Published online Oct 14, 2006. doi: 10.3748/wjg.v12.i38.6229
Revised: July 8, 2006
Accepted: July 18, 2006
Published online: October 14, 2006
We report the case of an 84-year-old female who had a partial gastrectomy with Billroth-II anastomosis 24 years ago for a benign peptic ulcer who now presented an acute pancreatitis secondary to an afferent loop syndrome. The syndrome was caused by a gallstone that migrated through a cholecystoenteric fistula. This is the first description in the literature of a biliary stone causing afferent loop syndrome.
- Citation: Dias AR, Lopes RI. Biliary stone causing afferent loop syndrome and pancreatitis. World J Gastroenterol 2006; 12(38): 6229-6231
- URL: https://www.wjgnet.com/1007-9327/full/v12/i38/6229.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i38.6229
The afferent loop syndrome is a mechanical obstruction that impairs the clearance of bile and pancreatic juices from the afferent jejunal loop of a gastrojejunostomy. Entrapment of the afferent loop by postoperative adhesions, internal hernias, loop kinking at the gastrojejunostomy, intestinal volvulus, intussusception, anastomotic cancer, enteroliths and bezoars have all been incriminated as causes. A cholecystoenteric fistula with biliary stone impactation in the anastomosis as a cause has never been reported, as far as we know.
An 84-year-old female presented in the emergency room with severe right upper quadrant pain and vomiting in the last 8 h. She referred cholecystolithiasis with infrequent episodes of pain; the last one extended for 6 d and ended 4 d ago, being longer and more severe than usual. She brought a previous abdominal sonography showing a single stone of 1.5 cm in the gallbladder.
Her past history included diabetes mellitus and a partial gastrectomy with a Billroth II reconstruction for benign peptic ulcer 24 years ago. On physical examination the patient reported intense pain in the superior half of the abdomen. Vital signs were stable. Laboratory exams showed mild leukocytosis and acute pancreatitis.
An abdominal sonography was performed and demonstrated air inside the gallbladder associated with a dilatation of the afferent jejunal loop, suggesting a gallstone ileus as a possible cause for the bowel distension.
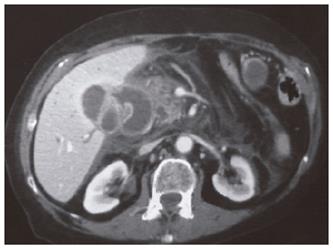
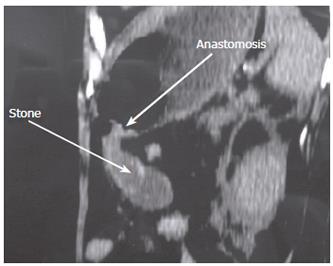
A computed tomography was then performed and revealed an afferent loop syndrome due to a stone impacted in the gastrojejunal anastomosis. Pancreatitis was also observed (Figure 1, Figure 2, Figure 3, Figure 4).
A few hours after the admission the patient presented hypotension and a decline in her mental status requiring orotracheal intubation and vasopressors. She was then transfered to an intensive care unit.
An upper digestive endoscopy was performed and successfully removed the stone with a basket (Figure 5). During the following two days her white blood cell count increased, her renal and liver functions declined and the vasopressors were progressively augmented. She also presented an abdominal compartiment syndrome on the second day being submitted to a decompressive laparotomy. During the laparotomy adhesions were observed between the afferent loop and the gallbladder.
On the third day the patient presented a cardiac arrest and died.
The afferent loop syndrome results from the obstruction of the afferent jejunal loop of a gastrojejunostomy. Its acute form usually occurs in the early postoperative period but it can occur decades after the surgery having a devastating course unless promptly treated[1-4].
There are various causes of the afferent loop syndrome. Adhesions, volvulus, intussusception are some of the most common while enteroliths, cancer and bezoars are some of the rarest[1-7]. This is the first report in the literature of a biliary stone causing the syndrome (Pubmed, Medscape, Cochrane database and Scielo database were systematically reviewed).
The pain reported by the patient 4 d before the admission might have been an acute cholecystitis that led to the formation of a cholecystoenteric fistula, allowing the biliary stone to ingress the afferent loop and ultimately stop in the anastomosis causing the obstruction.
Concerning the acute pancreatitis it is an uncommon and agressive manifestation of the afferent loop syndrome with few cases found in the literature. The transmission of high pressures back to the biliopancreatic ductal system leading to duodenopancreatic reflux seems to play an important role in its pathogenesis. An experimental model of “closed duodenal loop” can simulate this clinical situation[4,6,8].
Regarding the management of the obstruction, the choice to perform a gastrointestinal endoscopy was based on the patient’s vital signs that were quickly declining. In fact this is a rapid procedure, with low risk of complications, far less aggressive than a laparotomy and it has already been successfully used to remove gallstones occluding the upper digestive tract[9,10]. Percutaneous drainage is also a conservative option[11]. Either way surgical lithotomy can always be performed, even as a last resource when the other options failed[12].
Although the obstruction was rapidly resolved and the measures for severe pancreatitis were quickly introduced the multiple organ disfunction was already installed. The patient’s age and the diabetes also contributed to the outcome.
| 1. | Bushkin FL, Woodward ER. The afferent loop syndrome. Major Probl Clin Surg. 1976;20:34-48. [PubMed] |
| 2. | Carbognin G, Biasiutti C, El-Khaldi M, Ceratti S, Procacci C. Afferent loop syndrome presenting as enterolith after Billroth II subtotal gastrectomy: a case report. Abdom Imaging. 2000;25:129-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Sarli L, Iusco D, Violi V, Roncoroni L. Enterolith ileus complicating afferent loop syndrome simulating acute pancreatitis. Int Surg. 2003;88:129-132. [PubMed] |
| 4. | Kaya E, Senyürek G, Dervisoglu A, Danaci M, Kesim M. Acute pancreatitis caused by afferent loop herniation after Billroth II gastrectomy: report of a case and review of the literature. Hepatogastroenterology. 2004;51:606-608. [PubMed] |
| 5. | Tien YW, Lee PH, Chang KJ. Enterolith: an unusual cause of afferent loop obstruction. Am J Gastroenterol. 1999;94:1391-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Mann NS, Rachut E. Carcinoma of gastric stump causing afferent loop obstruction and acute pancreatitis. Hepatogastroenterology. 2004;51:184-185. [PubMed] |
| 7. | Hui MS, Perng HL, Choi WM, Chem LK, Yang KC, Chen TJ. Afferent loop syndrome complicated by a duodenal phytobezoar after Billroth-II subtotal gastrectomy. Am J Gastroenterol. 1997;92:1550-1552. [PubMed] |
| 8. | Ratia Giménez T, Escribano Vera J, Vicent Granell J, Lomas Espadas M. [Acute pancreatitis and afferent loop syndrome]. Rev Esp Enferm Dig. 1991;80:61-64. [PubMed] |
| 9. | Lübbers H, Mahlke R, Lankisch PG. Gallstone ileus: endoscopic removal of a gallstone obstructing the upper jejunum. J Intern Med. 1999;246:593-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | López Rosés L, Toscano J, Iñiguez F, Santos E, Pérez Carnero A. [Successful endoscopic therapy in a case of Bouveret's syndrome]. Rev Esp Enferm Dig. 1994;85:483-485. [PubMed] |
| 11. | Kitamura H, Miwa S, Nakata T, Nomura K, Tanaka T, Ikegami T, Miyagawa S, Kawasaki S. Sonographic detection of visceral adhesion in percutaneous drainage of afferent-loop small-intestine obstruction. J Clin Ultrasound. 2000;28:133-136. [PubMed] [DOI] [Full Text] |
| 12. | Gencosmanoglu R, Inceoglu R, Baysal C, Akansel S, Tozun N. Bouveret's syndrome complicated by a distal gallstone ileus. World J Gastroenterol. 2003;9:2873-2875. [PubMed] |
S- Editor Wang J L- Editor Zhu LH E- Editor Liu WF