INTRODUCTION
Gastrointestinal stromal tumors (GISTs), which arise primarily in the gut wall, are mesenchymal neoplasms closely related to the interstitial cells of Cajal. GISTs typically carry gain-of-function mutations in genes encoding the KIT receptor tyrosine kinase (CD117) or platelet-derived growth factor receptor α, both of which are involved in cell survival, development and proliferation[1]. Although GISTs can arise at any location in the gastrointestinal tract, they are found most often in the stomach (60%-70%), followed by the small intestine (20%-30%), colon and rectum (5%), and esophagus (< 5%)[2-4].
Bacteria-induced abscess in the gastric wall is extremely rare, and the diagnosis is often late. Prior to the development of sufficient therapy, suppurative gastritis often results in death, with a mortality rate reported between 37% and 84%[5-7]. Here, we report an unusual case of a patient with GIST of the stomach and a giant abscess who experienced undiagnosed fever for two months prior to hospitalization.
CASE REPORT
A 74 year old man presented with fever and abdominal pain in the past two months. On examination, there was fever (38.1°C) and minimal tenderness in the epigastrium, but no jaundice or abnormal lymph node enlargement. The patient was taking no medications and his past medical history was unremarkable. Routine laboratory data on admission showed a white blood cell count of 10 500/mm3,
C-reactive protein of 16.5 mg/dL and an erythrocyte sedimentation rate of 65 mm/h. Other chemistry and liver function tests were normal.
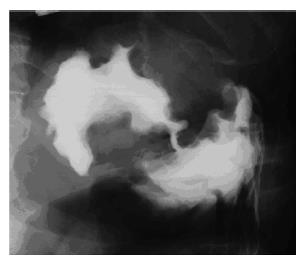
Gastrointestinal endoscopy revealed a gastric submucosal tumor in the fornix, with a fistula to the gastric lumen that was inundated with a great deal of turbid, yellow fluid (Figure 1). The fluid was found to contain abundant Streptococcus intermedius. Examination of the upper gastrointestinal tract X-ray series that included administration of amidotrizoic acid (Gastrografin® Nihon Schering K.K. Osaka Japan) revealed a large cavity, about 7 cm × 8 cm, penetrating into the gastric lumen (Figure 2).
Figure 1 Endoscopic view of a gastric submucosal tumor in the fornix, with a fistula to the gastric lumen.
Within the submucosal tumor was a great deal of turbid, yellow fluid oozing from the fistula.
Figure 2 Upper gastrointestinal tract X-ray revealing a large cavity, about 7 cm × 8 cm, penetrating into the gastric lumen.
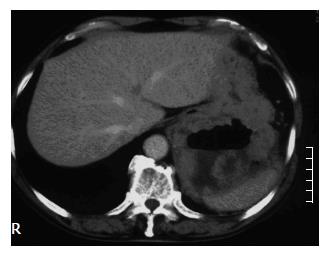
An enhanced computed tomography (CT) scan of the abdomen revealed a large central cavity in the tumor that was partially filled with fluid, and irregular thickening of the gastric wall in the posterior aspect of the fundus (Figure 3). No other visceral abnormalities were found.
Figure 3 Enhanced com-puted tomography (CT) scan of the abdomen revealing a large central cavity in the tumor partially filled with fluid, and an irregular thickening of the gastric wall in the posterior aspect of the fundus extending into the left subphrenic space.
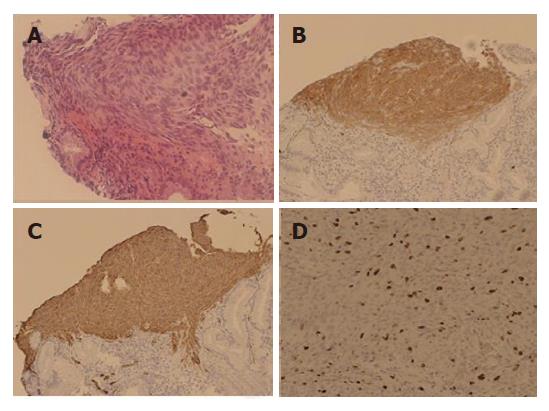
Biopsy specimens taken from the fistula edge during endoscopy resembled a gastric myogenic tumor composed of spindle cells. Immunohistochemical staining for KIT and CD34 was positive, whereas staining for α-smooth-muscle actin, desmin and S-100 protein was negative. The labeling index (L.I) for MIB-1, determined by counting positively stained nuclei among 1000 tumor cells, was about 18% (Figure 4).
Figure 4 Photomicrographs of biopsy specimens from the fistula showing spindle-shaped cells (A) (HE, × 200), immunohistochemical staining showing a diffuse positive signal for KIT (B) (× 100), a diffuse positive signal for CD34 (C) (× 100), and MIB-1 (D).
The labeling index (L.I) was 18% (× 200).
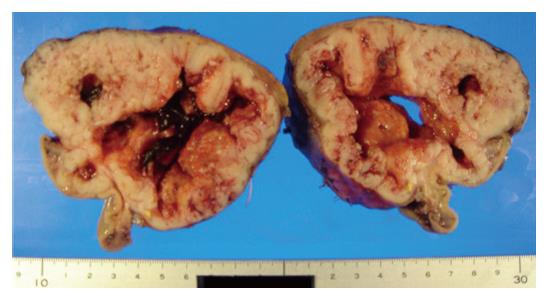
The mass was diagnosed as a GIST accompanied with a giant abscess. The patient was treated by endoscopic drainage of the abscess through the fistula and intravenous administration of antibiotics. Subsequent to improvement in his clinical condition and laboratory tests, a partial gastrectomy (proximal partial gastrectomy) was performed 20 d after admission. Macroscopic examination revealed a 10 cm × 12 cm × 7 cm submucosal, intramural tumor protruding from the serosal surface (Figure 5). The cut surfaces were grayish-white and showed a large amount of central necrosis with a fistula to the gastric lumen. The surgical margins were free of tumor.
Figure 5 Gross appearance of a 10 cm × 12 cm × 7 cm solid tumor with a large amount of central necrosis and a fistula to the gastric lumen.
DISCUSSION
GISTs are the most common mesenchymal tumors of the gastrointestinal tract[8]. In general, tumor size and mitotic index are accepted as two independent prognostic factors for diagnosis[9]. For GISTs, prognostic markers that include size larger than 5 cm, mitotic rate > 5/50, high-power fields (HPF), tumor necrosis and a Ki-67 (MIB-1) index ≥ 10% all are associated with malignancy and high mortality[10,11]. For patients with large or mitotically active gastric GISTs, a MIB-1 proliferative index ≥ 10% is predictive of early recurrence and tumor-related death[12].
Whereas small GISTs (5 cm or less) can be treated by wedge gastric resection, larger tumors may require subtotal or total gastrectomy, including omentectomy. Metastatic or unresectable GISTs are treated with Imanitib mesylate (STI571), a small molecular tyrosine kinase inhibitor of KIT, platelet-delivered growth factor receptor and BCR-ABL. The large size (> 5 cm) and high mitotic count of the tumor in the present case classified it as a high risk. Since cystic degeneration, necrosis and focal hemorrhage generally predominate in larger tumor masses, we hypothesize that the central cavity in this GIST could be due to extensive necrosis.
Suppurative gastritis has generally been regarded as a secondary phenomenon caused by the hematogenous spread of bacteria from other infected organs or from a local invasion of the gastric mucosa[13-15]. Alcoholism, diabetes mellitus, decreased gastric acidity and immuno-suppression have been regarded as predisposing factors[16,17]. Suppurative gastritis can be classified as diffuse or localized. A gastric wall abscess is localized and less common, and frequently involves the antrum or pylorus[13]. In order of frequency, Streptococci, Staphylococci, E. coli, Haemophilus influenzae, Proteus and Closttridium are the most common pathogens[18].
This particular case of gastric abscess also contained Streptococcus intermedius. A combination therapy that includes systemic administration of antibiotics and endoscopic drainage of pus has been reported to be an alternative to aggressive surgery[19,20]. Since no organ besides the stomach presented any sign of infection, the abscess in this case might have formed due to bacteria that spread to the adjacent cavity via the fistula. Endoscopic drainage of the abscess and administration of antibiotics resulted in the clinical improvement of this patient. He also was treated with Imanitib mesylate as adjuvant therapy, and no metastasis or recurrence was recognized during the 2-year follow-up period.
Few cases of submucosal tumor accompanied with abscess formation have been reported[21-22]. Recently, following endoscopic biopsy, a giant GIST with abscess formation was reported[21]. This GIST was large (12 cm × 13 cm in diameter) and accompanied with a closed abscess that did not penetrate into the gastric lumen. In 1998, Seidel et al[22] reported a gastric leiomyosarcoma with abscess penetrating into the gastric lumen. This case of submucosal tumor is more similar to our case because spontaneous drainage of pus from the gastric abscess to the lumen was observed endoscopically. Because no immunohistochemical staining for KIT and CD34 was carried out, the case could not clearly be diagnosed as GIST. Hence, this is the first report of a patient with clearly diagnosed GIST accompanied with endoscopic evidence of an abscess penetrating into the gastric lumen.
S- Editor Wang J L- Editor Wang XL E- Editor Che YB