CASE REPORT
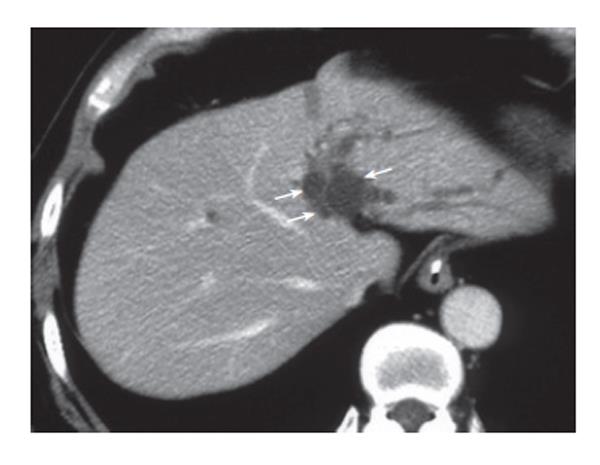
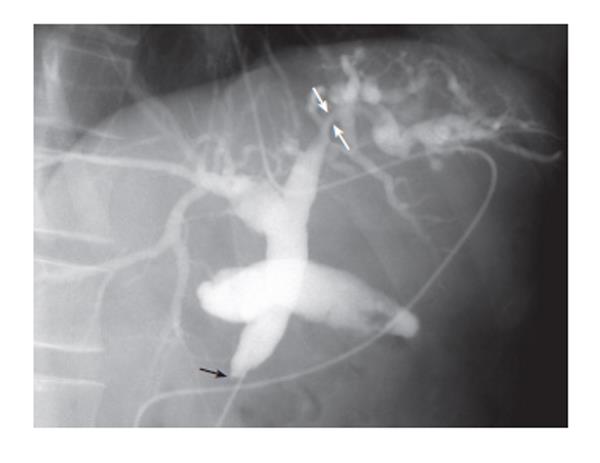
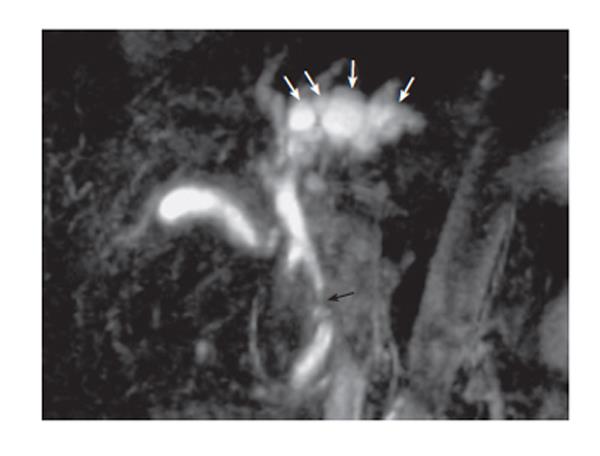
A 54-year-old Japanese man was admitted to a local hospital for complaints of jaundice. He was diagnosed with lower bile duct carcinoma and referred to our hospital after placement of endoscopic naso-biliary drainage. He had a history of heavy alcohol use and had been hospitalized for one year with alcoholism ten years previously. Physical examination results were generally unremarkable. The liver was palpable two fingerbreadths below the right costal margin. No ascites or edema was present. Laboratory examination revealed a normal complete blood count and normal coagulation. Liver function test results at admission to our hospital were as follows: aspartate aminotransferase (AST), 75 U/I; alanine aminotransferase (ALT), 133 U/I; alkaline phosphatase (ALP), 467 U; γ-glutamyl transpeptidase (GTP), 196 U/I; total bilirubin, 1.1 mg/mL; indocyanine green test (at 15 min), 6.2%. Hepatits virus screening was negative and no tumor markers were elevated. Abdominal ultrasonography revealed multiple small cystic lesions and tubular anechoic areas along the umbilical portion of the portal vein that were difficult to differentiate with dilatation of the intrahepatic bile ducts. CT revealed a tumor in the lower bile duct and multiple small cystic lesions along the umbilical portion of the portal vein (Figure 1). Cholangiography via an endoscopic naso-biliary drainage tube revealed complete obstruction of the lower bile duct, smooth stenosis of the left hepatic duct, and a slight dilatation of the intrahepatic bile duct in the left lobe (Figure 2). Magnetic resonance cholangiopancreatography (MRCP) showed bead-like cystic lesions along the biliary tree in the left lobe of the liver (Figure 3). The left hepatic duct stenosis appeared to be caused by extramural compression by these cysts. Portal phase superior mesenteric arteriography and hepatic arteriography demonstrated no particular abnormalities. Based on these imaging studies, he was diagnosed as having lower bile duct carcinoma and peribiliary cysts. He underwent pylorus preserving pancreatoduodenectomy. As for the peribiliary cysts, a course of observation was decided upon. The carcinoma was a nodal infiltrating-type tumor sized 12 mm × 8 mm existing in the lower bile duct.
Figure 1 CT revealing multiple small cystic lesions along the umbilical portion of the portal vein (arrows).
Figure 2 Cholangiogram via endoscopic naso-biliary drainage tube revealing complete obstruction in the lower bile duct (black arrow) and smooth stenosis of the left hepatic duct (white arrows) and a slight dilatation of the intrahepatic bile duct in the left lobe.
Figure 3 Magnetic resonance cholangiopancreatogram showing bead-like cystic lesions (arrows) along the biliary tree in the left lobe of the liver.
The tumor was histopathologically diagnosed as a moderately differentiated tubular adenocarcinoma, pT3, pN0, pM0 and stage IIA[3]. After the operation, minor leakage of the pancreatojejunostomy developed and was successfully treated by conservative therapy. He is alive without recurrence and symptoms 10 mo after surgery at this writing.
DISCUSSION
Peribiliary cysts were first reported by Nakanuma et al in 1984[4]. They speculated that the peribiliary cysts arose from cystic dilatation of the intrahepatic extramural peribiliary glands in the periductal connective tissue[4]. A systematic study of autopsied livers disclosed that the disease is not uncommon; cystic changes of the peribiliary glands were found in 202 livers (20.2%) among 1000 consecutive autopsy livers[1]. However, since the degree of cystic dilatation is quite variable, and the majority are recognizable microscopically, this disease is still poorly recognized in clinical practice[5]. The precise mechanism for cystic dilatations of intrahepatic peribiliary glands is unclear. Peribiliary cysts are usually detectable in pre-existing hepatobiliary diseases such as liver cirrhosis, idiopathic portal hypertension, portal vein thrombosis, alcoholic liver disease, and adult-type polycystic kidney disease[4,6,7]. Therefore, it has been speculated that circulation failure caused by the interference of blood flow through the portal vein causes morphological changes of extramural glands around the bile duct. Nakanuma presumed that, in cases of adult-type polycystic kidney disease, gene expression in the intrahepatic peribiliary glands related to this disease may lead to the formation of peribiliary cysts[5]. In the case reported here, alcoholic liver injury did not develop into liver cirrhosis, and there were no findings of portal hypertension. Peribiliary cysts are also known to develop in patients with cystic dilatation of the intrahepatic biliary system after hepatic portoenterostomy[8]. We speculate that in the case reported here, cholestasia due to lower bile duct cancer, in addition to alcoholic liver disease, might be related to the development of peribiliacy cysts. However, whether peribiliary cysts existed before the development of bile duct cancer is uncertain, since he had not undergone diagnostic imaging before the onset of obstructive jaundice.
On diagnostic imaging, peribiliary cysts are characterized as clusters of relatively small multiple cystic lesions developing around the hepatic hilum and large branches of the portal vein, but not in liver parenchyma[9]. Recently, MRCP has been reported to be useful in the diagnosis of peribiliary cysts. MRCP clearly depicts multiple cysts as a string of bead-like structures or a foamy fringe along the hepatic hilum or larger bile ducts. Drip infusion cholangiographic (DIC) CT is also useful for diagnosing peribiliary cysts. On DIC-CT, peribiliary cysts are not filled with contrast material since these cysts do not communicate with the lumen of the biliary tree.
Peribiliary cysts have usually been considered to be clinically harmless. There are two reports describing obstructive jaundice secondary to the obstruction of bile ducts by peribiliary cysts[2,10]. It is thought that surgery is not indicated for asymptomatic peribiliary cysts but they should be followed up[9,11]. Misdiagnosis of peribiliary cysts as intrahepatic cholangiocarcinoma is a possibility[2,12,13], and there are two reports concerning such patients undergoing hepatectomy on suspicion of intrahepatic cholangiocarcinoma[12,13]. Precise diagnosis can be obtained easily by characteristic findings with diagnostic imaging if the attending clinician is knowledgeable about peribiliary cysts. Needless to say, unnecessary operations for patients with peribiliary cysts should be avoided.
There have been no reports of peribiliary cysts accompanying bile duct carcinoma. If knowledge of the clinical entity of peribiliary cysts becomes widespread, the number of patients with peribiliary cysts accompanying biliary malignancy is sure to increase. When peribiliary cysts and biliary malignancy exist simultaneously, the operative procedure should be chosen according to the staging and extension of the malignancy as well as the positional relationship between the two lesions based on proper diagnosis. We chose not to select surgical therapy for the peribiliary cysts, on the basis that we diagnosed the stricture of the left hepatic duct as compression by peribiliary cysts, and hepatopancreatoduodenectomy, an indispensable procedure for resecting both the lower bile duct cancer and stricture of left hepatic duct, by itself is associated with high rates of postoperative complications and operative mortality[14]. Over-surgery due to misdiagnosis for patients with biliary malignancy accompanied by peribiliary cysts should be avoided. However, peribiliary cysts have been reported to become gradually enlarged and increased in number in some cases[15,16]. Long-term follow-up is obviously called for.