Published online Nov 21, 2006. doi: 10.3748/wjg.v12.i43.7061
Revised: June 13, 2006
Accepted: June 16, 2006
Published online: November 21, 2006
Retroperitoneal fibrosis (RPF) is a rare condition of unclear etiology. It can cause ureteral obstruction. We present the unique case of a 54 years old female, who initially presented with spontaneous perforation of the cecum. Upon exploring the abdomen, the classical glistening white, unyielding retroperitoneal fibrosis was encountered. A right hemicolectomy was performed. Subsequently, the patient presented with bilateral ureteral obstruction, and later on with small bowel obstruction. Ureteral obstruction was treated with stents, and small bowel obstruction was treated with bypass. To our knowledge no case of idiopathic RPF presenting with features of both bilateral ureteral and small bowel obstruction has been reported in the literature.
- Citation: Aziz F, Conjeevaram S, Phan T. Retroperitoneal fibrosis: A rare cause of both ureteral and small bowel obstruction. World J Gastroenterol 2006; 12(43): 7061-7063
- URL: https://www.wjgnet.com/1007-9327/full/v12/i43/7061.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i43.7061
Retroperitoneal fibrosis (RPF) is a rare condition of unclear etiology. It is believed to be immune-related. About two-thirds of the cases are thought to be idiopathic. We present a case of idiopathic RPF in a 54 years old female who developed bilateral hydronephrosis and then small bowel obstruction due to extrinsic compression from retroperitoneal fibrosis.
To our knowledge no case of idiopathic RPF presenting with features of both bilateral ureteral and small bowel obstruction has been reported in the literature. We recommend early surgical intervention in patients with advanced RPF who are unresponsive to steroids.
A fifty four years old African-American female came to the emergency room with a five-day history of abdominal pain. She described it to be sharp in nature and localized mostly in the middle of the abdomen. She graded pain to be seven on a scale of zero to ten. The pain had no radiation or shifting. The patient also complained of nausea and three episodes of vomiting which was bilious in nature. The patient passed her last bowel movement three days ago and it was normal. She denied fever or shaking chills. Her past medical history was significant for hypertension, type II diabetes mellitus and asthma.
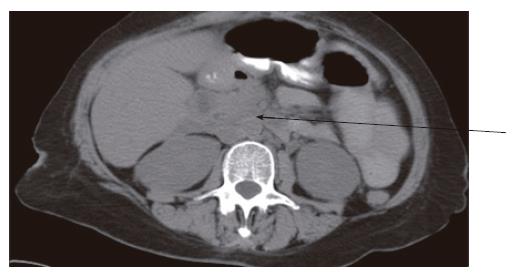
Her past surgical history was significant for laparoscopic cholecystectomy done 6 years ago. On physical examination, she was afebrile and her vital signs were stable. She was awake and alert. She had normal heart sounds, and bilateral breath sounds. Her abdomen was soft, and had generalized and reboud tenderness. Her white blood cell count was 18 000 cells/mm3; the hemoglobin was 14 mg/dL and platelet count was 253 cells/mm3. Her serum chemistry and coagulation tests were normal. Her flat and upright abdominal radiographs were normal. CT of the abdomen and pelvis showed extravasation of oral contrast and inflammation around the ascending colon (Figure 1). She was brought to the operating room and an exploratory laparotomy was performed via a midline incision. On entering the peritoneal cavity, dense intra-abdominal adhesions were encountered at the hepatic flexure. The classical glistening white, unyielding retroperitoneal fibrosis was encountered. The plaque predominantly encased both kidneys. It extended over the renal pelvis and upper ureters on both sides up to the level of aortic bifurcation and encased the great vessels in the midline. A 1 cm × 2 cm perforation was found in the cecum. A right hemicolectomy was performed. Pathology report showed fibrinous adhesions and inflammatory reaction around the site of perforation. No evidence of any tumor was seen. Patient’s post-operative course was uneventful. She started a clear liquid diet on post-operative d 2, and was gradually advanced to a regular diet. The patient was diagnosed with retroperitoneal fibrosis and, hence, received oral steroids. The patient was discharged home on post-operative d 6. She was examined in clinic 4 wk after surgery and reported no complaints.
Three months after surgery, the patient presented to the emergency room with complaints of severe back pain. Her examination was normal. Her laboratory tests were normal. CT scan of the abdomen showed marked hydronephrosis of the right kidney. She underwent cystoscopy which showed narrowing of the right proximal ureter. A stent was placed in the right ureter. The stent was removed 3 wk after placement.
She presented to emergency room after 9 mo with complaints of back pain. Her physical examination and laboratory work was normal. CT of abdomen and pelvis showed bilateral hydronephrosis (Figure 2). A cystoscopy was performed which showed a normal bladder. Retrograde pyelogram showed normal ureters until the proximal part of both ureters, where tortuosity and dilation of the renal pelvis on both sides was noted. Bilateral ureteral stents were placed.
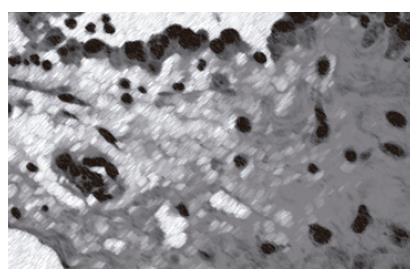
Eight months after bilateral stent placement, she presented to the hospital with complaints of severe abdominal pain. The pain was localized to the middle of the abdomen. It was sharp in intensity and had no radiation and no shifting. The pain was associated with repeated bouts of vomiting. On physical examination, she was afebrile and her vital signs were stable. She was awake and alert. Her abdomen was soft and not distended. She had tenderness in the right upper quadrant. Her white blood cell count was 34 000 cells/mm3, and the hemoglobin was 13 mg/dL. All other laboratory values were in the normal range. Abdominal radiographs showed multiple air fluid levels. CT of her abdomen showed multiple dilated loops of the small bowel and thickening of the bowel wall. Transition point appeared to be somewhere between the jejunum and the ileum. The colon was normal (Figure 3). An exploratory laparotomy was performed through midline incision. On opening the abdomen, the findings were that of severe fibrotic reaction with almost a frozen abdomen on the right lower aspect. Once again, classical glistening white, unyielding retroperitoneal fibrosis was encountered. Careful lysis of adhesions was done and the left upper quadrant was explored, whereby dilated loops of small bowel were found. Lysis of adhesions was attempted in the right lower quadrant but was encountered with enormous amount of bleeding. It was felt that the obstruction was caused by the external compression from retroperitoneal fibrosis. A decision was made to bypass the dilated segment of the jejunum into the colon without interfering with the frozen abdomen on the right side. The ligament of Treitz was identified and the dilated small segment was seen up to about 200 cm of the jejunum. The last portion of jejunum which entered into the frozen part of the abdomen was identified. A 10 cm long segment was anastomosed with the transverse colon which was free of adhesions. Side-to-side anastomosis was done using a GIA-75 and a TA60. Irrigation of the abdomen was carried out. The abdominal cavity was closed. The postoperative course was uneventful. On postoperative d 2, the patient’s nasogastric tube was discontinued. A clear liquid diet was started on postoperative d 3 and was gradually replaced with regular diet. The patient was discharged home on post operative d 9. Pathology report showed fibrinous adhesions and inflammatory reaction (Figure 4).
Classical idiopathic retroperitoneal fibrosis, also known as Ormond’s disease, was described in 1948[1]. The typical retroperitoneal fibrosis is a fibrotic process encasing the abdominal vessels and the ureter with an epicenter at the level of L4-52. RPF has an inciting agent in one-third of the cases, while the remaining two-thirds have no known cause[2].
CT scan of the abdomen is the imaging investigation of choice. Cases with ureteric obstruction can be successfully treated with steroids alone[3], and occasionally with tamoxifen[4], but ureterolysis may still be necessary in advanced or unresponsive cases. This case is unusual because the patient did not respond to oral steroids and had symptomatic ureteral and small bowel obstruction due to retroperitoneal fibrosis. We recommend early surgical intervention in patients with advanced RPF who are unresponsive to steroids.
| 1. | ORMOND JK. Bilateral ureteral obstruction due to envelopment and compression by an inflammatory retroperitoneal process. J Urol. 1948;59:1072-1079. [PubMed] |
| 2. | Resnick MI, Kursh D. Extrinsic obstruction of the ureter. Campbell's Urology, 7th ed. Philadelphia: Saunders 1998; 387-422. |
| 3. | Higgins PM, Bennett-Jones DN, Naish PF, Aber GM. Non-operative management of retroperitoneal fibrosis. Br J Surg. 1988;75:573-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 61] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | al-Musawi D, Mitchenere P, al-Akraa M. Idiopathic retroperitoneal fibrosis treated with tamoxifen only. Br J Urol. 1998;82:442-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
S- Editor Wang J L- Editor Karam SM E- Editor Bi L