, Suzuki Y, Yamagishi A, Hiratsuka M, Fukuda T, Sugie H, Kondo N, Matsubara Y, Narisawa K. Glycogen storage disease type Ib without neutropenia. J Pediatr. 2000;137:253-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 71. | Roe TF, Thomas DW, Gilsanz V, Isaacs H, Atkinson JB. Inflammatory bowel disease in glycogen storage disease type Ib. J Pediatr. 1986;109:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 72. | Saltik-Temizel IN, Koçak N, Ozen H, Yüce A, Gürakan F, Demir H. Inflammatory bowel disease-like colitis in a young Turkish child with glycogen storage disease type 1b and elevated platelet count. Turk J Pediatr. 2005;47:180-182. [PubMed] |
| 73. | Melis D, Fulceri R, Parenti G, Marcolongo P, Gatti R, Parini R, Riva E, Della Casa R, Zammarchi E, Andria G. Genotype/phenotype correlation in glycogen storage disease type 1b: a multicentre study and review of the literature. Eur J Pediatr. 2005;164:501-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 74. | Martin AP, Bartels M, Schreiber S, Buehrdel P, Hauss J, Fangmann J. Successful staged kidney and liver transplantation for glycogen storage disease type Ib: A case report. Transplant Proc. 2006;38:3615-3619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 75. | Melis D, Pivonello R, Parenti G, Della Casa R, Salerno M, Lombardi G, Sebastio G, Colao A, Andria G. Increased prevalence of thyroid autoimmunity and hypothyroidism in patients with glycogen storage disease type I. J Pediatr. 2007;150:300-305, 305.e1. [PubMed] |
| 76. | Narisawa K, Otomo H, Igarashi Y, Arai N, Otake M, Tada K, Kuzuya T. Glycogen storage disease type 1b: microsomal glucose-6-phosphatase system in two patients with different clinical findings. Pediatr Res. 1983;17:545-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 77. | Kovacevic A, Ehrlich R, Mayatepek E, Wendel U, Schwahn B. Glycogen storage disease type Ib without hypoglycemia. Mol Genet Metab. 2007;90:349-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 78. | Greene HL, Slonim AE, O'Neill JA, Burr IM. Continuous nocturnal intragastric feeding for management of type 1 glycogen-storage disease. N Engl J Med. 1976;294:423-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 138] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 79. | Schroten H, Roesler J, Breidenbach T, Wendel U, Elsner J, Schweitzer S, Zeidler C, Burdach S, Lohmann-Matthes ML, Wahn V. Granulocyte and granulocyte-macrophage colony-stimulating factors for treatment of neutropenia in glycogen storage disease type Ib. J Pediatr. 1991;119:748-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 36] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 80. | Roe TF, Coates TD, Thomas DW, Miller JH, Gilsanz V. Brief report: treatment of chronic inflammatory bowel disease in glycogen storage disease type Ib with colony-stimulating factors. N Engl J Med. 1992;326:1666-1669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 71] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 81. | Yiu WH, Pan CJ, Allamarvdasht M, Kim SY, Chou JY. Glucose-6-phosphate transporter gene therapy corrects metabolic and myeloid abnormalities in glycogen storage disease type Ib mice. Gene Ther. 2007;14:219-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 82. | Fenske CD, Jeffery S, Weber JL, Houlston RS, Leonard JV, Lee PJ. Localisation of the gene for glycogen storage disease type 1c by homozygosity mapping to 11q. J Med Genet. 1998;35:269-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 83. | Veiga-da-Cunha M, Gerin I, Chen YT, Lee PJ, Leonard JV, Maire I, Wendel U, Vikkula M, Van Schaftingen E. The putative glucose 6-phosphate translocase gene is mutated in essentially all cases of glycogen storage disease type Inon-a. Eur J Hum Genet. 1999;7:717-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 68] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 84. | Galli L, Orrico A, Marcolongo P, Fulceri R, Burchell A, Melis D, Parini R, Gatti R, Lam C, Benedetti A. Mutations in the glucose-6-phosphate transporter (G6PT) gene in patients with glycogen storage diseases type 1b and 1c. FEBS Lett. 1999;459:255-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 85. | Melis D, Havelaar AC, Verbeek E, Smit GP, Benedetti A, Mancini GM, Verheijen F. NPT4, a new microsomal phosphate transporter: mutation analysis in glycogen storage disease type Ic. J Inherit Metab Dis. 2004;27:725-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 86. | Shen JJ, Chen YT. Molecular characterization of glycogen storage disease type III. Curr Mol Med. 2002;2:167-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 62] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 87. | Bao Y, Dawson TL, Chen YT. Human glycogen debranching enzyme gene (AGL): complete structural organization and characterization of the 5' flanking region. Genomics. 1996;38:155-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 88. | Bao Y, Yang BZ, Dawson TL, Chen YT. Isolation and nucleotide sequence of human liver glycogen debranching enzyme mRNA: identification of multiple tissue-specific isoforms. Gene. 1997;197:389-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 89. | Parvari R, Moses S, Shen J, Hershkovitz E, Lerner A, Chen YT. A single-base deletion in the 3'-coding region of glycogen-debranching enzyme is prevalent in glycogen storage disease type IIIA in a population of North African Jewish patients. Eur J Hum Genet. 1997;5:266-270. [PubMed] |
| 90. | Santer R, Kinner M, Steuerwald U, Kjaergaard S, Skovby F, Simonsen H, Shaiu WL, Chen YT, Schneppenheim R, Schaub J. Molecular genetic basis and prevalence of glycogen storage disease type IIIA in the Faroe Islands. Eur J Hum Genet. 2001;9:388-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 91. | Shen J, Bao Y, Liu HM, Lee P, Leonard JV, Chen YT. Mutations in exon 3 of the glycogen debranching enzyme gene are associated with glycogen storage disease type IIIthat is differentially expressed in liver and muscle. J Clin Invest. 1996;98:352-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 91] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 92. | Van Hoof F, Hers HG. The subgroups of type 3 glycogenosis. Eur J Biochem. 1967;2:265-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 96] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 93. | Ding JH, de Barsy T, Brown BI, Coleman RA, Chen YT. Immunoblot analyses of glycogen debranching enzyme in different subtypes of glycogen storage disease type III. J Pediatr. 1990;116:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 54] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 94. | Momoi T, Sano H, Yamanaka C, Sasaki H, Mikawa H. Glycogen storage disease type IIIwith muscle involvement: reappraisal of phenotypic variability and prognosis. Am J Med Genet. 1992;42:696-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 95. | Coleman RA, Winter HS, Wolf B, Chen YT. Glycogen debranching enzyme deficiency: long-term study of serum enzyme activities and clinical features. J Inherit Metab Dis. 1992;15:869-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 96. | Lucchiari S, Pagliarani S, Salani S, Filocamo M, Di Rocco M, Melis D, Rodolico C, Musumeci O, Toscano A, Bresolin N. Hepatic and neuromuscular forms of glycogenosis type III: nine mutations in AGL. Hum Mutat. 2006;27:600-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 97. | Moses SW, Wanderman KL, Myroz A, Frydman M. Cardiac involvement in glycogen storage disease type III. Eur J Pediatr. 1989;148:764-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 98. | Cleary MA, Walter JH, Kerr BA, Wraith JE. Facial appearance in glycogen storage disease type III. Clin Dysmorphol. 2002;11:117-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 99. | Coleman RA, Winter HS, Wolf B, Gilchrist JM, Chen YT. Glycogen storage disease type III(glycogen debranching enzyme deficiency): correlation of biochemical defects with myopathy and cardiomyopathy. Ann Intern Med. 1992;116:896-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 58] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 100. | Lee P, Burch M, Leonard JV. Plasma creatine kinase and cardiomyopathy in glycogen storage disease type III. J Inherit Metab Dis. 1995;18:751-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 101. | Demo E, Frush D, Gottfried M, Koepke J, Boney A, Bali D, Chen YT, Kishnani PS. Glycogen storage disease type III-hepatocellular carcinoma a long-term complication? J Hepatol. 2007;46:492-498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 90] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 102. | ANDERSEN DH. Familial cirrhosis of the liver with storage of abnormal glycogen. Lab Invest. 1956;5:11-20. [PubMed] |
| 103. | Brown BI, Brown DH. Lack of an alpha-1,4-glucan: alpha-1,4-glucan 6-glycosyl transferase in a case of type IV glycogenosis. Proc Natl Acad Sci USA. 1966;56:725-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 86] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 104. | Moses SW, Parvari R. The variable presentations of glycogen storage disease type IV: a review of clinical, enzymatic and molecular studies. Curr Mol Med. 2002;2:177-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 104] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 105. | Thon VJ, Khalil M, Cannon JF. Isolation of human glycogen branching enzyme cDNAs by screening complementation in yeast. J Biol Chem. 1993;268:7509-7513. [PubMed] |
| 106. | L'herminé-Coulomb A, Beuzen F, Bouvier R, Rolland MO, Froissart R, Menez F, Audibert F, Labrune P. Fetal type IV glycogen storage disease: clinical, enzymatic, and genetic data of a pure muscular form with variable and early antenatal manifestations in the same family. Am J Med Genet A. 2005;139A:118-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 107. | Greene HL, Brown BI, McClenathan DT, Agostini RM, Taylor SR. A new variant of type IV glycogenosis: deficiency of branching enzyme activity without apparent progressive liver disease. Hepatology. 1988;8:302-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 108. | Schröder JM, May R, Shin YS, Sigmund M, Nase-Hüppmeier S. Juvenile hereditary polyglucosan body disease with complete branching enzyme deficiency (type IV glycogenosis). Acta Neuropathol. 1993;85:419-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 109. | Servidei S, Riepe RE, Langston C, Tani LY, Bricker JT, Crisp-Lindgren N, Travers H, Armstrong D, DiMauro S. Severe cardiopathy in branching enzyme deficiency. J Pediatr. 1987;111:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 64] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 110. | Bruno C, van Diggelen OP, Cassandrini D, Gimpelev M, Giuffrè B, Donati MA, Introvini P, Alegria A, Assereto S, Morandi L. Clinical and genetic heterogeneity of branching enzyme deficiency (glycogenosis type IV). Neurology. 2004;63:1053-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 87] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 111. | Alegria A, Martins E, Dias M, Cunha A, Cardoso ML, Maire I. Glycogen storage disease type IV presenting as hydrops fetalis. J Inherit Metab Dis. 1999;22:330-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 112. | Zellweger H, Mueller S, Ionasescu V, Schochet SS, McCormick WF. Glycogenosis. IV. A new cause of infantile hypotonia. J Pediatr. 1972;80:842-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 113. | McMaster KR, Powers JM, Hennigar GR, Wohltmann HJ, Farr GH. Nervous system involvement in type IV glycogenosis. Arch Pathol Lab Med. 1979;103:105-111. [PubMed] |
| 114. | Giuffrè B, Parini R, Rizzuti T, Morandi L, van Diggelen OP, Bruno C, Giuffrè M, Corsello G, Mosca F. Severe neonatal onset of glycogenosis type IV: clinical and laboratory findings leading to diagnosis in two siblings. J Inherit Metab Dis. 2004;27:609-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 115. | Reusche E, Aksu F, Goebel HH, Shin YS, Yokota T, Reichmann H. A mild juvenile variant of type IV glycogenosis. Brain Dev. 1992;14:36-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 116. | Ferguson IT, Mahon M, Cumming WJ. An adult case of Andersen's disease--Type IV glycogenosis. A clinical, histochemical, ultrastructural and biochemical study. J Neurol Sci. 1983;60:337-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 28] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 117. | Shin YS, Steigüber H, Klemm P, Endres W, Schwab O, Wolff G. Branching enzyme in erythrocytes. Detection of type IV glycogenosis homozygotes and heterozygotes. J Inherit Metab Dis. 1988;11 Suppl 2:252-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 118. | Lossos A, Barash V, Soffer D, Argov Z, Gomori M, Ben-Nariah Z, Abramsky O, Steiner I. Hereditary branching enzyme dysfunction in adult polyglucosan body disease: a possible metabolic cause in two patients. Ann Neurol. 1991;30:655-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 60] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 119. | Selby R, Starzl TE, Yunis E, Brown BI, Kendall RS, Tzakis A. Liver transplantation for type IV glycogen storage disease. N Engl J Med. 1991;324:39-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 49] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 120. | Starzl TE, Demetris AJ, Trucco M, Ricordi C, Ildstad S, Terasaki PI, Murase N, Kendall RS, Kocova M, Rudert WA. Chimerism after liver transplantation for type IV glycogen storage disease and type 1 Gaucher's disease. N Engl J Med. 1993;328:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 182] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 121. | Newgard CB, Fletterick RJ, Anderson LA, Lebo RV. The polymorphic locus for glycogen storage disease VI(liver glycogen phosphorylase) maps to chromosome 14. Am J Hum Genet. 1987;40:351-364. [PubMed] |
| 122. | Hers HG. Enzymatic studies of hepatic fragments; application to the classification of glycogenoses. Rev Int Hepatol. 1959;9:35-55. [PubMed] |
| 123. | Tang NL, Hui J, Young E, Worthington V, To KF, Cheung KL, Li CK, Fok TF. A novel mutation (G233D) in the glycogen phosphorylase gene in a patient with hepatic glycogen storage disease and residual enzyme activity. Mol Genet Metab. 2003;79:142-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 124. | Burwinkel B, Bakker HD, Herschkovitz E, Moses SW, Shin YS, Kilimann MW. Mutations in the liver glycogen phosphorylase gene (PYGL) underlying glycogenosis type VI. Am J Hum Genet. 1998;62:785-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 68] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 125. | Davidson JJ, Ozçelik T, Hamacher C, Willems PJ, Francke U, Kilimann MW. cDNA cloning of a liver isoform of the phosphorylase kinase alpha subunit and mapping of the gene to Xp22.2-p22.1, the region of human X-linked liver glycogenosis. Proc Natl Acad Sci USA. 1992;89:2096-2100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 126. | Hendrickx J, Willems PJ. Genetic deficiencies of the glycogen phosphorylase system. Hum Genet. 1996;97:551-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 127. | Van den Berg IE, Berger R. Phosphorylase b kinase deficiency in man: a review. J Inherit Metab Dis. 1990;13:442-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 128. | Hidaka F, Sawada H, Matsuyama M, Nunoi H. A novel mutation of the PHKA2 gene in a patient with X-linked liver glycogenosis type 1. Pediatr Int. 2005;47:687-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 129. | Schimke RN, Zakheim RM, Corder RC, Hug G. Glycogen storage disease type IX: benign glycogenosis of liver and hepatic phosphorylase kinase deficiency. J Pediatr. 1973;83:1031-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 130. | Willems PJ, Gerver WJ, Berger R, Fernandes J. The natural history of liver glycogenosis due to phosphorylase kinase deficiency: a longitudinal study of 41 patients. Eur J Pediatr. 1990;149:268-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 57] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 131. | Schippers HM, Smit GP, Rake JP, Visser G. Characteristic growth pattern in male X-linked phosphorylase-b kinase deficiency (GSD IX). J Inherit Metab Dis. 2003;26:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 132. | Burwinkel B, Amat L, Gray RG, Matsuo N, Muroya K, Narisawa K, Sokol RJ, Vilaseca MA, Kilimann MW. Variability of biochemical and clinical phenotype in X-linked liver glycogenosis with mutations in the phosphorylase kinase PHKA2 gene. Hum Genet. 1998;102:423-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (3)] |
| 133. | Hendrickx J, Coucke P, Hors-Cayla MC, Smit GP, Shin YS, Deutsch J, Smeitink J, Berger R, Lee P, Fernandes J. Localization of a new type of X-linked liver glycogenosis to the chromosomal region Xp22 containing the liver alpha-subunit of phosphorylase kinase (PHKA2). Genomics. 1994;21:620-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 134. | Burwinkel B, Maichele AJ, Aagenaes O, Bakker HD, Lerner A, Shin YS, Strachan JA, Kilimann MW. Autosomal glycogenosis of liver and muscle due to phosphorylase kinase deficiency is caused by mutations in the phosphorylase kinase beta subunit (PHKB). Hum Mol Genet. 1997;6:1109-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 135. | Bashan N, Iancu TC, Lerner A, Fraser D, Potashnik R, Moses SW. Glycogenosis due to liver and muscle phosphorylase kinase deficiency. Pediatr Res. 1981;15:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 136. | Maichele AJ, Burwinkel B, Maire I, Søvik O, Kilimann MW. Mutations in the testis/liver isoform of the phosphorylase kinase gamma subunit (PHKG2) cause autosomal liver glycogenosis in the gsd rat and in humans. Nat Genet. 1996;14:337-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 54] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 137. | Burwinkel B, Shiomi S, Al Zaben A, Kilimann MW. Liver glycogenosis due to phosphorylase kinase deficiency: PHKG2 gene structure and mutations associated with cirrhosis. Hum Mol Genet. 1998;7:149-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 138. | Manz F, Bickel H, Brodehl J, Feist D, Gellissen K, Geschöll-Bauer B, Gilli G, Harms E, Helwig H, Nützenadel W. Fanconi-Bickel syndrome. Pediatr Nephrol. 1987;1:509-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 62] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 139. | Fanconi G, Bickel H. Not Available. Helv Paediatr Acta. 1949;4:359-396. [PubMed] |
| 140. | Saltik-Temizel IN, Coşkun T, Yüce A, Koçak N. Fanconi-Bickel syndrome in three Turkish patients with different homozygous mutations. Turk J Pediatr. 2005;47:167-169. [PubMed] |
| 141. | Fukumoto H, Seino S, Imura H, Seino Y, Eddy RL, Fukushima Y, Byers MG, Shows TB, Bell GI. Sequence, tissue distribution, and chromosomal localization of mRNA encoding a human glucose transporter-like protein. Proc Natl Acad Sci USA. 1988;85:5434-5438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 286] [Article Influence: 7.5] [Reference Citation Analysis (1)] |
| 142. | Santer R, Schneppenheim R, Dombrowski A, Götze H, Steinmann B, Schaub J. Mutations in GLUT2, the gene for the liver-type glucose transporter, in patients with Fanconi-Bickel syndrome. Nat Genet. 1997;17:324-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 190] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 143. | Aperia A, Bergqvist G, Linné T, Zetterström R. Familial Fanconi syndrome with malabsorption and galactose intolerance, normal kinase and transferase activity. A report on two siblings. Acta Paediatr Scand. 1981;70:527-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 144. | Müller D, Santer R, Krawinkel M, Christiansen B, Schaub J. Fanconi-Bickel syndrome presenting in neonatal screening for galactosaemia. J Inherit Metab Dis. 1997;20:607-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 145. | Lee PJ, Van't Hoff WG, Leonard JV. Catch-up growth in Fanconi-Bickel syndrome with uncooked cornstarch. J Inherit Metab Dis. 1995;18:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 146. | Odievre M. Hepato-renal glycogenosis with complex tubulopathy. 2. Cases of a new entity. Rev Int Hepatol. 1966;16:1-70. [PubMed] |
| 147. | Haines JL, Ozelius LJ, McFarlane H, Menon A, Tzall S, Martiniuk F, Hirschhorn R, Gusella JF. A genetic linkage map of chromosome 17. Genomics. 1990;8:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 148. | Ausems MG, Verbiest J, Hermans MP, Kroos MA, Beemer FA, Wokke JH, Sandkuijl LA, Reuser AJ, van der Ploeg AT. Frequency of glycogen storage disease type IIin The Netherlands: implications for diagnosis and genetic counselling. Eur J Hum Genet. 1999;7:713-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 205] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 149. | Matsuishi T, Yoshino M, Terasawa K, Nonaka I. Childhood acid maltase deficiency. A clinical, biochemical, and morphologic study of three patients. Arch Neurol. 1984;41:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 150. | Reuser AJ, Kroos M, Willemsen R, Swallow D, Tager JM, Galjaard H. Clinical diversity in glycogenosis type II. Biosynthesis and in situ localization of acid alpha-glucosidase in mutant fibroblasts. J Clin Invest. 1987;79:1689-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 77] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 151. | Slonim AE, Bulone L, Ritz S, Goldberg T, Chen A, Martiniuk F. Identification of two subtypes of infantile acid maltase deficiency. J Pediatr. 2000;137:283-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 100] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 152. | Beratis NG, LaBadie GU, Hirschhorn K. Characterization of the molecular defect in infantile and adult acid alpha-glucosidase deficiency fibroblasts. J Clin Invest. 1978;62:1264-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 153. | Francesconi M, Auff E. Cardiac arrhythmias and the adult form of type IIglycogenosis. N Engl J Med. 1982;306:937-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 154. | Makos MM, McComb RD, Hart MN, Bennett DR. Alpha-glucosidase deficiency and basilar artery aneurysm: report of a sibship. Ann Neurol. 1987;22:629-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 56] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 155. | Amartino H, Painceira D, Pomponio RJ, Niizawa G, Sabio Paz V, Blanco M, Chamoles N. Two clinical forms of glycogen-storage disease type IIin two generations of the same family. Clin Genet. 2006;69:187-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 156. | Ausems MG, Lochman P, van Diggelen OP, Ploos van Amstel HK, Reuser AJ, Wokke JH. A diagnostic protocol for adult-onset glycogen storage disease type II. Neurology. 1999;52:851-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 157. | Slonim AE, Coleman RA, McElligot MA, Najjar J, Hirschhorn K, Labadie GU, Mrak R, Evans OB, Shipp E, Presson R. Improvement of muscle function in acid maltase deficiency by high-protein therapy. Neurology. 1983;33:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 158. | Isaacs H, Savage N, Badenhorst M, Whistler T. Acid maltase deficiency: a case study and review of the pathophysiological changes and proposed therapeutic measures. J Neurol Neurosurg Psychiatry. 1986;49:1011-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 159. | Amalfitano A, Bengur AR, Morse RP, Majure JM, Case LE, Veerling DL, Mackey J, Kishnani P, Smith W, McVie-Wylie A. Recombinant human acid alpha-glucosidase enzyme therapy for infantile glycogen storage disease type II: results of a phase I/IIclinical trial. Genet Med. 2001;3:132-138. [PubMed] |
| 160. | Lebo RV, Anderson LA, DiMauro S, Lynch E, Hwang P, Fletterick R. Rare McArdle disease locus polymorphic site on 11q13 contains CpG sequence. Hum Genet. 1990;86:17-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 161. | Grünfeld JP, Ganeval D, Chanard J, Fardeau M, Dreyfus JC. Acute renal failure in McArdle's disease. Report of two cases. N Engl J Med. 1972;286:1237-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 53] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 162. | Howard TD, Akots G, Bowden DW. Physical and genetic mapping of the muscle phosphofructokinase gene (PFKM): reassignment to human chromosome 12q. Genomics. 1996;34:122-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 163. | Tarui S, Okuno G, Ikura Y, Tanaka T, Suda M, Nishikawa M. Phosphofructokinase deficiency in skeletal muscle. A new type of glycogenosis. Biochem Biophys Res Commun. 1965;19:517-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 244] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
S- Editor Zhu LH L- Editor Zhu LH E- Editor Chen GJ