Published online Mar 28, 2007. doi: 10.3748/wjg.v13.i12.1877
Revised: January 20, 2007
Accepted: March 16, 2007
Published online: March 28, 2007
We report an unusual case of primary amyloidosis of the stomach in a patient complaining of dyspeptic symptoms. The diagnosis was confirmed histologically and other gastrointestinal site or systemic involvement was ruled out. Uncharacteristic dyspeptic symptoms may hide this rare metabolic disease.
- Citation: Rotondano G, Salerno R, Cipolletta F, Bianco MA, De Gregorio A, Miele R, Prisco A, Garofano ML, Cipolletta L. Localized amyloidosis of the stomach: A case report. World J Gastroenterol 2007; 13(12): 1877-1878
- URL: https://www.wjgnet.com/1007-9327/full/v13/i12/1877.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i12.1877
The term amyloidosis refers to a group of disorders cha-racterized by the extracellular accumulation of insoluble, fibrillar proteins in various organs and tissues. Amyloidosis commonly shows a systemic involvement. Localised deposition of amyloid is a rather uncommon form, and amyloidal deposit confined to the stomach is extremely rare. The clinical manifestations of gastric amyloidosis are often uncharacteristic and subclinical[1].
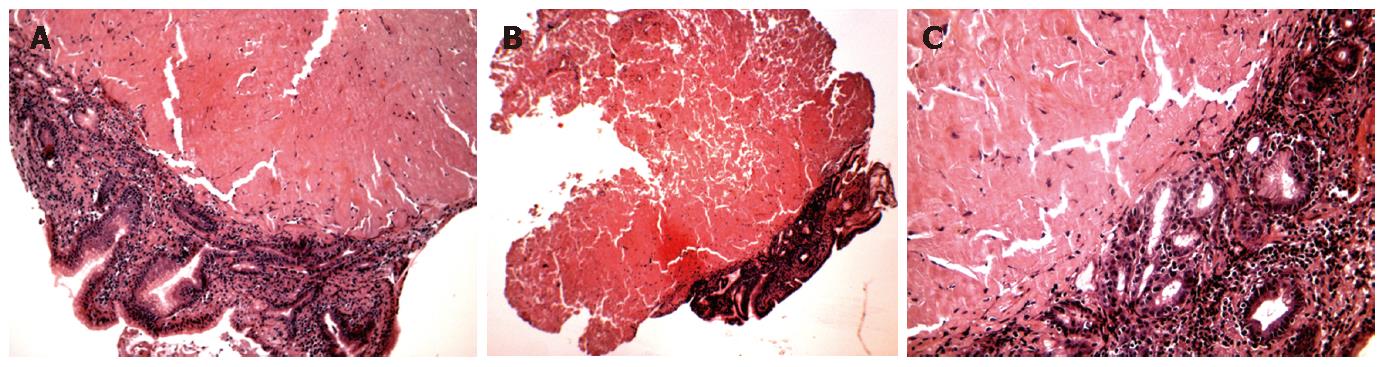
A 55-year old Caucasian male was referred to our open-access Digestive Endoscopy Unit by his family physician due to epigastric pain, heartburn and mild weight loss (< 3 kg). Physical examination showed reduced lower thoracic basis sound, more evident on right side, no wheezes, crackles, or rhonchi. Blood tests and urinalysis were normal. Chest X-rays were normal. Upper gastrointestinal (GI) endoscopy showed two white-yellowish 3-cm circular areas with fine granular appearance on the distal portion of the gastric body and angulus (Figure 1). Histologic examination of biopsy specimens taken at the edges of the lesions showed deposition of fibrillar eosinophilic substance, infiltration of lymphocytes and polyclonal mature plasma cells in the lamina propria, compatible with a pattern of gastric amyloidosis (Figure 2). Endoscopic examination and biopsy samplings of the esophagus, duodenum and rectum excluded other gastrointestinal localizations. Endoscopic ultrasound showed mild thick-ening of the first two layers of the gastric wall with no pathological perigastric or coeliac lymph nodes. The patient was then evaluated in the Centre for the Study of Systemic Amyloidosis of the University of Pavia, where examination of serum, liver, kidney and heart ruled out any multiorgan involvement.
Amyloidosis is a disorder characterized by extracellular deposition of amyloid in various tissues and organs. Common gastrointestinal manifestations include gastro-paresis, constipation, malabsorption, intestinal pseudo-obstruction, and bleeding[2,3]. The absence of systemic sym-ptoms may make diagnosis difficult. Endoscopic findings such fine granular appearance and polypoid protrusions are common and may reflect amyloid deposition in the mucosa or submucosa of the alimentary tract[4].
Localized gastric amyloidosis is an uncommon form of the disease, sometimes associated with gastric ma-lignancies, such as carcinoma and stromal tumours[5,6]. The patient reported herein complained of dyspeptic symptoms, and had isolated gastric involvement without any other gastrointestinal or systemic localizations. Proton pump inhibitors (pantoprazole 40 mg daily per os) were administered as intermittent “on demand” therapy for his dyspeptic complaints, associated with a prokinetic drug (domperidone twice daily before meals). No further treatment was deemed necessary, since the patient was symptoms-free on a clinical follow-up of about 10 mo. Periodic controls have been scheduled to follow the evo-lution of disease and early recognition of multiorgan involvement.
Although gastric amyloidosis is rare, it should be con-sidered among the possible diagnoses in dyspeptic patients and clinical follow-up in specialized centres is warranted in the management of these cases.
| 1. | Deniz K, Sari I, Torun E, Patiroğlu TE. Localized gastric amyloidosis: a case report. Turk J Gastroenterol. 2006;17:116-119. [PubMed] |
| 2. | Lee JG, Wilson JA, Gottfried MR. Gastrointestinal manifestations of amyloidosis. South Med J. 1994;87:243-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Kim H, Jee SR, Lee SB, Lee JH, Park SJ, Park ET, Lee YJ, Lee SH, Seol SY, Chung JM. A case of secondary amyloidosis presenting as massive gastrointestinal bleeding. Korean J Gastroenterol. 2006;47:397-401. [PubMed] |
| 4. | Tada S, Iida M, Iwashita A, Matsui T, Fuchigami T, Yamamoto T, Yao T, Fujishima M. Endoscopic and biopsy findings of the upper digestive tract in patients with amyloidosis. Gastrointest Endosc. 1990;36:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 122] [Article Influence: 3.4] [Reference Citation Analysis (5)] |
| 5. | Bedioui H, Chebbi F, Ayadi S, Ftériche F, Sassi K, Jouini M, Ksantini R, Ammous A, Kacem M, Ben Safta Z. Gastric amyloidosis mimicking malignancy. A case report. Ann Chir. 2006;131:455-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Overstreet K, Barone RM, Robin HS. Secondary amyloidosis and gastrointestinal stromal tumors. A case report and discussion of pathogenesis. Arch Pathol Lab Med. 2003;127:470-473. [PubMed] |
S- Editor Liu Y L- Editor Wang XL E- Editor Liu Y